Key Points
Question
Is physician involvement in prehospital advanced life support (ALS) associated with increased chance of favorable outcomes after traumatic out-of-hospital cardiac arrest?
Findings
In this Japanese nationwide, population-based registry study, including 4382 patients with traumatic out-of-hospital cardiac arrest, ALS by physician was associated with increased chance of prehospital return of spontaneous circulation and 1-month survival compared with both ALS by emergency medical service personnel and basic life support. Advanced life support by physician was also associated with increased chance of neurologically favorable survival compared with ALS by emergency medical service personnel, although there was no difference between ALS by physician and basic life support.
Meaning
Physicians should probably be involved in prehospital ALS in traumatic out-of-hospital cardiac arrest cases; however, further well-designed studies are required to determine the optimal prehospital care for patients with traumatic out-of-hospital cardiac arrest.
Abstract
Importance
Controversy remains as to whether advanced life support (ALS) or basic life support (BLS) is superior for critically ill and injured patients, including out-of-hospital cardiac arrest (OHCA) and major trauma, in the prehospital setting.
Objective
To assess whether prehospital ALS should be provided for traumatic OHCA and who should perform it.
Design, Setting, and Participants
Japanese government-managed nationwide population-based registry data of patients with OHCA transported to an emergency hospital were analyzed. Patients who experienced traumatic OHCA following a traffic collision from 2013 to 2014 were included. Patients provided prehospital ALS by a physician were compared with both patients provided ALS by emergency medical service (EMS) personnel and patients with only BLS. The data were analyzed on May 1, 2017.
Exposures
Advanced life support by physician, ALS by EMS personnel, or BLS only.
Main Outcomes and Measures
The primary outcome was 1-month survival. The secondary outcomes were prehospital return of spontaneous circulation and favorable neurologic outcomes with the Glasgow-Pittsburgh cerebral performance category score of 1 or 2.
Results
A total of 4382 patients were included (mean [SD] age, 57.5 [22.2] years; 67.9% male); 828 (18.9%) received prehospital ALS by physician, 1591 (36.3%) received prehospital ALS by EMS personnel, and 1963 (44.8%) received BLS only. Among these patients, 96 (2.2%) survived 1 month after OHCA, including 26 of 828 (3.1%) for ALS by physician, 25 of 1591 (1.6%) for ALS by EMS personnel, and 45 of 1963 (2.3%) for BLS. After adjusting for potential confounders using multivariable logistic regression, ALS by physician was significantly associated with higher odds for 1-month survival compared with both ALS by EMS personnel and BLS (adjusted OR, 2.13; 95% CI, 1.20-3.78; and adjusted OR, 1.94; 95% CI, 1.14-3.25; respectively), whereas there was no significant difference between ALS by EMS personnel and BLS (adjusted OR, 0.91; 95% CI, 0.54-1.51). A propensity score–matched analysis in the ALS cohort showed that ALS by physician was associated with increased chance of 1-month survival compared with ALS by EMS personnel (risk ratio, 2.00; 95% CI, 1.01-3.97; P = .04). This association was consistent across a variety of sensitivity analyses.
Conclusions and Relevance
In traumatic OHCA, ALS by physician was associated with increased chance of 1-month survival compared with both ALS by EMS personnel and BLS.
This population-based registry study assesses whether prehospital advanced life support should be provided for traumatic out-of-hospital cardiac arrest following a traffic collision and who should perform it.
Introduction
More than 120 000 Japanese individuals have an out-of-hospital cardiac arrest (OHCA) annually.1,2,3 Although the survival rate from OHCA is improving, no more than approximately 10% of patients with OHCA survive 1 month after OHCA.1,2,3 Patients with traumatic OHCA, accounting for less than 10% of the total patients with OHCA, have an extremely low survival rate, not only in Japan4 but also throughout the world.5,6,7,8
Prehospital advanced life support (ALS) for critically ill and injured patients, including those with OHCA and major trauma, has been introduced,9,10,11,12,13 developed, and expanded in many emergency medical service (EMS) systems.14,15,16,17 Emergency medical service system models are quite varied around the world. Some countries (such as France) have the Franco-German EMS system, in which a physician is brought to the patient,18,19 while other countries (such as the United States, Japan, and Australia) have the Anglo-American EMS system, in which a patient is brought to the physician (that is, prehospital care is provided by nonphysicians).20,21,22 Tiers of care provided by EMS system also vary depending on countries.20,21,22 In the United States, EMS system models are numerous and varied depending on areas.21 In Japan, the EMS system is principally the Anglo-American EMS system and 1-tiered, and some municipalities have their own physician-staffed EMS system.20,23
Thus far, to our knowledge, the benefit of prehospital ALS for traumatic OHCA has not been established. To our knowledge, no randomized clinical trials comparing ALS with basic life support (BLS) have been conducted in the traumatic OHCA population, and such a trial may be ethically difficult to conduct. In addition, observational studies of traumatic OHCA comparing ALS and BLS are scarce. Previous high-quality studies of OHCA or major trauma patients comparing ALS and BLS failed to find the survival benefit of ALS over BLS, although most studies on OHCA excluded trauma cases, and studies on major trauma usually included non–cardiac arrest cases.24,25,26,27 One of the potential reasons for those failures to show the benefit of ALS vs BLS may be a lack of consideration of who should perform prehospital ALS. Although there is controversy as to who should perform prehospital ALS,28 several studies have indicated the potential effectiveness of physician involvement in prehospital ALS in OHCA or major trauma cases.23,29,30,31
To simultaneously examine both whether prehospital ALS should be provided and who should perform prehospital ALS, we sought to assess whether prehospital ALS by a physician would be associated with an increased chance of favorable outcomes in OHCA with blunt trauma following a traffic collision compared with both ALS by EMS personnel and BLS.
Methods
Data Source, Study Setting, and Participants
The All-Japan Utstein Registry is a nationwide, population-based registry of patients with OHCA sponsored by the Fire and Disaster Management Agency. In this registry, data were prospectively collected using the Utstein-style uniform reporting.32,33 As has been described in detail previously,1,2,3 trained EMS personnel prospectively collect data on patients with OHCA transported to an emergency hospital. This registry included almost all patients with OHCA, including those with do-not-resuscitate orders, because EMS personnel in Japan are not allowed to terminate out-of-hospital resuscitation except in specific situations (eg, decapitation, rigor mortis, livor mortis, and decomposition). Data are collected from 3 sources (1-1-9 dispatch centers, fire stations, and receiving hospitals) and are integrated into the All-Japan Utstein Registry system on the Fire and Disaster Management Agency database server. The certification by the Fire and Disaster Management Agency and the logical internal checks with standardized software secure the integrity, accuracy, and completeness of the data.
In Japan, all EMS personnel perform cardiopulmonary resuscitation (CPR) according to the Japanese CPR guidelines, which basically conform to the American Heart Association guidelines, although EMS personnel have different authorization depending on their completed training program.34 An ambulance generally has a crew of 3 EMS personnel. Although a physician accompanies an ambulance in some municipalities, physician-staffed ambulances are not yet widespread. Instead, most ambulances include at least 1 emergency life-saving technician (ELST), certified to insert an intravenous catheter and a supraglottic airway device (since 1991). In addition, a specially trained ELST, who has completed an extensive training program, can administer epinephrine and insert an endotracheal tube. Epinephrine administration and endotracheal intubation by specially trained ELST officially started in April 2006 and July 2004, respectively. As of 2014, almost all (97.4%) ambulances included at least 1 ELST, and most (82.9%) were specially trained ELSTs.34 However, ALS procedures cannot be performed without the instruction of a medical director in each municipality. In addition, EMS personnel in Japan are not allowed to perform other advanced interventions (eg, surgical airway, chest drain, or intraosseous access). This means that EMS personnel in Japan can perform only intravenous catheter insertion and fluid infusion, intravenous epinephrine administration, and endotracheal intubation, even if they do all they can. On the other hand, physicians who accompany an ambulance to treat a patient with traumatic OHCA commonly specialize in emergency medicine and can perform any procedure (including blood transfusion, thoracotomy, resuscitative endovascular balloon occlusion of the aorta, or extracorporeal CPR) as long as the equipment and skills permit. Patients with traumatic OHCA are usually transported to a tertiary emergency medical center in each region, and these centers have similar level of capacity to perform sufficient treatment. As of 2012, there were 246 tertiary emergency medical centers; each center covered 500 000 people.
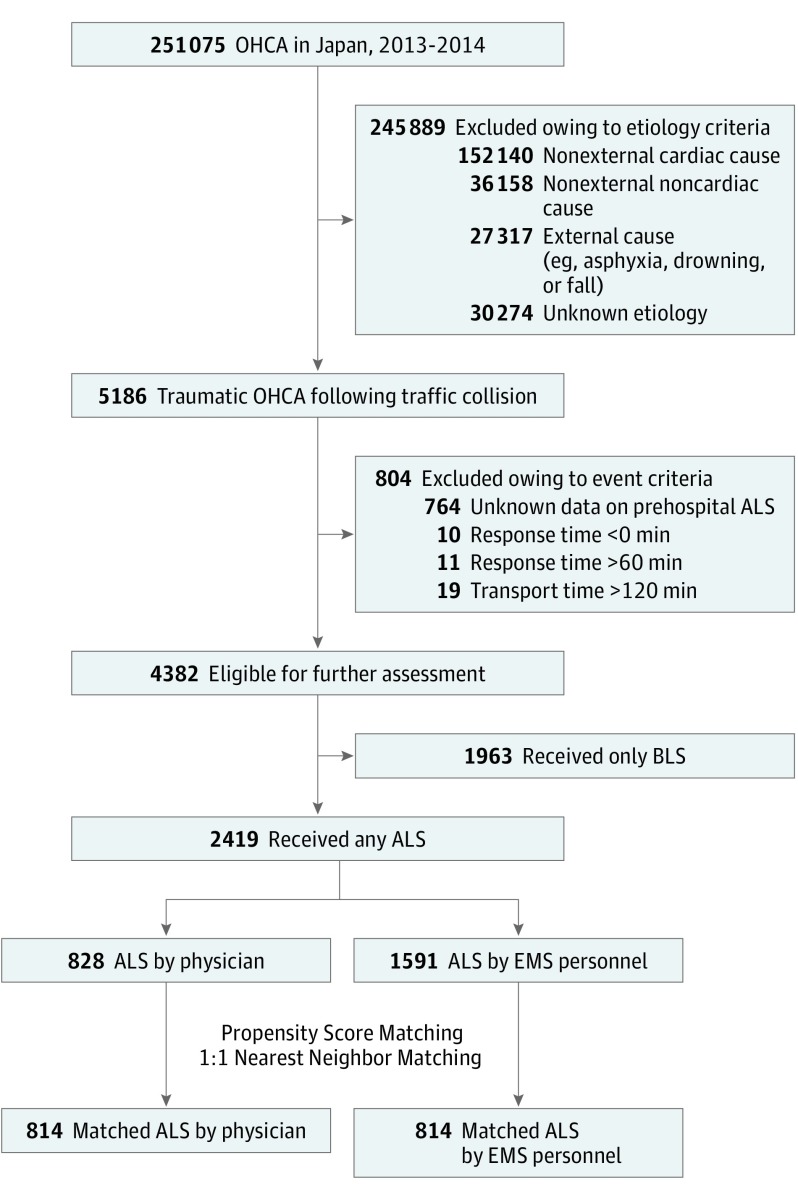
This study included patients with traumatic OHCA following a traffic collision submitted to the All-Japan Utstein Registry between January 1, 2013, and December 31, 2014. We excluded patients with unrealistic or contradictory (ie, negative or considerably long) times and patients with unknown data on prehospital ALS (Figure). Patients who received at least 1 prehospital ALS procedure (ie, intravenous catheter insertion, epinephrine administration, or advanced airway treatment including supraglottic airway device and endotracheal tube) were assigned to the ALS group, whereas patients who did not receive any ALS procedure were assigned to the BLS group.
Figure. Study Flow Diagram.
ALS indicates advanced life support; BLS, basic life support; EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest.
This study was conducted according to the amended Declaration of Helsinki, with a waiver of informed consent owing to the anonymous nature of the data. The study was approved by the institutional review board of University of the Ryukyus, Okinawa, Japan.
Data Collection
Data on patient characteristics (ie, sex and age), bystander characteristics (ie, witnesses and bystander CPR), cardiac arrest characteristics (ie, first documented rhythm and etiology of cardiac arrest), and prehospital care characteristics (ie, intravenous catheter insertion, epinephrine administration, advanced airway treatment, and physician involvement in prehospital ALS) were collected in this registry. A series of EMS activity times (ie, emergency call receipt, contact with patient, and hospital arrival) were recorded by each EMS squad. Time intervals were calculated based on those variables recorded in whole minutes; the response time represents the interval between emergency call and contact with patient, and the transport time represents the interval between contact with patient and hospital arrival. The calculated interval of 1 minute represents that 1 event occurred within the next whole minute after the other event, whereas the time interval of 0 minutes indicates that 2 events occurred within the same whole minute. The etiology of cardiac arrest was determined by attending physicians in the emergency department in collaboration with EMS personnel. To reconfirm the etiology of the cardiac arrest and collect the outcome data on survival and neurological status, a 1-month follow-up survey was conducted by each fire department, based on an inquiry for the receiving hospital. If the patient was transferred or discharged from the hospital within 1 month, further investigations were conducted by the fire department in cooperation with the hospital personnel.
Outcomes
The primary outcome was 1-month survival. The secondary outcomes were prehospital return of spontaneous circulation (ROSC) and favorable neurologic outcome. Neurologic outcome was assessed by inpatient attending physicians using the Glasgow-Pittsburgh cerebral performance category scores 1 month after OHCA. A cerebral performance category score of 1 (good performance) or 2 (moderate disability) was considered a favorable neurologic outcome, and a cerebral performance category score of 3 (severe disability), 4 (vegetative state), or 5 (death) was considered a poor neurologic outcome.33,35
Statistical Analysis
The study cohort was characterized using descriptive statistics. Categorical variables were presented as counts with proportions, and the χ2 test was used to evaluate differences between the 2 groups. Continuous variables were presented as means with standard deviations or medians with interquartile ranges (IQRs), and the t test or the Wilcoxon Mann-Whitney test was used, respectively, to evaluate differences between the 2 groups.
Multivariable logistic regression models were used to determine the association between the type of prehospital care and outcomes, both with and without distinguishing the type of ALS professional. The following variables that could influence the outcomes after OHCA were included in the models: sex, age, witness, bystander CPR, first rhythm, response time, transport time, and a treatment variable (BLS vs ALS, or BLS vs ALS by EMS personnel vs ALS by physician). Adjusted odds ratios (ORs) with 95% confidence intervals were reported.
To further characterize the association between the type of ALS professional (EMS personnel vs physician) and outcomes after OHCA, propensity score analyses were performed in the prehospital ALS cohort. The propensity score for each patient receiving prehospital ALS by physician or EMS personnel was estimated using a multivariable logistic regression model. The model included the following variables with pretreatment characteristics: sex (male or female), age (≤17 years, 18-64 years, or ≥65 years), witness (witnessed or unwitnessed), bystander CPR (any CPR or no CPR), first rhythm (ventricular fibrillation, ventricular tachycardia, pulseless electrical activity, asystole, or others), and response time (<10 minutes or ≥10 minutes). A 1:1 nearest-neighbor matching was performed using a caliper of 0.2 without replacement between patients receiving ALS by physician and ALS by EMS personnel.36 The success of the matching procedure was confirmed by comparing the baseline characteristics with standardized differences within 0.1.37 Risk ratios (RRs) of each outcome for patients receiving prehospital ALS by physician vs EMS personnel were reported with 95% confidence intervals. Absolute risk reduction (ARR) and the number needed to treat (NNT) were also calculated.
Sensitivity analyses were performed for the primary outcome to verify that the results of the comparison between ALS by physician and ALS by EMS personnel did not depend on the method of covariate adjustment of the propensity score matching (eFigure in the Supplement). JMP Pro, version 11.2.0 software (SAS Institute Inc) was used for all statistical analyses. A 2-sided P value of .05 was considered significance level for all hypothesis tests.
Results
During the study period, we identified 4382 patients with traumatic OHCA eligible for analysis (Figure). Of these, 1963 (44.8%) received only BLS in the prehospital settings. Of the remaining 2419 (55.2%), prehospital ALS was performed by physician in 828 patients (18.9%), and by EMS personnel in 1591 patients (36.3%).
Table 1 summarizes the baseline characteristics of the total cohort according to the type of prehospital care. In the total cohort of traumatic OHCA, although most cases (3067 patients [70.0%]) were witnessed, the frequency of bystander CPR was low (863 patients [19.7%]). The median response time was 9 minutes (IQR, 7-12; mean [SD], 10.3 [86.1] minutes). The first rhythm was commonly the nonshockable rhythm (ie, pulseless electrical activity in 1595 patients [36.4%] and asystole in 2364 patients [53.9%]).
Table 1. Baseline Characteristics of the Total Cohort According to the Type of Prehospital Care.
| Characteristic | Total Cohort, No. (%) | Prehospital ALS Cohort, No. (%) | ||||
|---|---|---|---|---|---|---|
| BLS (n = 1963) | ALS (n = 2419) | P Value | By EMS Personnel (n = 1591) | By Physician (n = 828) | P Value | |
| Pretreatment variable | ||||||
| Calendar year | ||||||
| 2013 | 1002 (51.0) | 1263 (52.2) | .44 | 826 (51.9) | 437 (52.8) | .69 |
| 2014 | 961 (49.0) | 1156 (47.8) | 765 (48.1) | 391 (47.2) | ||
| Sex | ||||||
| Male | 1306 (66.5) | 1670 (69.0) | .08 | 1095 (68.8) | 575 (69.4) | .75 |
| Female | 657 (33.5) | 749 (31.0) | 496 (31.2) | 253 (30.6) | ||
| Age, mean (SD), y | 55.9 (22.6) | 58.8 (21.9) | <.001 | 59.2 (21.5) | 58.1 (22.5) | .26 |
| ≤17 | 96 (4.9) | 96 (4.0) | .001 | 54 (3.4) | 42 (5.1) | .07 |
| 18-64 | 1003 (51.1) | 1124 (46.5) | 731 (45.9) | 393 (47.5) | ||
| ≥65 | 864 (44.0) | 1199 (49.6) | 806 (50.7) | 393 (47.5) | ||
| Witness | ||||||
| Witnessed | 1374 (70.0) | 1693 (70.0) | >.99 | 1129 (71.0) | 564 (68.1) | .15 |
| Unwitnessed | 589 (30.0) | 726 (30.0) | 462 (29.0) | 264 (31.9) | ||
| Bystander CPR | ||||||
| Any CPR | 317 (16.1) | 546 (22.6) | <.001 | 367 (23.1) | 179 (21.6) | .42 |
| No CPR | 1646 (83.9) | 1873 (77.4) | 1224 (76.9) | 649 (78.4) | ||
| First rhythm | ||||||
| VF | 52 (2.6) | 51 (2.1) | .001 | 39 (2.5) | 12 (1.4) | .02 |
| VT | 1 (0.1) | 5 (0.2) | 4 (0.3) | 1 (0.1) | ||
| PEA | 698 (35.6) | 897 (37.1) | 591 (37.1) | 306 (37.0) | ||
| Asystole | 1039 (52.9) | 1325 (54.8) | 881 (55.4) | 444 (53.6) | ||
| Other | 173 (8.8) | 141 (5.8) | 76 (4.8) | 65 (7.9) | ||
| Response time from emergency call to contact with patient, min | ||||||
| Median (IQR) | 8 (6-11) | 9 (7-13) | <.001 | 9 (7-12) | 9 (7-14) | .01 |
| Mean (SD) | 9.7 (5.8) | 10.7 (6.3) | <.001 | 10.5 (6.0) | 11.3 (6.8) | .002 |
| Response time interval, min | ||||||
| <10 | 1211 (61.7) | 1325 (54.8) | <.001 | 907 (57.0) | 418 (50.5) | .002 |
| ≥10 | 752 (38.3) | 1094 (45.2) | 684 (43.0) | 410 (49.5) | ||
| Posttreatment variable | ||||||
| Transport time from contact with patient to hospital arrival, min | ||||||
| Median (IQR) | 22 (16-30) | 27 (20-39) | <.001 | 26 (20-36) | 31 (20-47) | <.001 |
| Mean (SD) | 25.4 (14.9) | 31.8 (16.8) | <.001 | 29.7 (14.5) | 35.9 (20.0) | <.001 |
| Total time from emergency call to hospital arrival, min | ||||||
| Median (IQR) | 31 (24-42) | 38 (29-51) | <.001 | 36 (28-48) | 43 (30-59) | <.001 |
| Mean (SD) | 35.1 (17.2) | 42.6 (19.3) | <.001 | 40.2 (17.0) | 47.1 (22.5) | <.001 |
Abbreviations: ALS, advanced life support; BLS, basic life support; CPR, cardiopulmonary resuscitation; EMS, emergency medical service; IQR, interquartile range; PEA, pulseless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia.
Table 2 shows the outcomes of patients with traumatic OHCA by the type of prehospital care in the total cohort. In a comparison between BLS and ALS without distinguishing the type of ALS professional, prehospital ALS was not associated with increased chance of 1-month survival (adjusted OR, 1.24; 95% CI, 0.81-1.91) or neurologic outcome (adjusted OR, 0.90; 95% CI, 0.39-2.04), although prehospital ALS was associated with a higher rate of prehospital ROSC compared with BLS (adjusted OR, 1.87; 95% CI, 1.43-2.46). In a comparison between BLS and ALS distinguishing the type of ALS professional (Table 2; eTable in the Supplement), although there was no difference in 1-month survival between ALS by EMS personnel and BLS (adjusted OR, 0.91; 95% CI, 0.54-1.51), physician involvement in prehospital ALS was associated with increased chance of 1-month survival compared with both BLS (adjusted OR, 1.94; 95% CI, 1.14-3.25) and ALS by EMS personnel (adjusted OR, 2.13; 95% CI, 1.20-3.78). In addition, a significant difference was observed in neurologic outcome between ALS by physician and ALS by EMS personnel (adjusted OR, 3.76; 95% CI, 1.14-14.51), although there was no difference between ALS by physician and BLS (adjusted OR, 1.77; 95% CI, 0.66-4.45).
Table 2. Outcomes of Patients With Traumatic OHCA by the Type of Prehospital Care in the Total Cohorta.
| Group | Prehospital ROSC | One-Month Survival | Neurologic Outcome (CPC 1 or 2) | |||
|---|---|---|---|---|---|---|
| Events, No. (%) | Adjusted OR (95% CI) | Events, No. (%) | Adjusted OR (95% CI) | Events, No. (%) | Adjusted OR (95% CI) | |
| BLS (n = 1963) | 95 (4.8) | 1 [Reference] | 45 (2.3) | 1 [Reference] | 14 (0.7) | 1 [Reference] |
| ALS (n = 2419) | 204 (8.4) | 1.87 (1.43-2.46) | 51 (2.1) | 1.24 (0.81-1.91) | 12 (0.5) | 0.90 (0.39-2.04) |
| By EMS personnel (n = 1591) | 110 (6.9) | 1.60 (1.19-2.16) | 25 (1.6) | 0.91 (0.54-1.51) | 4 (0.3) | 0.47 (0.13-1.35) |
| By physician (n = 828) | 94 (11.4) | 2.41 (1.74-3.35) | 26 (3.1) | 1.94 (1.14-3.25) | 8 (1.0) | 1.77 (0.66-4.45) |
Abbreviations: ALS, advanced life support; BLS, basic life support; CPC, Glasgow-Pittsburgh cerebral performance category; EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; OR, odds ratio; ROSC, return of spontaneous circulation.
The variables that could influence outcomes after OHCA were included in the models.
Table 3 summarizes the baseline characteristics of the propensity score–matched cohort according to the type of ALS professional. After propensity score matching, the baseline characteristics were well balanced on pretreatment characteristics between the ALS by physician and ALS by EMS personnel. For posttreatment characteristics, the transport time was significantly longer in the ALS by physician group compared with the ALS by EMS personnel group.
Table 3. Baseline Characteristics of the Propensity Score–Matched Cohort According to the Type of ALS Professional.
| Characteristic | Propensity Score–Matched Cohort | |||
|---|---|---|---|---|
| ALS by Physician (n = 814) | ALS by EMS Personnel (n = 814) | Standardized Difference | P Value | |
| Pretreatment variable | ||||
| Calendar year | ||||
| 2013 | 432 (53.1) | 424 (52.1) | 0.0200 | .69 |
| 2014 | 382 (46.9) | 390 (47.9) | −0.0200 | |
| Sex | ||||
| Male | 546 (69.3) | 567 (69.7) | −0.0087 | .87 |
| Female | 250 (30.7) | 247 (30.3) | 0.0087 | |
| Age, mean (SD), y | 58.5 (22.2) | 58.4 (22.2) | 0.0045 | .90 |
| ≤17 | 36 (4.4) | 31 (3.8) | 0.0303 | .82 |
| 18-64 | 387 (47.5) | 392 (48.2) | −0.0140 | |
| ≥65 | 391 (48.0) | 391 (48.0) | 0.0000 | |
| Witness | ||||
| Witnessed | 553 (67.9) | 561 (68.9) | −0.0215 | .67 |
| Unwitnessed | 261 (32.1) | 253 (31.1) | 0.0215 | |
| Bystander CPR | ||||
| Any CPR | 173 (21.3) | 164 (20.1) | 0.0296 | .58 |
| No CPR | 641 (78.7) | 650 (79.9) | −0.0296 | |
| First rhythm | ||||
| VF | 12 (1.5) | 10 (1.2) | 0.0260 | .97 |
| VT | 1 (0.1) | 2 (0.2) | −0.0258 | |
| PEA | 304 (37.3) | 303 (37.2) | 0.0021 | |
| Asystole | 444 (54.5) | 444 (54.5) | 0.0000 | |
| Other | 53 (6.5) | 55 (6.8) | −0.0120 | |
| Response time from emergency call to contact with patient, min | ||||
| Median (IQR) | 9 (7-14) | 9 (7-13) | NA | .84 |
| Mean (SD) | 11.3 (6.8) | 11.1 (6.5) | 0.0301 | .91 |
| Response time interval, min | ||||
| <10 | 413 (50.7) | 409 (50.2) | 0.0100 | .84 |
| ≥10 | 401 (49.3) | 405 (49.8) | −0.0100 | |
| Posttreatment variable | ||||
| Transport time from contact with patient to hospital arrival, min | ||||
| Median (IQR) | 31 (20-47) | 27 (20-37) | NA | <.001 |
| Mean (SD) | 35.8 (20.0) | 29.9 (13.9) | 0.3426 | <.001 |
| Total time from emergency call to hospital arrival, min | ||||
| Median (IQR) | 43 (30-59) | 37 (29-49) | NA | <.001 |
| Mean (SD) | 47.1 (22.5) | 40.9 (16.6) | 0.3136 | <.001 |
Abbreviations: ALS, advanced life support; CPR, cardiopulmonary resuscitation; EMS, emergency medical service; IQR, interquartile range; NA, not applicable; PEA, pulseless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia.
Table 4 shows the outcomes of patients with traumatic OHCA by the type of ALS professional in the propensity score–matched cohort. Physician involvement in prehospital ALS was associated with increased chance of 1-month survival compared with ALS by EMS personnel (24 of 814 [3.0%] vs 12 of 814 [1.5%]; RR, 2.00; 95% CI, 1.01-3.97; P = .04; ARR, 1.47%; NNT, 67.83). Similar associations were observed for prehospital ROSC (87 of 814 [10.7%] vs 57 of 814 [7.0%]; RR, 1.53; 95% CI, 1.11-2.10; P = .009; ARR, 3.69%; NNT, 27.13), and favorable neurologic outcome (7 of 814 [0.9%] vs 0 of 814; P = .008; ARR, 0.86%; NNT, 116.28).
Table 4. Outcomes of Patients With Traumatic OHCA by the Type of ALS Professional in the Propensity Score–Matched Cohort.
| Outcome | Favorable Outcomes, No. (%) | RR (95% CI) | P Value | |
|---|---|---|---|---|
| ALS by Physician (n = 814) | ALS by EMS Personnel (n = 814) | |||
| Prehospital ROSC | 87 (10.7) | 57 (7.0) | 1.53 (1.11-2.10) | .009 |
| 1-mo Overall survival | 24 (3.0) | 12 (1.5) | 2.00 (1.01-3.97) | .04 |
| Neurologic outcome (CPC 1 or 2) | 7 (0.9) | 0 | NA | .008 |
| CPC 1 | 5 (0.6) | 0 | NA | NA |
| CPC 2 | 2 (0.3) | 0 | NA | NA |
| CPC 3 | 6 (0.7) | 3 (0.4) | NA | NA |
| CPC 4 | 10 (1.2) | 8 (1.0) | NA | NA |
| CPC 5 | 791 (97.2) | 803 (98.6) | NA | NA |
Abbreviations: ALS, advanced life support; CPC, Glasgow-Pittsburgh cerebral performance category; EMS, emergency medical service; NA, not applicable; OHCA, out-of-hospital cardiac arrest; ROSC, return of spontaneous circulation; RR, risk ratio.
Discussion
Principal Findings
In this nationwide population-based observational study of traumatic OHCA, physician involvement in prehospital ALS was associated with increased chance of 1-month survival compared with both ALS by EMS personnel and BLS, although no difference was observed between ALS by EMS personnel and BLS. The association of the type of ALS professional with 1-month survival was consistent across a variety of sensitivity analyses, which indicated that the relationship was robust. Advanced life support by physician was also associated with increased chance of favorable neurologic outcome compared with ALS by EMS personnel, although there was no difference in neurologic outcome between ALS by physician and BLS.
Previous Studies and Important Differences With This Study
To our knowledge, there are no randomized clinical trials comparing ALS vs BLS in traumatic OHCA, regardless of distinguishing the type of ALS professional. Even if study population is not limited to traumatic OHCA but expanded to nontraumatic OHCA or major trauma without cardiac arrest, there are no randomized clinical trials but several high-quality studies comparing ALS and BLS. However, those studies failed to find the survival benefit of ALS vs BLS24,26; on the contrary, several studies indicated that ALS might be associated with worse outcomes compared with BLS.25,27 One of the limitations of those studies, or a potential reason for failures to show the benefit of ALS vs BLS, may be lack of consideration on who should perform prehospital ALS because several studies have indicated the advantage of physician involvement in prehospital ALS in OHCA or major trauma cases.23,29,30,31 Actually, our findings indicated ALS by physician was associated with increased chance of 1-month survival compared with BLS; however, without distinguishing the type of ALS professional, there was no difference in survival between ALS and BLS. Our study extends the findings of previous studies by distinguishing ALS by physician from ALS by EMS personnel, comparing ALS by physician with both ALS by EMS personnel and BLS, including a large study sample, evaluating 1-month neurologic outcomes in addition to survival, and using several robust covariate adjustment methods.
Differences Between ALS by Physician and ALS by EMS Personnel
Several reasons were considered to explain the advantages of ALS by physicians compared with ALS by EMS personnel. Physicians can perform ALS based on their own judgment, but EMS personnel need permission or instruction from a medical director in each municipality to perform ALS, which may prevent EMS personnel from timely treatments. There might be differences in the proficiency in ALS procedures between physician and EMS personnel. Systematic reviews and meta-analyses indicated that there was a significant difference in the success rate of prehospital endotracheal intubation between physician and EMS personnel.38,39 The lower success rate of advanced interventions could lead to longer interruption of CPR or lower quality of CPR, which would be fatal. Because establishing vascular access is essential to administer needed fluids or medications, intraosseous access can be substituted for intravenous access if an ALS professional has difficulty rapidly establishing intravenous access.40,41,42,43,44 However, EMS personnel are not allowed to establish intraosseous access in Japan. In addition, there are other advanced interventions that EMS personnel are not allowed to perform (eg, surgical airway, chest drain, pericardial drain, or thoracotomy). Such advanced interventions that only physicians can perform might have a great effect on survival after traumatic OHCA.45,46,47,48,49 Unfortunately, the information on such interventions could not be obtained from the All-Japan Utstein Registry data.
Limitations
First, despite using a variety of analytical techniques in an effort to control for selection bias and confounders, unmeasured confounding could remain. The life support technique, BLS or ALS, provided by the EMS personnel was not random and depended on the instruction of the medical director in each municipality. However, we cannot know why the medical director chose BLS or ALS from this registry. Whether a physician would accompany an ambulance was determined for each municipality. However, we cannot identify which patient belonged to which municipality in this registry. Although there are approximately 800 fire departments (each fire department covers 1 or several municipalities) in Japan, we were able to obtain information on only 47 prefectures (each prefecture consists of numerous municipalities) in this registry. Because municipalities in each prefecture are not homogenous, we could not adjust for regional clusters.50 In addition, EMS personnel in Japan are not allowed to terminate out-of-hospital resuscitation, whereas physicians can declare death out of the hospital and can decide not to transport the patient. That might cause survivorship bias, although almost all patients are transported to the hospital on procedural grounds.
Second, the generalizability of our findings to any type of traumatic OHCA is uncertain. Because the etiology of cardiac arrest among the patients included in this study was mostly blunt trauma following a traffic collision, it is uncertain whether our findings can be generalized to penetrating trauma. In addition, we could not know the detailed injured area (eg, head, chest, abdomen, or extremities) or injury severity (eg, injury severity score, or abbreviated injury scale score).
Third, the generalizability of our findings to other countries is unknown. The Japanese style of EMS system may differ from that in other countries; compared with Japan, physicians might be more commonly involved in prehospital care, EMS personnel might have more chance to perform ALS procedures, or EMS personnel might be allowed to perform more advanced interventions.
Fourth, the quality of ALS procedure was not assessed. Because failed attempts at ALS procedures were not recorded in this registry, some patients for whom the attempt to provide ALS procedure had been made might be assigned to the BLS group.
Fifth, the data on in-hospital or postresuscitation care that could affect the outcomes after traumatic OHCA were unavailable, although patients with traumatic OHCA are principally transported to a tertiary emergency medical center in each region and these centers have similar levels of capability. Because comparing the registry data with the medical record data at the patient level was impossible owing to anonymization, our analyses could not be adjusted for characteristics on in-hospital or postresuscitation care.51
Finally, the effectiveness of physician involvement in prehospital ALS on neurologic outcome was uncertain compared with BLS. The sample size was likely too small to detect differences in neurologic outcome. In addition, scoring the cerebral performance category could cause interrater bias. An adequately powered and well-designed study would be required.
Conclusions
The results of this nationwide, population-based observational study of traumatic OHCA from 2013 to 2014 indicated that physician involvement in prehospital ALS was associated with increased chance of prehospital ROSC and 1-month survival compared with both ALS by EMS personnel and BLS. Advanced life support by physician was also associated with increased chance of favorable neurologic outcome compared with ALS by EMS personnel, but no difference was observed compared with BLS.
Our findings have important policy implications, although further well-designed studies (including a cost-effectiveness analysis) are required. To improve outcomes after traumatic OHCA, increasing physician-manned ambulances may be effective. Another effective option may be to permit EMS personnel to perform ALS based on their own judgment and/or expand the range of available procedures that EMS personnel can learn, practice, and perform.
eFigure. Sensitivity Analyses for One-month Survival in the Prehospital ALS Cohort
eTable. Outcomes of Traumatic Patients With OHCA in ALS by Physician vs ALS by EMS Personnel
References
- 1.Kitamura T, Iwami T, Kawamura T, et al. ; Japanese Circulation Society Resuscitation Science Study Group . Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation. 2012;126(24):-. [DOI] [PubMed] [Google Scholar]
- 2.Fukuda T, Ohashi-Fukuda N, Matsubara T, et al. . Trends in outcomes for out-of-hospital cardiac arrest by age in Japan: an observational study. Medicine (Baltimore). 2015;94(49):e2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakahara S, Tomio J, Ichikawa M, et al. . Association of bystander intervenetions with neurologically intact survival among patients with bystander-witnessed out-of-hospital cardiac arrest in Japan. JAMA. 2015;314(3):247-254. [DOI] [PubMed] [Google Scholar]
- 4.Tsutsumi Y, Fukuma S, Tsuchiya A, et al. . Association between spinal immobilization and survival at discharge for on-scene blunt traumatic cardiac arrest: a nationwide retrospective cohort study. Injury. 2018;49(1):124-129. [DOI] [PubMed] [Google Scholar]
- 5.Zwingmann J, Mehlhorn AT, Hammer T, Bayer J, Südkamp NP, Strohm PC. Survival and neurologic outcome after traumatic out-of-hospital cardiopulmonary arrest in a pediatric and adult population: a systematic review. Crit Care. 2012;16(4):R117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hopson LR, Hirsh E, Delgado J, Domeier RM, McSwain NE, Krohmer J; National Association of EMS Physicians; American College of Surgeons Committee on Trauma . Guidelines for withholding or termination of resuscitation in prehospital traumatic cardiopulmonary arrest: joint position statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma. J Am Coll Surg. 2003;196(1):106-112. [DOI] [PubMed] [Google Scholar]
- 7.Beck B, Tohira H, Bray JE, et al. . Trends in traumatic out-of-hospital cardiac arrest in Perth, Western Australia from 1997 to 2014. Resuscitation. 2016;98:79-84. [DOI] [PubMed] [Google Scholar]
- 8.Barnard E, Yates D, Edwards A, Fragoso-Iñiguez M, Jenks T, Smith JE. Epidemiology and aetiology of traumatic cardiac arrest in England and Wales: a retrospective database analysis. Resuscitation. 2017;110:90-94. [DOI] [PubMed] [Google Scholar]
- 9.Pantridge JF, Geddes JS. A mobile intensive-care unit in the management of myocardial infarction. Lancet. 1967;2(7510):271-273. [DOI] [PubMed] [Google Scholar]
- 10.Adgey AA, Scott ME, Allen JD, Nelson PG, Geddes JS, Zaidi SA. Management of ventricular fibrillation outside hospital. Lancet. 1969;1(7607):1169-1171. [DOI] [PubMed] [Google Scholar]
- 11.Eisenberg MS, Copass MK, Hallstrom A, Cobb LA, Bergner L. Management of out-of-hospital cardiac arrest: failure of basic emergency medical technician services. JAMA. 1980;243(10):1049-1051. [PubMed] [Google Scholar]
- 12.Rowley JM, Mounser P, Garner C, Hampton JR. Advanced training for ambulance crews: implications from 403 consecutive patients with cardiac arrest managed by crews with simple training. Br Med J (Clin Res Ed). 1987;295(6610):1387-1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gold CR. Prehospital advanced life support vs “scoop and run” in trauma management. Ann Emerg Med. 1987;16(7):797-801. [DOI] [PubMed] [Google Scholar]
- 14.Link MS, Berkow LC, Kudenchuk PJ, et al. . Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18)(suppl 2):S444-S464. [DOI] [PubMed] [Google Scholar]
- 15.de Caen AR, Berg MD, Chameides L, et al. . Part 12: pediatric advanced life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18)(suppl 2):S526-S542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lavonas EJ, Drennan IR, Gabrielli A, et al. . Part 10: special circumstances of resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18)(suppl 2):S501-S518. [DOI] [PubMed] [Google Scholar]
- 17.ATLS Subcommittee; American College of Surgeons’ Committee on Trauma; International ATLS working group . Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg. 2013;74(5):1363-1366. [DOI] [PubMed] [Google Scholar]
- 18.Dick WF. Anglo-American vs Franco-German emergency medical services system. Prehosp Disaster Med. 2003;18(1):29-35. [DOI] [PubMed] [Google Scholar]
- 19.Duchateau FX, Hamada S, Raux M, et al. ; Traumabase Group . Long-term prognosis after out-of-hospital resuscitation of cardiac arrest in trauma patients: prehospital trauma-associated cardiac arrest. Emerg Med J. 2017;34(1):34-38. [DOI] [PubMed] [Google Scholar]
- 20.Tanigawa K, Tanaka K. Emergency medical service systems in Japan: past, present, and future. Resuscitation. 2006;69(3):365-370. [DOI] [PubMed] [Google Scholar]
- 21.Pozner CN, Zane R, Nelson SJ, Levine M. International EMS systems: the United States: past, present, and future. Resuscitation. 2004;60(3):239-244. [DOI] [PubMed] [Google Scholar]
- 22.Willis CD, Cameron PA, Bernard SA, Fitzgerald M. Cardiopulmonary resuscitation after traumatic cardiac arrest is not always futile. Injury. 2006;37(5):448-454. [DOI] [PubMed] [Google Scholar]
- 23.Yasunaga H, Horiguchi H, Tanabe S, et al. . Collaborative effects of bystander-initiated cardiopulmonary resuscitation and prehospital advanced cardiac life support by physicians on survival of out-of-hospital cardiac arrest: a nationwide population-based observational study. Crit Care. 2010;14(6):R199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stiell IG, Wells GA, Field B, et al. ; Ontario Prehospital Advanced Life Support Study Group . Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):647-656. [DOI] [PubMed] [Google Scholar]
- 25.Sanghavi P, Jena AB, Newhouse JP, Zaslavsky AM. Outcomes after out-of-hospital cardiac arrest treated by basic vs advanced life support. JAMA Intern Med. 2015;175(2):196-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stiell IG, Nesbitt LP, Pickett W, et al. ; OPALS Study Group . The OPALS Major Trauma Study: impact of advanced life-support on survival and morbidity. CMAJ. 2008;178(9):1141-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sanghavi P, Jena AB, Newhouse JP, Zaslavsky AM. Outcomes of basic versus advanced life support for out-of-hospital medical emergencies. Ann Intern Med. 2015;163(9):681-690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Vopelius-Feldt J, Wood J, Benger J. Critical care paramedics: where is the evidence? a systematic review. Emerg Med J. 2014;31(12):1016-1024. [DOI] [PubMed] [Google Scholar]
- 29.Wilson SL, Gangathimmaiah V. Does prehospital management by doctors affect outcome in major trauma? a systematic review. J Trauma Acute Care Surg. 2017;83(5):965-974. [DOI] [PubMed] [Google Scholar]
- 30.Hamilton A, Steinmetz J, Wissenberg M, et al. . Association between prehospital physician involvement and survival after out-of-hospital cardiac arrest: a Danish nationwide observational study. Resuscitation. 2016;108:95-101. [DOI] [PubMed] [Google Scholar]
- 31.Di Bartolomeo S, Sanson G, Nardi G, Michelutto V, Scian F. HEMS vs Ground-BLS care in traumatic cardiac arrest. Prehosp Emerg Care. 2005;9(1):79-84. [DOI] [PubMed] [Google Scholar]
- 32.Cummins RO, Chamberlain D, Hazinski MF, et al. ; American Heart Association . Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style’. Circulation. 1997;95(8):2213-2239. [DOI] [PubMed] [Google Scholar]
- 33.Jacobs I, Nadkarni V, Bahr J, et al. ; International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes . Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004;110(21):3385-3397. [DOI] [PubMed] [Google Scholar]
- 34.Fire and Disaster Management Agency Kyukyukyujo-no genkyo 2014 [Current Situations of Emergency Medical Services and Rescue Services 2014]. Tokyo, Japan: Fire and Disaster Management Agency; 2015. [Google Scholar]
- 35.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480-484. [DOI] [PubMed] [Google Scholar]
- 36.Rosenbaum PR, Donald BR. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39:33-38. [Google Scholar]
- 37.Haukoos JS, Lewis RJ. The Propensity Score. JAMA. 2015;314(15):1637-1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Crewdson K, Lockey DJ, Røislien J, Lossius HM, Rehn M. The success of pre-hospital tracheal intubation by different pre-hospital providers: a systematic literature review and meta-analysis. Crit Care. 2017;21(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lossius HM, Røislien J, Lockey DJ. Patient safety in pre-hospital emergency tracheal intubation: a comprehensive meta-analysis of the intubation success rates of EMS providers. Crit Care. 2012;16(1):R24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anson JA. Vascular access in resuscitation: is there a role for the intraosseous route? Anesthesiology. 2014;120(4):1015-1031. [DOI] [PubMed] [Google Scholar]
- 41.Reades R, Studnek JR, Vandeventer S, Garrett J. Intraosseous versus intravenous vascular access during out-of-hospital cardiac arrest: a randomized controlled trial. Ann Emerg Med. 2011;58(6):509-516. [DOI] [PubMed] [Google Scholar]
- 42.Leidel BA, Kirchhoff C, Bogner V, Braunstein V, Biberthaler P, Kanz KG. Comparison of intraosseous versus central venous vascular access in adults under resuscitation in the emergency department with inaccessible peripheral veins. Resuscitation. 2012;83(1):40-45. [DOI] [PubMed] [Google Scholar]
- 43.Lewis P, Wright C. Saving the critically injured trauma patient: a retrospective analysis of 1000 uses of intraosseous access. Emerg Med J. 2015;32(6):463-467. [DOI] [PubMed] [Google Scholar]
- 44.Engels PT, Erdogan M, Widder SL, et al. . Use of intraosseous devices in trauma: a survey of trauma practitioners in Canada, Australia and New Zealand. Can J Surg. 2016;59(6):374-382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Narvestad JK, Meskinfamfard M, Søreide K. Emergency resuscitative thoracotomy performed in European civilian trauma patients with blunt or penetrating injuries: a systematic review. Eur J Trauma Emerg Surg. 2016;42(6):677-685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Slessor D, Hunter S. To be blunt: are we wasting our time? emergency department thoracotomy following blunt trauma: a systematic review and meta-analysis. Ann Emerg Med. 2015;65(3):297-307.e16. [DOI] [PubMed] [Google Scholar]
- 47.Cook TM, Gupta K. Emergency thoracotomy after cardiac arrest from blunt trauma is not always futile. Resuscitation. 2007;74(1):187-190. [DOI] [PubMed] [Google Scholar]
- 48.Fialka C, Sebök C, Kemetzhofer P, Kwasny O, Sterz F, Vécsei V. Open-chest cardiopulmonary resuscitation after cardiac arrest in cases of blunt chest or abdominal trauma: a consecutive series of 38 cases. J Trauma. 2004;57(4):809-814. [DOI] [PubMed] [Google Scholar]
- 49.Tisherman SA. Salvage techniques in traumatic cardiac arrest: thoracotomy, extracorporeal life support, and therapeutic hypothermia. Curr Opin Crit Care. 2013;19(6):594-598. [DOI] [PubMed] [Google Scholar]
- 50.Haider AH, Saleem T, Leow JJ, et al. . Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? J Am Coll Surg. 2012;214(5):756-768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Haut ER, Mann NC, Kotwal RS Military trauma care’s learning health system: the importance of data driven decision making. http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2016/Trauma-Care/Importance-of-Data-Driven-Decision-Making-CP.pdf. Accessed January 11, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Sensitivity Analyses for One-month Survival in the Prehospital ALS Cohort
eTable. Outcomes of Traumatic Patients With OHCA in ALS by Physician vs ALS by EMS Personnel