Abstract
Background:
Despite several well-described operative techniques, the optimal management of anterior cruciate ligament (ACL) injuries in pediatric patients remains unclear.
Purpose:
To identify surgeons’ preferred ACL reconstruction techniques and postoperative protocols for pediatric patients of various ages.
Study Design:
Cross-sectional study.
Methods:
An electronic survey was administered to surgeons in the Pediatric Research in Sports Medicine (PRiSM) society, resulting in a cohort of experienced respondents who performed a relatively high volume of ACL reconstructions in skeletally immature patients. Surgeon and practice demographic information was recorded. The survey presented the scenario of a patient who had a physical examination and imaging consistent with an acute, isolated ACL tear. The respondents were asked to select their preferred reconstruction technique for female and male patients at consecutive skeletal ages from 8 to 15 years. Surgeons were also asked about postoperative protocol.
Results:
Of 103 surgeons, 88 (85%) responded to the survey, the majority of whom (68%) performed more than 25 pediatric ACL reconstructions annually. The greatest variation in technique was from ages 11 to 13 years in female patients and from 11 to 14 years in male patients. The modified MacIntosh was the most frequently used technique for patients aged 8 to 10 years. An all-epiphyseal technique was preferred over a broader age range in male patients than female patients, with peak use at age 11 in both. A partial transphyseal (hybrid) technique was preferred in slightly older patients, with peak use at age 12 in female patients and 13 in male patients. The transphyseal technique was most widely used at age 13 and older in female patients and 14 and older in male patients. The impact of fellowship training (pediatrics, sports, or both) on technique preference was statistically significant for male patients aged 11 to 13 and female patients 11 and 12 (all P < .05). Surgeons with pediatric orthopaedic training tended to prefer an all-epiphyseal reconstruction, while those with both pediatric and sports medicine training preferred the modified MacIntosh.
Conclusion:
The preferred ACL reconstruction technique varied considerably, especially for patients aged 11 to 13 years. The modified MacIntosh reconstruction was favored in patients aged 10 years or younger, while the transphyseal technique was preferred in female patients aged 13 years and older and in male patients 14 years and older. The surgeon’s fellowship training was significantly associated with his or her preferred surgical technique.
Keywords: ACL, pediatric sports medicine, anterior cruciate ligament reconstruction, technique, skeletally immature
With the increasing incidence of pediatric anterior cruciate ligament (ACL) injuries has come an evolution in management strategies for these patients.5,17,26 Although many surgeons historically recommended nonoperative or delayed surgical treatment for skeletally immature individuals,13 a growing body of literature is reporting the negative consequences of delaying reconstruction.3,6,7,9,14,20,21,23,24 In an attempt to stabilize the knee while allowing normal growth, a number of surgical techniques have been developed for pediatric ACL reconstruction.1,11,15,17,25
Whether any specific type of reconstruction is truly best suited for a given skeletal age is largely unclear.4,8,16,22,27 Biomechanical studies have been unable to discern the superiority of any single technique.10,18 Given this lack of consensus, clinical practice might vary widely. The purpose of this study was to report detailed, current trends in the surgical management of pediatric ACL injuries.
Methods
An electronic survey was distributed to 103 surgeons in the Pediatric Research in Sports Medicine (PRiSM) society via REDCap (Research Electronic Data Capture). The questionnaire was pilot-tested internally at our institution and then among a small sample of members of the American Orthopaedic Society for Sports Medicine prior to distribution to PRiSM members. In this way, we were able to modify and optimize the questionnaire before final dissemination. The survey did not ask for the respondent’s name, institution, or other directly identifiable data.
The first portion of the survey inquired about demographics with the following questions:
Do you perform ACL surgery?
What is your primary type of practice?
What percentage of your practice involves pediatric orthopaedics?
What is your age?
What is your sex?
What percentage of your practice involves sports medicine?
What formal fellowship training have you completed?
Geographically, where do you practice?
How many years have you been in practice?
How many ACL reconstructions do you perform in skeletally immature patients every year?
The next section of the survey consisted of a theoretical clinical scenario involving an acute, sports-related ACL rupture with symptomatic instability and no concomitant injuries or ligamentous laxity. Respondents were asked to choose their preferred reconstruction technique for male and female patients in this scenario at each year of skeletal age between 8 and 15 years. For the sake of the clinical vignette, skeletal age was assumed to be within 3 months of chronological age. Treatment options included nonoperative management or modified MacIntosh,11,12 all-epiphyseal, hybrid, or transphyseal reconstruction (Figure 1).
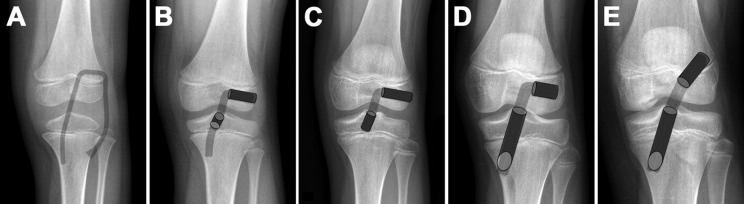
Figure 1.
Diagrammatic representation of techniques included in the survey. (A) Modified MacIntosh procedure. (B, C) Anderson and Lawrence-Ganley all-epiphyseal procedures, respectively. (D) Hybrid reconstruction. (E) Transphyseal reconstruction. (Reprinted with permission from Milewski MD, Beck NA, Lawrence JT, Ganley TJ. Anterior cruciate ligament reconstruction in the young athlete: a treatment algorithm for the skeletally immature. Clin Sports Med. 2011;30(4):801-810. ©2011 Elsevier.19)
The modified MacIntosh, as described by Kocher et al,11,12 consists of a combined intra- and extra-articular reconstruction with iliotibial band autograft. The all-epiphyseal technique includes epiphyseal femoral and tibial tunnels, with similar methods described by Anderson1 and by others.2,15 The hybrid technique is a partial transphyseal reconstruction with an all-epiphyseal femoral tunnel and transphyseal tibial tunnel. Surgeons were also asked their preferred graft for each of these techniques (if they indicated that they used the technique). For each method, respondents were asked the earliest time point after surgery at which they would allow full return to sports, assuming full functional recovery, and the duration for which they prescribe ACL functional bracing after return to sports.
Responses were collected and analyzed independently by nonclinical team members who had no direct input in the initial survey creation. Statistical analysis was performed with the use of SPSS version 20 (IBM Corp). Standard descriptive statistics were used to report demographic data. Each of the aforementioned demographic variables was tested for an association with the preferred technique. Chi-square and Fisher exact tests were used to detect proportional differences for categorical variables, as appropriate. Independent-samples t tests were used in the comparison of means for continuous variables. Statistical significance was defined as P < .05.
Results
Complete survey responses were collected from 88 of 103 respondents (85%). The respondents spanned a well-distributed range of years in practice and geographic locations. All respondents had fellowship training, and the majority of surgeons performed more than 25 pediatric ACL reconstructions annually. Nearly all respondents specialized in pediatric orthopaedics or sports medicine, and 85% had a practice that mostly focused on sports medicine. Detailed demographics are displayed in Table 1.
TABLE 1.
Demographic Characteristics of Survey Respondentsa
| Demographic Characteristic | Finding |
|---|---|
| Age, y, mean ± SD | 43.4 ± 8.4 |
| Sex | |
| Female | 20 (18) |
| Male | 78 (69) |
| Prefer not to answer | 1 (1) |
| Fellowship training | |
| Pediatric orthopaedics only | 40 (35) |
| Sports medicine only | 17 (15) |
| Both pediatric orthopaedics and sports medicine | 40 (35) |
| Other | 3 (3) |
| Years in practice | |
| <5 y | 28 (25) |
| 5-10 y | 33 (29) |
| 11-15 y | 13 (11) |
| >15 y | 26 (23) |
| Practice type | |
| Academic | 65 (57) |
| Hospital group | 14 (12) |
| Mixed academic and private practice | 15 (13) |
| Private practice | 7 (6) |
| Practice location | |
| East Coast | 35 (31) |
| Midwest | 23 (20) |
| South | 20 (18) |
| West Coast | 17 (15) |
| International (outside United States) | 5 (4) |
| Percentage of practice involving pediatric orthopaedics | |
| <25% | 1 (1) |
| 25-50% | 8 (7) |
| 51-75% | 9 (8) |
| >75% | 82 (72) |
| Percentage of practice involving sports medicine | |
| <25% | 1 (1) |
| 25-50% | 14 (12) |
| 51-75% | 34 (30) |
| >75% | 51 (45) |
| Pediatric anterior cruciate ligament reconstructions performed annually | |
| <25 | 32 (28) |
| 25-49 | 44 (39) |
| 50-99 | 15 (13) |
| 100-149 | 9 (8) |
aData are reported as % (n) of respondents, except for age. Any discrepancies in percentages totaling to 100% due to rounding.
Preferred Surgical Technique
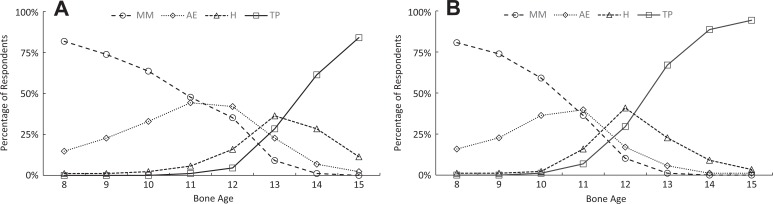
None of the survey respondents chose nonoperative management as a treatment option for any year of skeletal age. Regarding operative management for male patients, the majority of respondents chose the modified MacIntosh technique for patients up to age 10 and a transphyseal reconstruction for those 14 years and older. However, a great deal of variation was found in preferred technique for 11-, 12-, and 13-year-old male patients (Figure 2A). The age of peak use for each reconstruction technique was 8 years for the modified MacIntosh, 11 for all-epiphyseal, 13 for hybrid, and 15 for transphyseal.
Figure 2.
Preferred anterior cruciate ligament reconstruction techniques for (A) male and (B) female patients. AE, all-epiphyseal; H, hybrid; MM, modified MacIntosh; TP, transphyseal.
For female patients, most surgeons chose the modified MacIntosh technique for patients 10 years or younger and a transphyseal reconstruction for those older than 13 years. Significant variation was found in preferred technique for female patients between the ages of 11 and 13 years (Figure 2B). The age of peak use for each reconstruction technique was 8 years for the modified MacIntosh, 11 for all-epiphyseal, 12 for hybrid, and 15 for transphyseal.
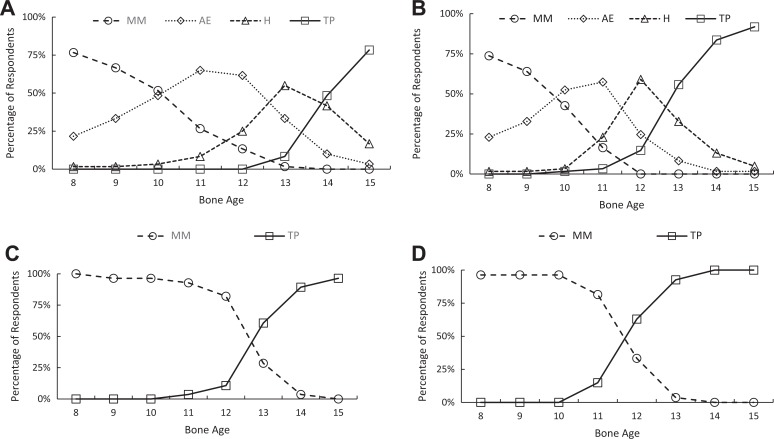
Sixty of the 88 surgeons (68%) chose an all-epiphyseal reconstruction in some age groups. The remainder of surgeons preferred only the modified MacIntosh for younger patients and the transphyseal technique for older ones. To see whether these two groups of surgeons differed in their approach, we analyzed their responses separately. Respondents who used all-epiphyseal techniques selected these procedures over a broader age range (Figure 3, A and B). For both male and female patients, these surgeons preferred the modified MacIntosh for 8- and 9 year-olds, with a nearly equal split between this technique and the all-epiphyseal technique in 10-year-olds. For male patients, the all-epiphyseal technique was favored for 11- and 12-year-olds, and the hybrid reconstruction was favored for 13-year-olds. For 14-year-old male patients, respondents indicated an almost even split between preference for the hybrid technique and the transphyseal technique; however, for 15-year-old male patients, respondents strongly preferred the transphyseal technique. For female patients, respondents favored the all-epiphyseal technique for 11-year-olds and the hybrid technique for 12-year-olds. For female patients 13 years of age, respondents preferred the transphyseal technique, but a significant number of respondents still favored a hybrid technique. The transphyseal technique was strongly preferred for female patients aged 14 and 15 years.
Figure 3.
The selected techniques of surgeons who use all-epiphyseal reconstructions in (A) male and (B) female patients compared with the selections of surgeons who do not perform all-epiphyseal reconstructions in (C) male and (D) female patients. AE, all-epiphyseal; H, hybrid; MM, modified MacIntosh; TP, transphyseal.
In contrast to surgeons who used all-epiphyseal techniques, surgeons who did not use this technique preferred using the modified MacIntosh reconstruction in older patients (Figure 3, C and D). Surgeons who did not use the all-epiphyseal technique also transitioned to the transphyseal technique at a slightly younger patient age than did those who used epiphyseal techniques. These respondents preferred the modified MacIntosh until about age 13 in male patients, after which the transphyseal technique was nearly always selected. This changeover point was slightly earlier in female patients, as the modified MacIntosh was strongly favored for female patients 11 years and younger whereas transphyseal reconstruction was preferred in those 12 years and older.
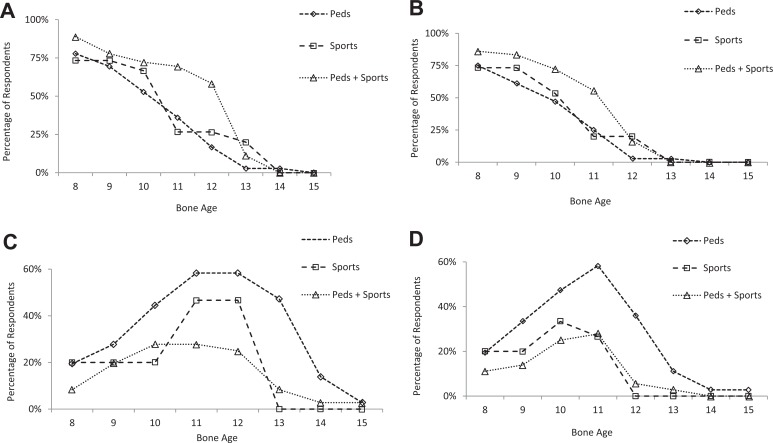
We also assessed the influence of fellowship training type on surgeon preference for the different treatment procedures. Variation in preferred technique for male patients aged 11, 12, and 13 years and female patients aged 11 and 12 years was significantly associated with the type of fellowship training of respondents (P < .05 for all). Surgeons with both pediatric and sports medicine fellowship training heavily favored the modified MacIntosh, while those with a single fellowship appeared to prefer all-epiphyseal reconstruction (Figure 4, A and B). Surgeons with a dual-fellowship background favored the modified MacIntosh more frequently in female patients aged 11 and 12 years, while surgeons with a pediatric fellowship appeared to favor all-epiphyseal reconstruction (P < .01 for both) (Figure 4, C and D). Additionally, the surgeon’s annual volume of ACL reconstructions was significantly associated with chosen reconstruction technique in 14-year-old male patients (P = .02). No other demographic variables were associated with technique preference.
Figure 4.
The percentage of respondents who preferred the modified MacIntosh for (A) male and (B) female patients compared with respondents who selected all-epiphyseal techniques for (C) male and (D) female patients, stratified by fellowship training. Peds, pediatric orthopaedic fellowship only; Sports, sports medicine fellowship only; Peds + Sports, both pediatric orthopaedic and sports medicine fellowships.
Preferred Graft
If respondents indicated on the survey that they would perform a specified surgical technique, they were asked their preferred graft choice (Table 2). Of the respondents, ≤4% noted that they would use an allograft with any of the techniques. Hamstring autograft was the most common choice for all techniques, with bone–patellar tendon–bone autograft reserved mostly for transphyseal reconstruction. No significant differences were found in graft choice for male versus female patients.
TABLE 2.
Graft Preference for Various Anterior Cruciate Ligament Reconstruction Techniquesa
| Graft Type | Male Patients | Female Patients |
|---|---|---|
| All-epiphyseal | ||
| Allograft | 4 (2) | 4 (2) |
| Autograft | 94 (47) | 96 (47) |
| Bone–patellar tendon–bone | 0 (0) | 0 (0) |
| Hamstrings | 85 (40) | 79 (37) |
| Quadriceps | 15 (7) | 17 (8) |
| Hybrid | ||
| Allograft | 2 (1) | 2 (1) |
| Autograft | 98 (43) | 98 (43) |
| Bone–patellar tendon–bone | 2 (1) | 0 (0) |
| Hamstrings | 74 (32) | 79 (34) |
| Quadriceps | 21 (9) | 21 (9) |
| Transphyseal | ||
| Allograft | 1 (1) | 1 (1) |
| Autograft | 99 (74) | 99 (82) |
| Bone–patellar tendon–bone | 11 (8) | 10 (8) |
| Hamstrings | 72 (53) | 73 (60) |
| Quadriceps | 16 (12) | 17 (14) |
aData are reported as % (n) of respondents. Any discrepancies in percentages totaling to 100% due to rounding.
Postoperative Protocol
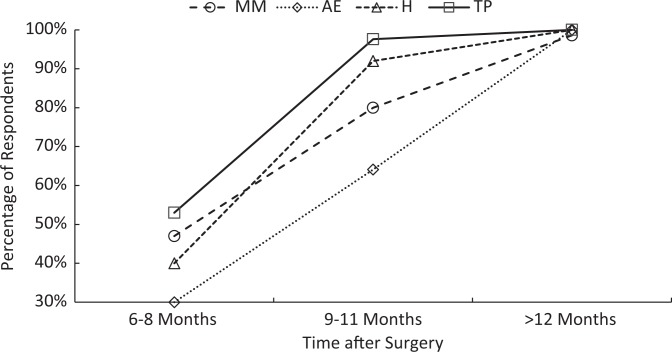
While most surgeons granted their patients clearance for return to sports within 1 year of surgery regardless of technique, a statistically significant difference was noted in protocol when stratified by procedure (Figure 5) (P < .01). Clearance for athletic activity trended toward longer delays for epiphyseal reconstructions.
Figure 5.
The cumulative percentage of respondents who granted their patients clearance for return to sports at 6-8 months, 9-11 months, and >12 months after various anterior cruciate ligament reconstruction techniques. The y-axis begins at 30%. AE, all-epiphyseal; H, hybrid; MM, modified MacIntosh; TP, transphyseal.
Treating physicians were asked about their recommendations for use of functional bracing with return to activities following clearance. Almost three-quarters of the surgeons recommended that patients use a functional ACL brace upon return to athletic activities (Table 3). Duration of bracing was similar for all techniques except the modified MacIntosh, for which 50% of respondents who endorsed bracing recommended it for at least 24 months after surgery.
TABLE 3.
Postoperative Functional Bracing Protocola
| Modified MacIntosh | All- Epiphyseal | Hybrid | Transphyseal | |
|---|---|---|---|---|
| Do not recommend brace | 21 (16) | 29 (29) | 28 (17) | 32 (28) |
| Recommend brace | 79 (61) | 71 (67) | 72 (43) | 68 (60) |
| <12 mo | 16 (10) | 21 (14) | 16 (7) | 23 (14) |
| 12-17 mo | 13 (8) | 25 (17) | 21 (9) | 18 (11) |
| 18-23 mo | 18 (11) | 15 (10) | 23 (10) | 23 (14) |
| ≥24 mo | 52 (32) | 39 (26) | 40 (17) | 35 (21) |
aData are reported as % (n) of respondents. Any discrepancies in percentages totaling to 100% due to rounding.
Discussion
The present study identified current practices in the management of ACL injuries in adolescents at varying skeletal ages from 8 to 15 years. Significant variation was found in the preferred surgical technique for male patients aged 11 through 14 and female patients 11 through 13 years. In these patients, respondents with pediatric orthopaedic training tended to prefer an all-epiphyseal reconstruction, while those with both pediatric and sports medicine training preferred the modified MacIntosh. Overall, the modified MacIntosh was the most commonly used technique in patients aged 8 to 10. The all-epiphyseal technique was preferred over a broader age range in male patients than female patients, with peak use at age 11 in both. The hybrid technique was preferred slightly later, with peak use at age 12 in female patients and 13 in male patients. The transphyseal technique was most widely used in female patients 13 years and older and in male patients 14 years and older.
The treatment of ACL injuries in skeletally immature patients continues to evolve, and this study suggests a possible shift in the approach to these patients over the past 15 years compared with historical data. Prior to the development of physeal-sparing surgical techniques, many surgeons advised nonoperative management or delaying of surgery until skeletal maturity. This preference was highlighted in a survey of the Herodicus Society and ACL Study Group by Kocher et al13 in 2002. In the theoretical case of an 8-year-old patient, only 16% of respondents selected initial operative management, the remainder choosing delayed surgery or nonoperative treatment. When the clinical scenario was changed to a 13-year-old patient, still only 34% of respondents opted for initial surgical management. In the current survey of a similar caliber group of pediatric sports medicine surgeons, although nonoperative treatment was an option, it was never selected. This is likely because numerous studies have described the negative consequences of such a strategy.3,6,7,9,14,20,21,23,24 Lawrence et al14 found that children who underwent reconstruction beyond 3 months after injury had a significantly higher rate of irreparable medial meniscal tears and lateral compartment chondral damage. Moksnes et al21 reported a 19.5% rate of new meniscal injuries in a prospective cohort of 40 skeletally immature children with ACL ruptures treated nonoperatively. Finally, a meta-analysis by Ramski et al24 confirmed that nonoperative and delayed operative treatment resulted in more instability episodes and meniscal tears as well as worse outcome scores. With increasing awareness of these issues and an increase in the incidence of pediatric ACL injuries,5,16,26 a plethora of surgical techniques for skeletally immature patients have been described.
Despite the growing body of literature, little evidence-based consensus is available on the optimal physeal-sparing technique or the ages for which specific procedures are best suited. Kocher et al13 found a high degree of variability in tibial and femoral drilling techniques and graft choice in their 2002 survey. At that time, the majority of respondents preferred transphyseal tunnels with soft tissue grafts for skeletally immature patients.13 In the present study, transphyseal tunnels were typically chosen only for older children; the modified MacIntosh, all-epiphyseal, and hybrid techniques were preferred for the majority of all other age groups. However, the favored procedure for these younger children varied widely among surgeons.
Similarly, the data presented here suggest variation in postoperative protocol. While few surgeons delayed their patients’ return to sports for more than 1 year postoperatively, no consensus was found on clearance earlier than 8 months versus 9 to 12 months. Similarly, although most respondents continued to prescribe functional bracing, the recommended duration varied from 12 to 24 months after surgery. This lack of consensus reflects the current literature, which offers little in the way of evidence-based recommendations. Even in areas for which the literature does provide some evidence, actual clinical practice is highly variable. For example, Dekker et al4 found that earlier return to sport is predictive of a second ACL injury. However, a significant proportion of respondents cleared children for athletic activity at 6 to 8 months after reconstruction.
The results of this study have several implications. While some agreement on how to treat the youngest and oldest patients was found, significant variation was noted regarding management of children in the middle age groups. For these patients, the surgeon’s fellowship training may affect which procedure is chosen, with those who have completed a pediatric fellowship preferring all-epiphyseal reconstruction and those with both pediatric and sports medicine fellowships tending to favor the modified MacIntosh. As demonstrated in Figures 3 and 4, surgeons who performed all-epiphyseal reconstructions appeared to prefer this technique over the modified MacIntosh starting at a younger patient age, around 10 years for both male and female patients. In contrast, those surgeons who did not generally prefer this procedure seemed to select the modified MacIntosh into an older patient age range, up to age 12 in male patients and age 11 in female patients. Interestingly, surgeons with single fellowship training—either pediatrics or sports medicine—appeared to choose the modified MacIntosh and all-epiphyseal techniques for similar age groups, especially in male patients. This is in contrast to surgeons with double fellowship training, who preferred the modified MacIntosh in older patients—more than half of surgeons selected it for 11-year-old female patients and 12-year-old male patients—and never selected the all-epiphyseal technique more than 28% of the time in any age group.
The basis for these findings along the lines of training is unclear. One possibility is that surgeons who are comfortable with a specific technique will stretch its indication across a slightly broader age range. For example, those who are experienced in traditional transphyseal reconstruction may prefer to apply modifications of this technique to younger patients in the form of an all-epiphyseal procedure rather than perform the modified MacIntosh. Similarly, surgeons uncomfortable or unfamiliar with a certain procedure may perform it less frequently by shifting its use to a smaller age group. The reasons behind this phenomenon are surely multifactorial, including not only the surgeon’s overall fellowship background but also specifically which techniques were taught during that training. In any case, future research should aim to further refine indications for the various ACL reconstruction techniques and identify which procedures truly have the best outcomes at various ages.
This study is not without limitations. Because it was based on a survey, it was designed to provide a commentary on current trends and preferences rather than recommendations on surgical technique. Furthermore, surgical decision making is affected by other subtleties and experiences that are beyond the scope of a questionnaire. Finally, since the survey was administered to the PRiSM society, a group of academic surgeons with an interest in sports medicine, the same results may not have been obtained in a query of community surgeons or adult sports medicine surgeons. Nonetheless, the data presented here likely reflect a true lack of consensus in physeal-sparing reconstruction, as PRiSM members are heavily involved in research on the subject and include some of the thought leaders in this area.
Conclusion
The present study describes significant variation in the preferred treatment of skeletally immature patients with ACL injuries. This is especially true for children between the ages of 11 and 13 years. Interestingly, technique preferences were associated with the surgeon’s fellowship training. Future research should aim to provide evidence-based guidelines regarding which procedures will best benefit each age group.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: P.D.F. has received educational support from Smith & Nephew. M.S.K. receives royalties from OrthoPediatrics, is a consultant for OrthoPediatrics, and is a paid speaker/presenter for Smith & Nephew. T.J.G. has received educational support from Arthrex. J.T.R.L. has received educational support from Arthrex and hospitality payments from Liberty Surgical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Children's Hospital of Philadelphia Institutional Review Board.
References
- 1. Anderson AF. Transepiphyseal replacement of the anterior cruciate ligament in skeletally immature patients: a preliminary report. J Bone Joint Surg Am. 2003;85-A(7):1255–1263. [DOI] [PubMed] [Google Scholar]
- 2. Anderson AF. Transepiphyseal replacement of the anterior cruciate ligament using quadruple hamstring grafts in skeletally immature patients. J Bone Joint Surg Am. 2004;86-A(suppl 1, pt 2):201–209. [DOI] [PubMed] [Google Scholar]
- 3. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(2):275–281. [DOI] [PubMed] [Google Scholar]
- 4. Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99(11):897–904. [DOI] [PubMed] [Google Scholar]
- 5. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. [DOI] [PubMed] [Google Scholar]
- 6. Graf BK, Lange RH, Fujisaki CK, Landry GL, Saluja RK. Anterior cruciate ligament tears in skeletally immature patients: meniscal pathology at presentation and after attempted conservative treatment. Arthroscopy. 1992;8(2):229–233. [DOI] [PubMed] [Google Scholar]
- 7. Henry J, Chotel F, Chouteau J, Fessy MH, Berard J, Moyen B. Rupture of the anterior cruciate ligament in children: early reconstruction with open physes or delayed reconstruction to skeletal maturity? Knee Surg Sports Traumatol Arthrosc. 2009;17(7):748–755. [DOI] [PubMed] [Google Scholar]
- 8. Ho B, Edmonds EW, Chambers HG, Bastrom TP, Pennock AT. Risk factors for early ACL reconstruction failure in pediatric and adolescent patients: a review of 561 cases. J Pediatr Orthop. 2018;38(7):388–392. [DOI] [PubMed] [Google Scholar]
- 9. Janarv PM, Nystrom A, Werner S, Hirsch G. Anterior cruciate ligament injuries in skeletally immature patients. J Pediatr Orthop. 1996;16(5):673–677. [DOI] [PubMed] [Google Scholar]
- 10. Kennedy A, Coughlin DG, Metzger MF, et al. Biomechanical evaluation of pediatric anterior cruciate ligament reconstruction techniques. Am J Sports Med. 2011;39(5):964–971. [DOI] [PubMed] [Google Scholar]
- 11. Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg Am. 2005;87(11):2371–2379. [DOI] [PubMed] [Google Scholar]
- 12. Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents: surgical technique. J Bone Joint Surg Am. 2006;88(suppl 1, pt 2):283–293. [DOI] [PubMed] [Google Scholar]
- 13. Kocher MS, Saxon HS, Hovis WD, Hawkins RJ. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of The Herodicus Society and The ACL Study Group. J Pediatr Orthop. 2002;22(4):452–457. [PubMed] [Google Scholar]
- 14. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39(12):2582–2587. [DOI] [PubMed] [Google Scholar]
- 15. Lawrence JT, Bowers AL, Belding J, Cody SR, Ganley TJ. All-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Clin Orthop Relat Res. 2010;468(7):1971–1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91(10):2321–2328. [DOI] [PubMed] [Google Scholar]
- 17. McCarthy MM, Graziano J, Green DW, Cordasco FA. All-epiphyseal, all-inside anterior cruciate ligament reconstruction technique for skeletally immature patients. Arthrosc Tech. 2012;1(2):e231–e239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McCarthy MM, Tucker S, Nguyen JT, Green DW, Imhauser CW, Cordasco FA. Contact stress and kinematic analysis of all-epiphyseal and over-the-top pediatric reconstruction techniques for the anterior cruciate ligament. Am J Sports Med. 2013;41(6):1330–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Milewski MD, Beck NA, Lawrence JT, Ganley TJ. Anterior cruciate ligament reconstruction in the young athlete: a treatment algorithm for the skeletally immature. Clin Sports Med. 2011;30(4):801–810. [DOI] [PubMed] [Google Scholar]
- 20. Mizuta H, Kubota K, Shiraishi M, Otsuka Y, Nagamoto N, Takagi K. The conservative treatment of complete tears of the anterior cruciate ligament in skeletally immature patients. J Bone Joint Surg Br. 1995;77(6):890–894. [PubMed] [Google Scholar]
- 21. Moksnes H, Engebretsen L, Risberg MA. Prevalence and incidence of new meniscus and cartilage injuries after a nonoperative treatment algorithm for ACL tears in skeletally immature children: a prospective MRI study. Am J Sports Med. 2013;41(8):1771–1779. [DOI] [PubMed] [Google Scholar]
- 22. Pierce TP, Issa K, Festa A, Scillia AJ, McInerney VK. Pediatric anterior cruciate ligament reconstruction: a systematic review of transphyseal versus physeal-sparing techniques. Am J Sports Med. 2017;45(2):488–494. [DOI] [PubMed] [Google Scholar]
- 23. Pressman A, Letts R, Jarvis JG. Anterior cruciate ligament tears in children: an analysis of operative versus nonoperative treatment. J Pediatr Orthop. 1997;17(4):505–511. [PubMed] [Google Scholar]
- 24. Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42(11):2769–2776. [DOI] [PubMed] [Google Scholar]
- 25. Redler LH, Brafman RT, Trentacosta N, Ahmad CS. Anterior cruciate ligament reconstruction in skeletally immature patients with transphyseal tunnels. Arthroscopy. 2012;28(11):1710–1717. [DOI] [PubMed] [Google Scholar]
- 26. Werner BC, Yang S, Looney AM, Gwathmey FW., Jr Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36(5):447–452. [DOI] [PubMed] [Google Scholar]
- 27. Yoo WJ, Kocher MS, Micheli LJ. Growth plate disturbance after transphyseal reconstruction of the anterior cruciate ligament in skeletally immature adolescent patients: an MR imaging study. J Pediatr Orthop. 2011;31(6):691–696. [DOI] [PubMed] [Google Scholar]