Abstract
Purpose:
To determine whether the type of health insurance a patient possesses and a patient’s race affects receipt of common tests to monitor open-angle glaucoma (OAG).
Design:
Retrospective longitudinal cohort study.
Participants:
21766 persons age ≥40 years old with newly-diagnosed OAG between 2007-2011 enrolled in Medicaid or a large United States managed care network.
Methods:
We determined the proportion of patients with newly-diagnosed OAG who underwent visual field (VF) testing, fundus photography (FP), other ocular imaging (OOI), or none of these tests within the first 15 months after initial OAG diagnosis. Multivariable logistic regression was used to assess the extent by which health insurance type and race/ethnicity affected the odds of undergoing glaucoma testing.
Main Outcome Measures:
Odds ratios (OR) of undergoing VF testing, FP, OOI, or none of these tests in the 15 months after initial OAG diagnosis with 95% confidence intervals (CI)
Results:
18372 persons with commercial health insurance and 3394 Medicaid recipients met the study inclusion criteria. The proportions of persons with commercial health insurance with newly-diagnosed OAG who underwent VF, FP, and OOI were 63%, 22%, and 54%, respectively, while the proportions were 35%, 19%, and 30%, respectively, for Medicaid recipients. Compared to those with commercial health insurance, Medicaid recipients were 234% more likely to not receive any glaucoma testing in the 15 months following initial diagnosis (OR=3.34, CI:3.07-3.63). After adjustment for confounders, whites with OAG enrolled in Medicaid had 198% higher odds of receiving no glaucoma testing compared with whites possessing commercial health insurance (OR=2.98, CI:2.66-3.33). Blacks with Medicaid insurance demonstrated 291% higher odds (OR=3.91, CI:3.40-4.49) of not receiving any glaucoma testing compared to blacks with commercial health insurance.
Conclusions:
Irrespective of race/ethnicity, Medicaid recipients with OAG are receiving substantially less glaucoma testing compared to persons with commercial health insurance. Disparities in testing are observed across all races/ethnicities but were most notable for blacks. These findings are particularly disconcerting since blacks are more likely than whites to go blind from OAG and there are disproportionately more blacks in Medicaid. Efforts are needed to improve the quality of glaucoma care for Medicaid recipients, especially racial minorities.
Précis:
Medicaid recipients with newly-diagnosed open-angle glaucoma are substantially less likely to undergo testing to monitor for disease progression compared with those with commercial health insurance. These disparities are most prominent for racial minorities.
Introduction
Open angle glaucoma (OAG) disproportionately affects racial minorities, including blacks, Latinos, and Asian Americans.1–5 Compared to whites, racial minorities are also more likely to develop vision loss and experience blindness from OAG.6–8 Despite the higher prevalence of OAG and greater disease burden on racial minorities, past studies have demonstrated substantial gaps in the monitoring of racial minorities with OAG to assess for disease progression9 and prior research found that fewer racial minorities than expected receive treatment for this sight-threatening disease.10 Past studies comparing glaucoma care by race have focused on groups of patients with Medicare or commercial health insurance.1–4,9,10 To the best of our knowledge, researchers have yet to assess for disparities in glaucoma care among socioeconomically disadvantaged persons such as those who are enrolled in Medicaid compared to those with other types of health insurance.
Medicaid is the largest health insurer for low income individuals, covering nearly 70 million Americans which is approximately 15% of all persons in the US who have health insurance.11 With the passage of the Patient Protection and Affordable Care Act (PPACA), the number of Medicaid beneficiaries has increased in recent years.12 Although little is known regarding utilization of glaucoma care services among those with Medicaid relative to persons with other forms of health insurance, past studies have compared utilization of other health care services, such as mammograms, Papanicolaou smears and prostate-specific antigen tests to check for cancer have demonstrated that Medicaid recipients receive fewer of these screening tests than persons with other types of health insurance.13,14 Likewise, Medicaid recipients tend to have worse health outcomes such as lower survival rates from lymphoma15, lower resection rates and higher mortality rates due to liver metastases from colorectal cancer16, and receive fewer surgical interventions for resectable pancreatic cancer compared to those with other insurance types.17
The purpose of this study is to compare Medicaid recipients who were newly-diagnosed with OAG to others with commercial health insurance and to determine whether the type of health insurance a patient possesses affects the likelihood of undergoing testing to monitor for disease progression, as recommended by the American Academy of Ophthalmology’s (AAO) Preferred Practice Pattern guidelines.18 Moreover, we sought to learn whether racial disparities in glaucoma management documented previously for persons with other forms of health insurance also exist for patients enrolled in Medicaid, and if so, whether there are greater or fewer disparities in glaucoma care for whites, blacks, and Latinos with Medicaid versus enrollees of the same race who possess commercial health insurance.
Methods
Data Sources
Data for these analyses came from two sources, the Medicaid Analytic Extract (MAX) and the Clinformatics DataMart (Optumlnsight, Eden Prairie, MN) databases.
Medicaid Analytic Extract
The MAX database contains de-identified health care claims data for persons in all 50 state-run Medicaid programs and Washington D.C. Researchers have used the Medicaid MAX dataset to study health care service utilization and outcomes of Medicaid recipients for other conditions.19,20 For each enrollee, we had access to all medical claims for ocular and non-ocular conditions, as identified based on International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) billing codes21, and all visits, diagnostic, and therapeutic procedures as identified based on Current Procedural Terminology22, 4th Edition and Healthcare Common Procedure Coding System (CPT-4®/HCPCS) billing codes from January 1, 2005 to December 31, 2012. In addition, the Personal Summary file has data on date of birth, sex, race/ethnicity, number of months of Medicaid eligibility in a given year, and most recent 5-digit ZIP code of residence for each enrollee.
Clinformatics DataMart Database
The Clinformatics DataMart database contains detailed de-identified records of enrollees in a large U.S. managed-care network. The data available include beneficiaries receiving any form of eye care from January 1, 2001, through December 31, 2014. To make the data comparable to those with Medicaid, we restricted our analyses to data from 2005-2012. This subset of beneficiaries had ≥1 ICD-9-CM codes for any eye-related diagnosis (360-379.9) or CPT-4 code for any eye-related visits, diagnostic or therapeutic procedures (65091-68899 or 92002-92499), or any other claims submitted by an ophthalmologist or optometrist during the beneficiary’s time in the medical plan. Similar to data from MAX, the Clinformatics DataMart contains information on medical claims for all ocular and non-ocular conditions and demographic information (age, sex, race/ethnicity) for each enrollee. Both datasets also contained information on the types of health care providers performing the services. The data from both sources were de-identified prior to our licensing it and the study was approved by the University of Michigan Institutional Review Board.
Participant Selection
We identified white, black, and Hispanic/Latino enrollees age ≥ 40 years in both datasets who had OAG diagnoses (ICD-9-CM codes 365.1, 365.10, 365.11, 365.12, and 365.15). As the objective was to evaluate diagnostic testing among those with newly-diagnosed OAG, enrollees with pre-existing OAG diagnosis identified during a two year look-back period were excluded. We also required ≥1 confirmatory OAG diagnosis on a later date to help assure the enrollees were not simply miscoded on 1 visit with this condition. Enrollees who were not continuously enrolled in each respective plan for at least 39 consecutive months (24 months prior to the initial OAG diagnosis and 15 months afterwards) were excluded since they may have undergone testing during the times they were not enrolled in the plan. Medicaid enrollees with dual enrollment in Medicare or with managed care were excluded. Those with other forms of glaucoma and glaucoma suspects were not included in these analyses.
Receipt of Glaucoma Testing
The outcome of interest was receipt of visual field (VF) testing (CPT 92081, 92082, and 92083), fundus photography (FP) (CPT 92250), or other ocular imaging (OOI) (CPT 92133, 92135) during the 15 months after initial OAG diagnosis. Other ocular imaging includes ocular coherence tomography (OCT), confocal scanning laser ophthalmoscopy (CSLO), and scanning laser polarimetry (SLP). The AAO Preferred Practice Patterns guidelines for primary OAG recommend receipt of perimetry and careful evaluation of the optic nerve at least once every 12 months.18 As others have done previously23, we added 3 additional months to account for enrollees who may have needed to reschedule their annual appointments to provide ample time for testing to take place. This 15-month period did not include the date of initial OAG diagnosis.
Analyses
Statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, NC) and R, version 3.3.1 (R Foundation for Statistical Computing, Vienna, Austria). Enrollees’ characteristics were summarized for the entire sample using frequencies and percentages for categorical variables and means and standard deviations (SD) for continuous variables. The proportion of enrollees undergoing ≥ 1 of a given diagnostic test (or no testing of any type) in the 15 months after initial OAG diagnosis was determined for enrollees in the two insurance plans. Comparisons of these proportions were performed using the Pearson’s chi-square test. For those who had no record of any glaucoma testing, we checked to determine what proportion had and did not have visits to eye care professionals (ophthalmologist or optometrist) during that 15 month time period.
Multivariable Logistic Regression
Multivariable logistic regression models were created to determine patient-level factors affecting the odds of undergoing each type of glaucoma test (or no testing of any type) in the 15 month time interval after the initial OAG diagnosis. The primary patient-level covariates of interest in the model were insurance type (Medicaid versus commercial) and race/ethnicity (white, black, or Latino/Hispanic). Other covariates included in the models as main effects were age at initial OAG diagnosis, calendar year of initial OAG diagnosis, sex, comorbid ocular diseases including age-related macular degeneration, cataract, macular edema, other conditions affecting the optic nerve that could warrant one of these tests, and other retinal conditions that could warrant OOI or FP testing, and medical comorbidities such as diabetes, hyperlipidemia, and systemic hypertension. Models were fit with and without an interaction term between race and insurance type to estimate the effect of race on the relationship between insurance type and glaucoma testing. The regression models generated odds ratios (OR) with 95% confidence intervals (CI). For all analyses, p<0.05 was considered statistically significant.
Results
Study sample
There were 3394 Medicaid recipients and 18372 persons with commercial health insurance who met the study inclusion criteria. Patients with Medicaid were, on average, younger in mean ± SD age at initial OAG diagnosis (56±7 years versus 63±11 years). A greater proportion of those in Medicaid were black (40.7% vs. 17.4%) and Hispanic/Latino (10.2% vs. 7.7%) (p<0.001 for both) and there was a greater proportion of females in Medicaid (59.3% vs. 53.6%) compared to commercial health insurance (p<0.001). (Table 1)
Table 1.
Demographic Characteristics of Enrollees with Medicaid and Commercial Health Insurance
| Medicaid | Commercial | |||
|---|---|---|---|---|
| Eligible, n | 3394 | 18372 | ||
| Mean / SD age at initial diagnosis | 56 | 7.3 | 63 | 11.4 |
| Age, n (%) | ||||
| 40-49 | 733 | 21.6 | 1996 | 10.9 |
| 50-59 | 1579 | 46.5 | 5318 | 29.0 |
| 60-69 | 1025 | 30.2 | 6019 | 32.8 |
| 70+ | 57 | 1.7 | 2592 | 27.4 |
| Sex, n (%) | ||||
| Female | 2011 | 59.3 | 9848 | 53.6 |
| Race, n (%) | ||||
| White | 1666 | 49.1 | 13764 | 74.9 |
| Black | 1382 | 40.7 | 3201 | 17.4 |
| Latino | 346 | 10.2 | 1407 | 7.7 |
SD= standard deviation
Rates of Glaucoma Testing
The proportion of enrollees in Medicaid who underwent VF testing at least once in the 15 months after initial OAG diagnosis was substantially lower compared to those with commercial health insurance (35.2% vs. 63.1%, respectively) (p<0.001). Likewise, the proportion of Medicaid beneficiaries who received OOI in the 15 months following initial diagnosis was much lower than those with commercial health insurance (29.8% versus 53.7%, respectively) (p<0.001). The proportion of Medicaid recipients who underwent FP within the first 15 months after initial OAG diagnosis (18.8%) was relatively similar to, though statistically significantly less than, those with commercial health insurance (22.3%) (p<0.001). Almost half of all Medicaid recipients with OAG (48.6%) had no record of any of the 3 glaucoma tests in the first 15 months after initial OAG diagnosis. By comparison, for those with commercial health insurance, 21.5% had no record of receipt of any of these tests during that same time period (p<0.001) (Figure 1). Among persons with commercial health insurance who had no record of any glaucoma testing, 84% had at least one record of an office visit to an eye care provider during that 15 month period. In Medicaid, the corresponding proportion was 62%.
Figure 1: Proportion of Enrollees with Medicaid and Commercial Health Insurance Who Underwent Glaucoma Testing in the 15 Months After Incident Open Angle Glaucoma Diagnosis.
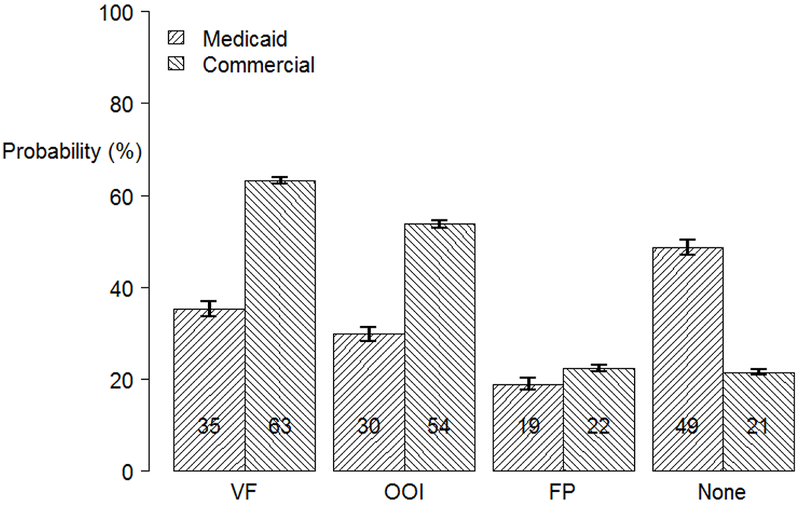
VF = Visual field; FP = Fundus photography; OOI = Other ocular imaging
Multivariable Logistic Regression Models
Visual Field Testing
In an multivariable adjusted logistic regression model, enrollees with Medicaid insurance had a 67% decreased odds of receiving VF testing compared to those with commercial health insurance (OR=0.33, 95% CI:0.31-0.36). Allowing for an interaction between health insurance type and race, whites with Medicaid insurance had a 63% decreased odds (OR=0.37, CI:0.33-0.42) of VF testing compared to whites with commercial health insurance, blacks with Medicaid had a 73% decreased odds (OR=0.27, CI:0.23-0.31) of undergoing VF testing compared to blacks with commercial health insurance, and Latinos/Hispanics in Medicaid had a 52% decreased odds (OR=0.48, CI:0.37-0.61) of VF testing relative to Latinos/Hispanics with commercial health insurance (Figure 2). These odds ratios were statistically significantly different from one another (p<0.0001).
Figure 2: Comparison of the Odds of Receiving Each Glaucoma Test in the 15 Months After Incident Open Angle Glaucoma Diagnosis for Medicaid and Commercial Health Insurance Enrollees, Overall and Stratified by Race.
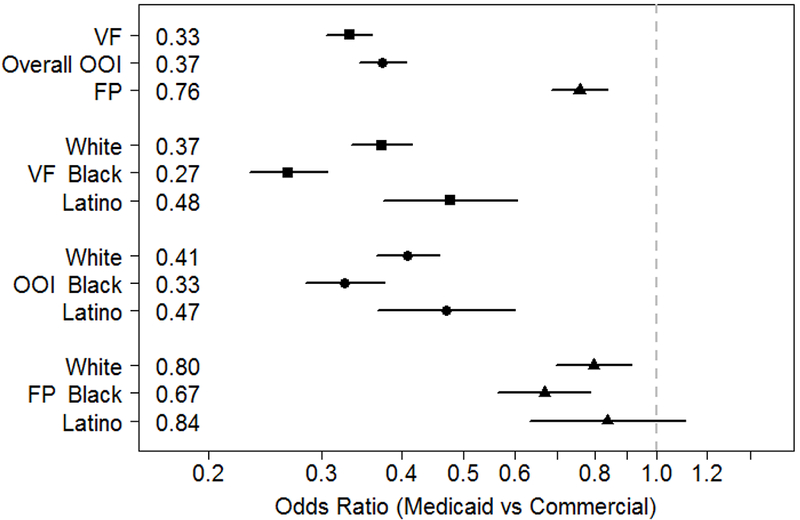
Model adjusted for potential confounders including age at initial OAG diagnosis, calendar year of initial OAG diagnosis, sex, comorbid ocular diseases including age-related macular degeneration, cataract, macular edema, other conditions affecting the optic nerve that could warrant one of these 3 tests, and other retinal conditions that could warrant FP or OOI testing and medical comorbidities such as diabetes, hyperlipidemia, and systemic hypertension.
VF = Visual field; FP = Fundus photography; OOI = Other ocular imaging
Fundus Photography
In the multivariable adjusted logistic regression model, Medicaid recipients had a 24% decreased odds of undergoing FP compared to those with commercial health insurance (OR = 0.76, CI:0.69-0.84). Allowing for an interaction between insurance type and race, whites with Medicaid had a 20% decreased odds (OR=0.80, CI:0.70-0.91) of FP testing compared to whites with commercial health insurance, blacks with Medicaid insurance had a 33% decreased odds (OR=0.67, CI:0.57-0.79) of undergoing FP testing compared to blacks with commercial health insurance, but Latinos/Hispanics did not have a statistically significant difference (OR=0.84, CI:0.63-1.11) in odds of receiving FP between the two health insurance types (Figure 2). These odds ratios were not statistically significantly different from one another (p=0.19).
Other Ocular Imaging
In the multivariable adjusted regression model, beneficiaries with Medicaid had a 63% decreased odds of receiving OOI (OR=0.37, CI:0.34-0.41) compared to enrollees with commercial health insurance. Allowing for an interaction between insurance type and race, whites with Medicaid insurance had a 59% decreased odds (OR=0.41, CI:0.37-0.46) of undergoing OOI testing compared to whites with commercial health insurance, blacks with Medicaid insurance had a 67% decreased odds (OR=0.33, CI:0.28-0.38) of undergoing OOI testing compared to blacks with commercial health insurance, and Latinos/Hispanics in Medicaid had a 53% decreased odds (OR=0.47, CI:0.37-0.60) of OOI testing relative to Latinos/Hispanics with commercial health insurance (Figure 2). These odds ratios were statistically significantly different from one another (p=0.012).
No Record of Any Glaucoma Testing
Table 2 shows the number of beneficiaries of different races/ethnicities who had no record of any glaucoma testing in the 15 months after initial OAG diagnosis for persons with the 2 insurance types. In the multivariable regression model, Medicaid enrollees had a 234% increased odds (OR=3.34, CI:3.07-3.63) of not receiving any glaucoma testing in the 15 months after initial OAG diagnosis compared to those with commercial health insurance. These differences were notable for all 3 race/ethnicity groups but most apparent among blacks. Blacks in Medicaid had a 291% increased odds (OR=3.91, CI:3.40-4.49) of not receiving any glaucoma testing compared to blacks with commercial health insurance. Latinos/Hispanics in Medicaid had a 167% increased odds (OR=2.67, CI:2.07-3.43) of not undergoing any testing compared to those with commercial health insurance. Likewise, whites in Medicaid had a 198% increased odds (OR=2.98, CI:2.66-3.33) of not undergoing any glaucoma testing compared to whites with commercial health insurance (Figure 3). These odds ratios were statistically significantly different from one another (p<0.0023).
Table 2:
Numbers of Beneficiaries with Incident Glaucoma who Undergo No Testing in the 15 Months After Initial Diagnosis
| Commercial | Medicaid | |||
|---|---|---|---|---|
| White | 2908/13764 | (21%) | 748/1666 | (45%) |
| Black | 742/3201 | (23%) | 755/1382 | (55%) |
| Latino | 397/1407 | (21%) | 147/346 | (42%) |
| All | 3947/18372 | (21%) | 1650/3994 | (49%) |
Figure 3: Comparison of the Odds of Undergoing No Glaucoma Testing in the 15 Months After Incident Open Angle Glaucoma Diagnosis for Medicaid and Commercial Health Insurance Enrollees.
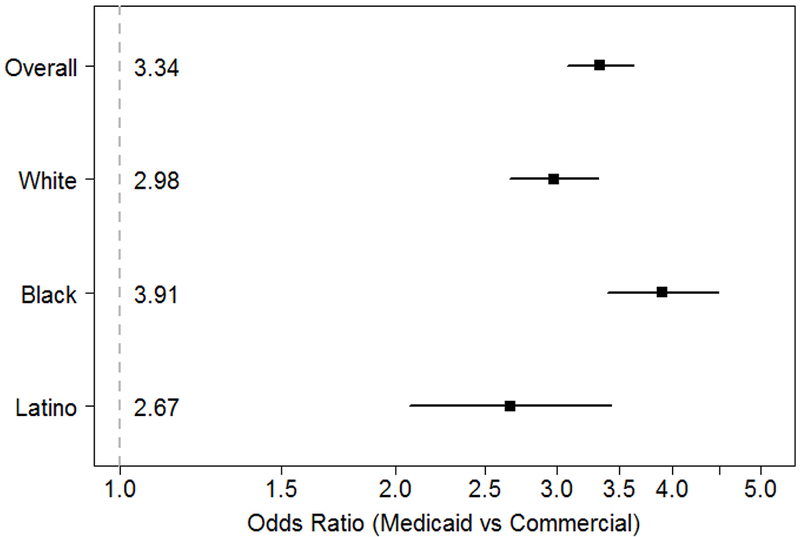
Model adjusted for potential confounders including age at initial OAG diagnosis, calendar year of initial OAG diagnosis, sex, comorbid ocular diseases including age-related macular degeneration, cataract, macular edema, other conditions affecting the optic nerve that could warrant one of these 3 tests, and other retinal conditions that could warrant FP or OOI testing and medical comorbidities such as diabetes, hyperlipidemia, and systemic hypertension.
VF = Visual field; FP = Fundus photography; OOI = Other ocular imaging
In a sensitivity analysis, we adjusted each of the 4 above-mentioned regression models for whether the enrollee lived in an urban or rural residential community and there was no substantive change in the results with the addition of this covariate to each model.
Discussion
We followed a large cohort of patients with newly-diagnosed OAG to determine the extent by which differences in type of health insurance a patient possesses affected utilization of tests that are routinely performed to monitor for OAG progression. We learned that compared to patients with commercial health insurance, those covered by Medicaid were substantially less likely to receive glaucoma testing of all types in the 15 months following initial diagnosis. In fact, nearly half of all patients with OAG with Medicaid insurance (49%) had no record of any glaucoma testing in the first 15 months following their initial diagnosis, while only 1 in 5 (21%) patients with commercial health insurance had no record of any glaucoma testing. These differences in utilization of testing among Medicaid enrollees and those with commercial insurance were observed for whites, blacks, and Latinos/Hispanics. The odds of receiving no glaucoma testing among patients in Medicaid were 198%, 291%, and 167% higher for whites, blacks, and Latinos/Hispanics, respectively, compared to their counterparts with commercial health insurance. The findings of these analyses raise serious concerns regarding the quality of glaucoma care received by Medicaid recipients.
Prior research has established that racial disparities exist in the use of testing to monitor patients with OAG. For example, using data on patients enrolled in Medicare from 1995 to 1999, Coleman and colleagues reported that blacks with OAG had a 7% lower rate of undergoing VF testing in the year prior to glaucoma surgery compared to whites.10 Using claims data from 2001 to 2009, our group previously compared utilization of glaucoma testing among a cohort of enrollees newly-diagnosed with OAG with commercial health insurance and found few differences in diagnostic testing among white and black patients but a considerably lower odds of testing among Latinos compared with whites.9 While our prior study adjusted for sociodemographic factors such as patient income and education level, all of the enrollees had the same form of health insurance. To our knowledge, the present analysis is the first to directly compare utilization of glaucoma testing for patients with two different types of health insurance. Our study findings suggest that the type of health insurance coverage a patient possesses— which, in this case may be a surrogate for annual income— appears to have an even greater effect on utilization of glaucoma testing than does race/ethnicity.
The large majority of study participants (84% with commercial health insurance and at least 62% with Medicaid insurance– which is an underestimate due to some difficulty identifying eye care providers in MAX) who did not undergo any glaucoma testing during the 15 month follow-up period had at least one visit to an eye care provider during that time frame. Thus, many of these enrollees had an opportunity to undergo testing, even though they did not. Unfortunately, with claims data alone it is difficult to determine whether the patient refused testing, whether the provider lacked the necessary equipment to perform the testing, or whether testing was simply overlooked. While physician reimbursement for care of Medicaid enrollees varies by state, there are some states where the Medicaid physician fee is 50% or less than that of Medicare. This reduced reimbursement may affect utilization of testing, especially for time-consuming tests like perimetry. There may be several other contributing factors as well. Medicaid recipients may have a more difficult time locating an eye care provider who will accept their insurance.24,25 Surveys have demonstrated that ophthalmologists are less likely to accept patients with Medicaid insurance compared to other health insurance types.24,25 Providers who are willing to care for Medicaid enrollees tend to be concentrated in academic medical centers, community health centers, or other large practices.26 For patients who are indigent, transportation to providers’ offices can be challenging.27–29 Even if Medicaid enrollees can identify providers who accept their insurance, if the demand of patients exceeds the supply of providers, it may take a long time to get an appointment and this may impact rates of testing.
Patient-related factors may also contribute to some of the differences in utilization we are observing. Medicaid recipients tend to be less well educated and have lower health literacy levels compared to those with other forms of health insurance.30 As such, they may be less aware of the importance of regular monitoring of OAG. In our analyses, we learned that among the subset of persons with no record of any glaucoma testing during the 15 months after initial diagnosis, a greater proportion of those in Medicaid lacked any record of visits compared to those with commercial health insurance. Earlier work by Friedman and colleagues also identified that a sizeable number of patients with newly-diagnosed glaucoma do not return for follow-up care within 18 months after initial diagnosis.31 Overall, approximately 19% of patients with Medicaid insurance in the U.S. are black and 31% are Hispanic/Latino.32 Since blacks are more likely to have OAG1–5 and much more likely to go blind from OAG,6–8 if anything, these patients require more visits, greater surveillance, and timely receipt of interventions compared to whites.
With the expansion of Medicaid under the PPACA, there will likely be an influx of patients with OAG enrolling in Medicaid. This, coupled with the aging U.S. population, makes it essential that we look for ways to improve the quality of care of OAG for Medicaid recipients. Increasing reimbursement to eye care providers caring for patients in Medicaid if they demonstrate evidence that they are following established guidelines for glaucoma care (similar to some of the initiatives aimed at improving quality of care for Medicare beneficiaries) may be a way to improve care quality. Better education of eye care providers on how patients in Medicaid are less likely to receive monitoring for OAG progression so that they can be proactive with their Medicaid patients to ensure they do not go for lengthy time periods without testing may be helpful at reducing the disparities observed. Another possibility may involve non-traditional methods of reaching Medicaid enrollees, such as creating “eye mobiles” equipped with glaucoma testing equipment that can travel to churches or community centers in less affluent communities.33 Moreover, technological advances have facilitated the ability to perform VF testing, FP, and OOI on handheld devices such as tablets and smartphones. Taking advantage of such advances may be an innovative way to reach this segment of the population.34
Study Strengths / Limitations
This is the first study, to our knowledge, to assess monitoring of OAG for enrollees in Medicaid compared to patients covered by commercial health insurance. Our study had adequate numbers of racial minorities with newly-diagnosed OAG to enable comparisons of care between the two plans and stratified by race/ethnicity. Identifying patients with OAG and their receipt of glaucoma testing were captured from claims submitted by eye care providers, which is more accurate than patient self-reporting.35
Our study has several limitations.36 Claims data lack the detailed clinical information needed to determine the appropriateness of testing that was or was not performed. Likewise, we lacked information on eye care providers’ access to testing equipment to perform these tests or the cost of such equipment, which may have affected utilization. We also cannot determine how much of the differences in utilization we are noting are due to a patient’s inability or unwillingness to undergo additional testing because of financial constraints or other reasons. While the Optum database specifies for each encounter whether the eye care provider caring for the patient was an ophthalmologist or optometrist, the ability to distinguish care by ophthalmologists versus optometrists was lacking for some of the Medicaid data, thereby preventing consideration of eye care provider characteristics in our analyses. Our analyses did not consider out-of-pocket costs which likely disproportionately affected persons in Medicaid from undergoing testing more than those with commercial health insurance. Finally, our findings may not be generalizable to those with other types of health insurance, or those who lack health insurance, who may be even less likely to receive care that is in accordance with clinical practice guidelines than those with Medicaid.
Conclusion
Our study highlights that a person’s health insurance and race can have a profound effect on receipt of timely recommended testing to monitor OAG for disease progression. Addressing these disparities will require efforts by health policy makers, clinicians, and health services researchers to identify opportunities to improve the quality of care received by Medicaid recipients with OAG.
Acknowledgments
Financial support: W.K. Kellogg Foundation, East Battle Creek, MI; R01 EY026641 National Eye Institute, Bethesda, MD (JDS); American Glaucoma Society Mentoring for Advancement of Physician-Scientists (MAPS) Award, American Glaucoma Society, San Francisco, CA (ARE).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented, in part, at the 25th annual American Glaucoma Society meeting, February 28, 2015, Coronado, CA.
The authors have no proprietary interest in any material discussed in this manuscript.
References
- 1.Tielsch JM, Sommer A, Katz J, et al. Racial variations in the prevalence of primary open–angle glaucoma. The Baltimore Eye Survey. JAMA. 1991;266(3):369–7. [PubMed] [Google Scholar]
- 2.Rudnicka AR, Mt-Isa S, Owen CG, et al. Variations in primary open-angle glaucoma prevalence by age, gender, and race: a Bayesian meta-analysis. Invest Ophthalmol Vis Sci. 2006;47(10):4254–61. [DOI] [PubMed] [Google Scholar]
- 3.Ostermann J, Sloan FA, Herndon LW, et al. Racial differences in glaucoma care: the longitudinal pattern of care. Arch Ophthalmol. 2005;123(12):1693–8. [DOI] [PubMed] [Google Scholar]
- 4.Stein JD, Kim DS, Niziol LM, et al. Differences in rates of glaucoma among Asian Americans and other racial groups, and among various Asian ethnic groups. Ophthalmology. 2011;118(6):1031–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Varma R, Ying-Lai M, Francis BA, et al. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2004. 111(8):1439–48. [DOI] [PubMed] [Google Scholar]
- 6.Chen PP. Risk and risk factors for blindness from glaucoma. Curr Opin Ophthalmol. 2004;15(2):107–111. [DOI] [PubMed] [Google Scholar]
- 7.Grant WM, Burke JF Jr. Why do some people go blind from glaucoma? Ophthalmology. 1982;89(9):991–998. [DOI] [PubMed] [Google Scholar]
- 8.Stone JS, Muir KW, Stinnett SS, et al. Glaucoma blindness at a tertiary eye care center. N C Med J. 2015; 76(4):211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stein JD, Talwar N, Laverne AM, et al. Racial disparities in the use of ancillary testing to evaluate individuals with open-angle glaucoma. Arch Ophthalmol. 2012; 130(12):1579–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Devgan U, Yu F, Kim E, et al. Surgical undertreatment of 443 glaucoma in black beneficiaries of Medicare. Arch Ophthalmol. 2000;118(2):253–6. [DOI] [PubMed] [Google Scholar]
- 11.Recent Trends in Medicaid and CHIP Enrollment as of January 2015: Early Finding from the CMS Performance Indicator Project. Available at: http://kff.org/medicaid/issue-brief/recent-trends-in-medicaid-and-chip-enrollment-as-of-january-2015-early-findings-from-the-cms-performance-indicator-project/ Accessed December 28, 2016.
- 12.Kaiser Commission on Medicaid and the Uninsured. Medicaid: A primer. Washington, DC: Henry J. Kaiser Family Foundation; 2013. Available at: http://kaiserfamilyfoundation.files.wordpress.com/2010/06/7334-05.pdf Accessed December 28, 2016. [Google Scholar]
- 13.Martires K, Kurlander D, Minwell G, et al. Patterns of cancer screening in primary care from 2005 to 2010. Cancer. 2014. January 15:120(2):253–61. [DOI] [PubMed] [Google Scholar]
- 14.McMorrow S, Long SK, Fogel A. Primary Care Providers Ordered Fewer Preventive Services For Women With Medicaid Than For Women With Private Coverage. Health Aff (Millwood). 2015. June;34(6):1001–9. [DOI] [PubMed] [Google Scholar]
- 15.Pulte D, Jansen L, Brenner H. Survival disparities by insurance type for patients aged 15-64 years with non-Hodgkin lymphoma. Oncologist. 2015. May;20(5):554–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Munene G, Parker RD, Shaheen AA, et al. Disparities in the surgical treatment of colorectal liver metastases. J Natl Med Assoc. 2013. Summer;105(2):128–37. [DOI] [PubMed] [Google Scholar]
- 17.Abraham A, Al-Refaie W, Parsons H, et al. Disparities in pancreas cancer care. Ann Surg Oncol. 2013. June;20(6):2078–87. [DOI] [PubMed] [Google Scholar]
- 18.Prum BE Jr, Rosenberg LF, Gedde SJ, et al. Primary Open-465 Angle Glaucoma Preferred Practice Pattern(®) Guidelines. Ophthalmology. 2016. January;123(1):P41–P111. [DOI] [PubMed] [Google Scholar]
- 19.Matone M, Localio R, Huang YS, et al. The relationship between mental health diagnosis and treatment with second-generation antipsychotics over time: a national study of U.S. Medicaid-enrolled children. Health Serv Res. 2012. October;47(5):1836–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Palmsten K, Huybrechts KF, Mogun H, et al. Harnessing the Medicaid Analytic eXtract (MAX) to Evaluate Medications in Pregnancy: Design Considerations. PLoS One. 2013. June 26;8(6):e67405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Physician International Classification of Diseases 9th Revision, Clinical Modification. Vols. 1 and 2 Chicago: American Medical Association Press; 2006. [Google Scholar]
- 22.CPT 2006: Current Procedural Terminology Professional Edition. Chicago, IL: American Medical Association; 2006. [Google Scholar]
- 23.Sloan FA, Brown DS, Carlisle ES, et al. Monitoring Visual Status: Why Patients Do or Do Not Comply with Practice Guidelines. Health Serv Res. 2004. October;39(5):1429–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. QuickStats: percentage of office-based physicians accepting new patients, by type of payment accepted—United States, 1999-1000 and 2008-2009. MMWR Morb Mortal Wkly Rep. 2011;60(27):928. [Google Scholar]
- 25.Decker SL. In 2011 Nearly One-Third of Physician Said They Would Not Accept New Medicaid Patients, But Rising Fees May Help. Health Affairs 2012: 31(8):1673–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cunningham P, May J. Medicaid Patients Increasingly Concentrated Among Physicians. Track Rep. 2006. August;(16):1–5. [PubMed] [Google Scholar]
- 27.Owsley C, McGwin G, Scilley K, et al. Perceived barriers to care and 486 attitudes about vision and eye care: focus groups with older African Americans and eye care providers. Invest Ophthalmol Vis Sci. 2006. July;47(7):2797–802. [DOI] [PubMed] [Google Scholar]
- 28.Gower EW, Silverman E, Cassard SD, et al. Barriers to attending an eye examination after vision screening referral within a vulnerable population. J Health Care Poor Underserved. 2013. August;24(3):1042–52. [DOI] [PubMed] [Google Scholar]
- 29.Arcury TA, Preisser JS, Gesler WM, et al. Access to Transportation and Health Care Utilization in a Rural Region. J Rural Health 2005;21:31–8. [DOI] [PubMed] [Google Scholar]
- 30.Sentell T Implications for Reform: Survey of California Adults Suggests Low Health Literacy Predicts Likelihood of Being Uninsured. Health Affairs 2012; 31(5)1039–48. [DOI] [PubMed] [Google Scholar]
- 31.Friedman DS, Cramer J, Quigley H. A more proactive approach is needed in glaucoma care. Arch Ophthalmol. 2005. August;123(8):1134–5. [DOI] [PubMed] [Google Scholar]
- 32.Kaiser Family Foundation. Distribution of the Nonelderly with Medicaid by Race/Ethnicity. Available at: http://kff.org/medicaid/state-indicator/distribution-by-raceethnicity-4/ Accessed October 26, 2016.
- 33.Elam AR, Lee PP. Barriers to and Suggestions on Improving Utilization of Eye Care in High-Risk Individuals: Focus Group Results. ISRN 2014:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sreelatha OK, Ramesh SV. Teleophthalmology: Improving patient outcomes? Clin Ophthalmol. 2016. February 10;10:285–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patty L, Wu C, Torres M, et al. Validity of self-reported eye disease and treatment in a population-based study: the Los Angeles Latino Eye Study. Ophthalmology. 2012;119(9):1725–1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stein JD, Lum F, Lee PP, et al. Use of health care claims data to study 508 patients with ophthalmologic conditions. Ophthalmology 2014;121:1134–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]


