Abstract
Objectives:
To describe aerobic physical activity among middle-aged and older adults by their self-reported cognitive decline and their receipt of informal care for declines in cognitive functioning and most common type of physical activity.
Design:
Cross-sectional study using data from the 2011 Behavioral Risk Factor Surveillance System.
Setting:
Landline and cellular telephone survey.
Participants:
93,082 respondents aged 45 years and older from 21 US states i in 2011.
Measurements:
Subjective cognitive decline (SCD) was defined as experiencing confusion or memory loss that was happening more often or getting worse during the past 12 months. Regular care was defined as always, usually, or sometimes receiving care from family or friends because of SCD. Using the 2008 Physical Activity Guidelines for Americans, respondents were classified as being inactive, insufficiently active, or sufficiently active based on their reported aerobic exercise. We calculated weighted proportions and used chi-square tests for differences across categories by SCD status and receipt of care. We estimated the prevalence ratio (PR) for being inactive, insufficiently active, and sufficiently active using separate log-binomial regression models, adjusting for covariates.
Results:
12.3% of respondents reported SCD and 23.1% of those with SCD received regular care. 29.6% (95%CI: 28.9–30.4) of respondents without SCD were inactive compared to 37.1% (95%CI: 34.7–39.5) of those with SCD who did not receive regular care and 50.2% (95%CI: 45.2–55.1) of those with SCD who received regular care. 52.4% (95%CI: 51.6–53.2) of respondents without SCD were sufficiently active compared to 46.4% (95%CI: 43.8–49.0) of respondents with SCD and received no regular care and 30.6% (95%CI: 26.1–35.6) of respondents with SCD who received regular care. After adjusting for demographic and health status differences, people receiving regular care for SCD had a significantly lower prevalence of meeting aerobic guidelines compared to people without SCD (PR=0.80, 95%CI: 0.69–0.93, p=0.005). The most prevalent physical activity was walking for adults aged ≥ 45 years old (41–52%) regardless of SCD status or receipt of care.
Conclusion:
Overall, the prevalence of inactivity was high, especially among people with SCD. These findings suggest a need to increase activity among middle-aged and older adults, particularly those with SCD who receive care. Examining ways to increase walking, potentially by involving informal caregivers, could be a promising way for people with SCD to reduce inactivity and gain the health benefits associated with meeting physical activity guidelines.
Keywords: cognitive impairment, physical activity, caregiving, walking
Introduction
Physical activity is a cornerstone of healthy aging [1]. The 2008 Physical Activity Guidelines for Americans recommend that all adults engage in at least 150 minutes per week of moderate-intensity aerobic activity or at least 75 minutes per week of vigorous-intensity aerobic activity to improve health and prevent chronic conditions [30]. Physical activity may prevent falls and fall-related injuries [2] - a major public health concern [3–5] - among community-dwelling older adults (age ≥65). Approximately one-third (30–33%) of older adults fall each year [6–8] which can be due to impairment of balance and gait and lack of muscle strength – risk factors for falls which may be improved by exercise [7]. Furthermore, mounting evidence demonstrates the negative health impacts of a sedentary lifestyle for older adults, including development of chronic conditions such as cardiovascular disease, diabetes, and other metabolic disorders [9–12]. Therefore, increasing physical activity levels may reduce the risk of developing or exacerbating chronic conditions. Based on previous studies of middle-aged and older adults, walking is a common source of physical activity and one in which most people can participate, as highlighted in the recent Step it Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities [13]. Walking has positive effects on physical health and has been associated with better cognitive health in older adults [14, 15].
Cognitive decline, ranging from normative memory loss to dementia including Alzheimer’s disease, affects 6–13% of community-dwelling older adults [5, 16–19]. Cognitively-impaired older adults experience an accelerated reduction of brain volume [3] and impairments of gait and balance [5, 20–23]. While it is not clear whether physical activity can improve cognitive function among people already experiencing cognitive declines [24, 25], being active is an important component of a health-promoting lifestyle for adults with cognitive impairment to improve physical function, manage other chronic health conditions, and reduce the risk of falling.
As community-dwelling adults age and develop physical and/or cognitive impairments, family members or friends often provide support and assistance. Family or informal caregivers contribute approximately 40 billion hours of unpaid services per year which is estimated to be worth $450 billion [26]. The amount of unpaid caregiving services provided is expected to increase as the population of older adults doubles from 31.5 million in 2000 to 71.5 million in 2030 [27]. These informal caregivers could facilitate healthier aging by helping older adults be more physically active; however, it is unclear whether receiving assistance influences the level and frequency of physical activity among adults with cognitive impairment.
The purpose of this study was to examine the association between cognitive impairment and physical activity among community-dwelling middle-aged and older adults. Our objectives are three-fold: 1) report the proportion of middle-aged and older adults who met physical activity guidelines, classified by subjective cognitive decline (SCD) status and by their receipt of informal care because of SCD, 2) assess whether experiencing SCD or receiving care because of SCD were associated with the level of physical activity, and 3) identify the most common types of physical activity.
Methods
Study Sample
We used publicly available data from the 21 US states that included the Cognitive Impairment optional module on the 2011 Behavioral Risk Factor Surveillance System (BRFSS): Arkansas, California, Florida, Hawaii, Illinois, Iowa, Louisiana, Maryland, Michigan, Nebraska, New Hampshire, New York, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Utah, Washington, West Virginia, and Wisconsin. The BRFSS is a population-based annual telephone survey conducted in US states and territories that is designed to assess health status, health conditions, health behaviors, and preventive services utilization among non-institutionalized adults age 18 and older [28]. The BRFSS surveys more than 400,000 people annually who are able to complete the interview, which averages 18 minutes for core questions and 5–10 minutes for additional modules and state-added questions. Interviewers may terminate the survey because “selected respondent [is] physically or mentally unable to complete an interview” (disposition code 260) [29].
Subjective Cognitive Decline Measures
We classified our primary exposure, subjective cognitive decline (SCD), using the following question: “During the past 12 months, have you experienced confusion or memory loss that is happening more often or is getting worse?” Respondents who said yes were classified as having SCD and those who said no were classified as not having SCD. We also classified receipt of SCD-related informal care using the question: “During the past 30 days, how often has a family member or friend provided any care or assistance for you because of confusion or memory loss?” Respondents who said that they always, usually, or sometimes received informal care because of SCD were classified as receiving regular care and respondents who said they rarely or never received informal care or assistance were classified as not receiving regular care.
Physical Activity Measures
We measured physical activity using a series of questions stemming from the following item: “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?” Respondents who said no were classified as inactive. Respondents who said yes were asked to identify up to two activities they spent the most time doing during the past month (“What type of physical activity or exercise did you spend the most time doing during the past month?” and “What other type of physical activity gave you the next most exercise during the past month?”). BRFSS interviewers used a coding list of 69 activities plus an “other” category to classify the activities. For each activity, respondents were asked to respond to the following questions to measure frequency and duration, respectively: (1) “How many times per week or per month did you take part in this activity during the past month?” (2) “And when you took part in this activity, for how many minutes or hours did you usually keep at it?”
The 2008 Physical Activity Guidelines for Americans recommend that all adults, regardless of age, engage in at least 150 minutes per week of moderate-intensity aerobic activity or at least 75 minutes per week of vigorous-intensity aerobic activity, or an equivalent combination thereof, with one minute of vigorous-intensity activity being equivalent to two minutes of moderate-intensity activity [30]. Each activity listed on the BRFSS is assigned a metabolic equivalent (MET) value [31]. We excluded pilates, tai chi, yoga, and weight lifting because they are not classified as aerobic (MET<3.0) [31]. We did not include the “other” category. Vigorous-intensity activity was defined as any activity that was estimated to occur at ≥60% of a person’s maximal oxygen uptake (VO2max), based on their age and sex [31]. For example, vigorous-intensity for a 45 year old woman is ≥5.4 METs and for a 45 year old man is ≥6.0 METs, while for a 65 year old woman it is ≥4.1 METs, and for a 65 year old man it is ≥4.2 METs. If an aerobic activity was ≥3 METs but did not meet the respondent’s age and sex specific vigorous intensity threshold, the activity was classified as moderate-intensity. We included all bouts of aerobic activity of 10 minutes or longer in our calculations of the total minutes of moderate-or vigorous-intensity activity. We calculated aerobic guideline adherence for each respondent using recommendations from the Centers for Disease Control and Prevention [31]. People who reported bouts of aerobic activity but did not meet the guideline threshold were classified as being insufficiently active. As noted above, respondents who reported no leisure time activity were classified as inactive. In addition, respondents who did not have any bouts of aerobic activity longer than 10 minutes were classified as inactive. Respondents who reported ≥150 minutes of moderate intensity activities, ≥75 minutes of vigorous activity, or an equivalent combination, were classified as being sufficiently active; thus, meeting aerobic activity recommendations.
We identified the five most frequent aerobic activities based on the weighted proportion of respondents (aged 45 years and older) who reported each activity. We combined several activities into a single category because the activities and MET values were similar. Specifically, we combined (1) “bicycling” and “bicycling machine exercise” into a single bicycling category; (2) “gardening,” “raking lawn,” “mowing lawn,” and “shoveling snow by hand” into an active housework category; and (3) “running” and “jogging” into a running or jogging category. Additional information is included in Supplementary Table 1.
Covariates
Respondents’ ages were categorized into four mutually exclusive categories (45–54, 55–64, 65–74, and 75 and older). Existing categories for race/ethnicity, marital status, income, and education were collapsed to limit the number of parameters. Having a limitation was defined as experiencing activity limitations due to a physical, mental, or emotional problems or using special equipment such as a cane or wheelchair [32]. Dichotomous variables were created to indicate whether respondents had ever been diagnosed with each of the following chronic health conditions: heart disease (stroke, coronary heart disease, or angina), diabetes (other than gestational diabetes), arthritis, lung disease, cancer (other than skin cancer), and asthma. In addition, we created a variable to indicate whether respondents had at least one of those six conditions. Body mass index (BMI), calculated based on self-reported weight and height, was categorized as underweight (<18.5), normal weight (18.5–24.9), overweight (25.0–29.9), and obese (≥30.0) for respondents age 45–69; for adults age 70 and older, we classified respondents with BMI<22.0 as underweight and with BMI 22.0–24.9 as normal weight (overweight and obese cutpoints were the same for all ages), consistent with European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines [#]. We classified current smokers as those with at least 100 cigarettes in lifetime and currently smoking some days or every day, former smokers as those with 100 cigarettes in lifetime and currently not smoking at all, and never smokers as those with less than 100 cigarettes in lifetime. For all demographic and health status covariates, we created a category for missing responses so that individuals could be retained in regression models. For most variables, <1% of responses were missing except race/ethnicity (1.1–2.1%), annual household income (9.3–12.8%), and BMI (2.6–3.6%).
Statistical Analysis
The Cognitive Impairment module was asked of BRFSS respondents of all ages in 2011 (n=120,792); however, we restricted our analyses to those aged 45 or older (n=93,082) because we were interested in associations among SCD and physical activity for middle-aged and older adults and to enhance comparability of our findings. Also, in subsequent years, the Cognitive Impairment module was administered only to respondents of the BRFSS aged 45 or older. We calculated the weighted proportion of respondents with and without SCD and receipt of care due to SCD by demographic and health status covariates. We used chi-square tests to compare both respondents with and without SCD to those who did and did not receive SCD-related care among respondents with SCD. We also calculated the weighted proportion of respondents who fell into each of the physical activity categories – inactive, insufficiently active, and sufficiently active. We used chi-square tests to compare respondents with and without SCD and also respondents who did and did not receive care for SCD within each of these physical activity categories. We calculated the proportion of respondents in each activity category (inactive, insufficiently active, and sufficiently active) within the four age groups (45–54, 55–64, 65–74, and 75 and older) because we expected activity levels to decline with age and to potentially change differently by SCD status and receipt of care for SCD.
We estimated the prevalence ratios (PR) for being inactive, insufficiently active, and sufficiently active using separate log-binomial regression models (generalized linear models specifying a binomial family and log link) [33]. We chose these models because of the cross-sectional nature of the data and the fact that the outcome (being sufficiently active) is common and, therefore the odds ratio would not provide a good approximation of the relative risk. We adjusted the models for factors associated with SCD and physical activity: age, gender, race/ethnicity, income, limitation status, physical health status, and smoking status. We did not include education or employment because both variables relate closely to income and limitation status. We included both an indicator of chronic conditions and limitation status because these variables reflect different constructs; health conditions do not necessarily equate to limitation and vice versa [34]. However, we did not include BMI because it is strongly associated with both health conditions and limitations and also because it is influenced by physical activity levels, the outcome of interest in this study. However, we did re-run the models within categories of BMI to assess whether the relationships differed by BMI category. We considered models with an interaction term between age category and SCD status and used a p-value of <0.05 to indicate a statistically significant interaction. For other comparisons, comparing proportions or regression model coefficients, we used a Bonferroni-corrected p-value <0.0167 to indicate statistical significance to account for the multiple comparisons (3 categories of physical activity).
Data were weighted using the appropriate weight variable in the BRFSS public data file based on the survey version(s) on which the cognitive impairment module appeared in each state and guidance available on the BRFSS website [35]. We included both landline and cellphone respondents. Seven states included in the module on both their landline and cell phone questionnaires, and the remaining 14 states included the module only on a landline version of the questionnaire. All analyses were conducted using survey (svy) commands with a subpopulation statement to restrict to respondents aged 45 and older and to account for the complex sample design in Stata version 12 (College Station, TX).
Results
Using the 2011 BRFSS dataset, we examined how cognitive impairment correlated with physical activity among community-dwelling middle-aged and older adults. Across 21 US states there were 93,082 respondents aged 45 years or older included in the study; 12.3% (95% confidence interval [CI]: 11.8–12.9) reported experiencing SCD. Among those with SCD, 23.1% (95% CI: 21.2–25.1) reported that they sometimes (15.2%), usually (3.1%), or always (4.8%) received care in the past month because of their SCD (regular care); 10.5% of respondents said they rarely received care and 66.3% said they never received care (76.8% no regular care; 95%CI: 74.9–78.8).
Most demographic and health status characteristics differed across categories of SCD. People with SCD had lower income, educational attainment, and health status and higher BMI and current smoking levels than people without SCD, and people with SCD who received regular care had the lowest levels of income and education and the highest burden of other chronic health conditions and limitations (Table 1).
Table 1.
Demographic, health, and quality of life characteristics of respondents aged 45 years and older by subjective cognitive decline (SCD) status and receipt of regular care for SCD†, Behavioral Risk Factor Surveillance System (BRFSS) 2011.
| Character- istic |
Category | Without SCD (n=82,932) |
With SCD (n=10,150) |
p-value | With SCD | p-value | |
|---|---|---|---|---|---|---|---|
| Receives regular
care for SCD | |||||||
| No (n=7,985) |
Yes (n=2,165) |
||||||
| Age | 45–54 | 37.2% | 36.6% | 0.01 | 34.5% | 43.7% | <0.0001 |
| 55–64 | 29.8% | 28.8% | 28.3% | 30.2% | |||
| 65–74 | 18.4% | 17.3% | 19.1% | 11.5% | |||
| 75+ | 14.6% | 17.3% | 18.2% | 14.6% | |||
| Gender | Female | 52.6% | 53.7% | 0.36 | 53.4% | 54.7% | 0.65 |
| Race/ ethnicity |
White, Non- Hispanic |
71.9% | 67.2% | 0.004 | 69.9% | 58.2% | 0.0001 |
| Black, Non- Hispanic |
9.8% | 9.6% | 0.83 | 8.1% | 14.8% | 0.0001 | |
| Any race, Hispanic |
6.4% | 7.7% | 0.16 | 7.7% | 8.0% | 0.83 | |
| Other
race, Non- Hispanic |
11.1% | 14.2% | 0.002 | 13.5% | 16.9% | 0.18 | |
| Missing | 0.9% | 1.1% | 0.16 | 0.9% | 2.1% | 0.04 | |
| Marital status |
Married or partnered |
62.5% | 50.5% | <0.0001 | 53.8% | 39.5% | <0.0001 |
| Divorced, separated, or widowed |
28.0% | 39.3% | <0.0001 | 36.6% | 48.2% | <0.0001 | |
| Never married |
9.3% | 10.1% | 0.47 | 9.4% | 12.2% | 0.24 | |
| Missing | 0.2% | 0.2% | 0.60 | 0.2% | 0.1% | 0.16 | |
| Educational attainment |
<High school | 14.5% | 23.4% | <0.0001 | 20.5% | 33.0% | <0.0001 |
| High school | 27.8% | 29.1% | 29.0% | 29.4% | |||
| Some college | 30.0% | 29.5% | 30.5% | 26.0% | |||
| College degree or higher |
27.4% | 17.8% | 19.7% | 11.4% | |||
| Missing | 0.2% | 0.2% | 0.2% | 0.2% | |||
| Annual household income |
<$15,000 | 10.2% | 22.3% | <0.0001 | 19.2% | 32.5% | <0.0001 |
| $15,000- $24,999 |
15.2% | 19.8% | 17.2% | 28.5% | |||
| $25,000- $49,999 |
23.1% | 22.9% | 24.9% | 16.2% | |||
| $50,000- $74,999 |
14.2% | 10.8% | 12.5% | 5.2% | |||
| $75,000+ | 26.3% | 14.1% | 16.9% | 4.9% | |||
| Missing | 11.1% | 10.1% | 9.3% | 12.8% | |||
| Employ- ment status |
Currently working |
47.9% | 29.1% | <0.0001 | 34.5% | 11.1% | <0.0001 |
| Not
currently working (including retired) |
44.4% | 44.4% | 0.96 | 48.4% | 31.4% | <0.0001 | |
| Unable to work |
7.4% | 26.2% | <0.0001 | 16.9% | 56.9% | <0.0001 | |
| Missing | 0.3% | 0.3% | 0.89 | 0.2% | 0.6% | 0.22 | |
| Disability status |
Disability | 30.9% | 64.2% | <0.0001 | 57.1% | 87.5% | <0.0001 |
| General health status |
Excellent, very good, or good |
78.2% | 50.7% | <0.0001 | 57.5% | 27.9% | <0.0001 |
| Chronic health conditions |
Heart disease | 12.4% | 25.4% | <0.0001 | 22.6% | 34.7% | <0.0001 |
| Diabetes | 15.7% | 23.0% | <0.0001 | 20.1% | 32.8% | <0.0001 | |
| Arthritis | 36.5% | 59.5% | <0.0001 | 56.4% | 70.0% | <0.0001 | |
| Lung disease | 7.7% | 18.9% | <0.0001 | 16.9% | 25.6% | 0.0001 | |
| Cancer | 10.1% | 13.7% | <0.0001 | 13.6% | 14.0% | 0.02 | |
| Asthma | 11.3% | 20.2% | <0.0001 | 17.5% | 29.2% | <0.0001 | |
| At least one of the six conditions above |
57.2% | 79.1% | <0.0001 | 76.6% | 87.4% | <0.0001 | |
| Body
mass index categoryǂ |
Underweight | 3.9% | 4.9% | <0.0001 | 5.1% | 4.6% | 0.03 |
| Normal | 27.1% | 23.0% | 23.6% | 21.1% | |||
| Overweight | 36.6% | 33.0% | 34.2% | 29.0% | |||
| Obese | 28.8% | 36.4% | 34.5% | 42.7% | |||
| Missing | 3.6% | 2.6% | 2.6% | 2.7% | |||
| Smoking status |
Never | 51.0% | 39.3% | <0.0001 | 40.4% | 35.7% | 0.09 |
| Former | 33.5% | 36.3% | 0.01 | 38.1% | 30.2% | 0.005 | |
| Current | 15.1% | 24.1% | <0.0001 | 21.2% | 33.8% | <0.0001 | |
| Missing | 0.4% | 0.3% | 0.11 | 0.3% | 0.3% | 0.98 | |
Regular care for SCD was defined as always, usually, or sometimes receiving care or assistance in the past 30 days from a family member or friend because of confusion or memory loss.
For adults <70 years old BMI categories were defined as underweight <18.5, normal weight 18.5–24.9, overweight 25.0–29.9, and obese ≥30.0. For adults age 70 years and older, categories were underweight <22.0, normal weight 22.0-, overweight, and obese.
Respondents with SCD were more frequently inactive than respondents without SCD (40.1% versus 29.6%, p<0.0001), and among respondents with SCD, those who received regular care were more inactive than those who did not receive regular care (50.2% versus 37.1%, p<0.0001) (Table 2). The proportion of respondents classified as insufficiently active was similar across groups when classified by their SCD status and receipt of care. Respondents with SCD less frequently were sufficiently active than respondents without SCD (42.8% versus 52.4%, p<0.0001), and those who received regular care for SCD were less likely than those with SCD who did not receive regular care to be sufficiently active (30.6% vs. 46.4%, p<0.0001). These activity patterns were similar within age categories, although among respondents aged 75 or older, there were smaller differences across categories of SCD and receipt of care (Figure 1 and Supplementary Table 2).
Table 2.
Weighted percentage of respondents aged 45 years and older who were inactive, insufficiently active, and sufficiently active based on aerobic activity by subjective cognitive decline (SCD) status and receipt of regular informal care for SCD†, Behavioral Risk Factor Surveillance System (BRFSS) 2011.
| SCD Status | Unweighted count n |
Inactive Weighted % (95% CI) |
Insufficiently Active Weighted % (95% CI) |
Sufficiently Active Weighted % (95% CI) |
|---|---|---|---|---|
| Without SCD | 82,932 | 29.6 (28.9–30.4) |
18.0 (17.4–18.6) |
52.4 (51.6–53.2) |
| With SCD | 10,150 | 40.1* (37.9–42.3) |
17.1 (15.5–18.9) |
42.8* (40.5–45.1) |
| With SCD and no regular informal care |
7,985 | 37.1 (34.7–39.5) |
16.5 (14.7–18.5) |
46.4 (43.8–49.0) |
| With SCD and regular informal care |
2,165 | 50.2§ (45.2–55.1) |
19.2 (15.6–23.4) |
30.6§ (26.1–35.6) |
Regular informal care for SCD was defined as always, usually, or sometimes receiving care or assistance in the past 30 days from a family member or friend because of confusion or memory loss.
p-value for chi-square test comparing people with SCD to people without SCD <0.0167.
p-value for chi-square test comparing people who received regular informal care for SCD to people who did not receive regular informal care for SCD <0.0167.
Figure 1.
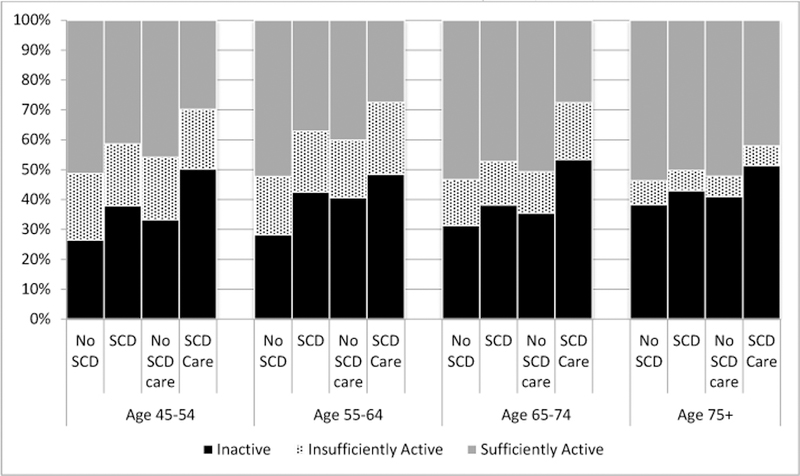
Weighted percentage of respondents who were classified as inactive, insufficiently active, and sufficiently active by self-reported memory loss (SCD) status and receipt of regular informal care for SCD, Behavioral Risk Factor Surveillance System (BRFSS) 2011.
Note: The “No SCD care” and “SCD care” columns are subsets of the “SCD” columns.
In unadjusted models (data not shown), people with SCD had a significantly higher prevalence ratio of being inactive and a significantly lower prevalence ratio of being sufficiently active than people without SCD regardless of whether or not they received care for SCD (inactivity: PR=1.25, 95%CI: 1.17–1.34, p<0.001 for those who did not receive regular care and PR=1.69, 95%CI:1.53–1.88, p<0.001 for those who did receive care; being sufficiently active: PR=0.89, 95%CI 0.84–0.94, p<0.001 for those who did not receive regular care and PR=0.58, 95%CI: 0.50–0.68, p<0.001 for those who did receive care). Although the differences in inactivity and sufficiently activity between people with and without SCD varied somewhat by age, we found no evidence of a statistically significant interaction between age and SCD status in the regression models. After adjusting for age (Table 3), the PRs for inactivity and meeting aerobic guidelines were attenuated slightly compared to the unadjusted values, but statistically significant differences remained for those with SCD compared to those without SCD. In the fully adjusted models, people receiving regular care for SCD were significantly less likely to be sufficiently active (PR=0.80, 95% CI: 0.69–0.94, p=0.005) compared to people without SCD, but there were no differences in inactivity or being insufficiently active to meet guidelines (inactivity: PR=1.11, 95%CI: 1.00–1.24; p=0.044; insufficient activity: PR= 1.00, 95%CI: 0.81–1.23, p=0.99). There were no significant differences in inactivity, insufficient activity, or sufficient activity for people with SCD who did not receive care compared to people without SCD (inactivity: PR=1.03, 95% CI: 0.97–1.10, p=0.32; insufficient activity: PR= 0.93, 95%CI: 0.82–1.05, p=0.25; meeting guidelines: PR=1.01, 95% CI: 0.96–1.07, p=0.68). Results were generally similar within each category of BMI (Supplementary Table 3). Specifically, point estimates for people receiving regular care for SCD indicated they were less likely to be sufficiently active compared to people without SCD regardless of their BMI category.
Table 3.
Association between subjective cognitive decline (SCD) and receipt of care for SCD† with being inactive, insufficiently active, and sufficiently active in adjusted weighted logistic regression models among adults aged 45 years and older, Behavioral Risk Factor Surveillance System (BRFSS) 2011.
| SCD Status | Inactive | Insufficiently Active | Sufficiently Active | |||
|---|---|---|---|---|---|---|
| PR (95%CI) |
p-value | PR (95%CI) |
p-value | PR (95%CI) |
p-value | |
| Age-adjusted models | ||||||
| No SCD | Ref | -- | Ref | -- | Ref | -- |
| SCD without regular care |
1.23 (1.15–1.32) |
<0.001 | 0.94 (0.84–1.07) |
0.35 | 0.88 (0.83–0.94) |
<0.001 |
| SCD with regular care |
1.68 (1.52–1.86) |
<0.001 | 1.02 (0.83–1.26) |
0.82 | 0.59 (0.50–0.68) |
<0.001 |
| Fully-adjusted models§ | ||||||
| No SCD | Ref | -- | Ref | -- | Ref | -- |
| SCD without regular care |
1.04 (0.97–1.10) |
0.32 | 0.93 (0.82–1.05) |
0.25 | 1.01 (0.96–1.07) |
0.68 |
| SCD with regular care |
1.11 (1.00–1.24) |
0.044 | 1.00 (0.81–1.23) |
0.99 | 0.80 (0.69–0.94) |
0.005 |
Regular care for SCD was defined as always, usually, or sometimes receiving care or assistance in the past 30 days from a family member or friend because of confusion or memory loss.
Each model included age, sex, categories of annual household income, an indicator for whether respondents had at least one chronic health condition (arthritis, asthma, cancer, chronic lung disease, diabetes, or heart disease), disability status, and smoking status categories.
PR: prevalence ratio
95%CI: 95% confidence interval
Walking was the most commonly reported activity among all adults aged 45 and older (51.9% of people without SCD and 45.6% of people with SCD, p<0.0001; 46.8% of people with no regular care for SCD and 41.4% of people who received regular care for SCD, p=0.056; Table 4). Other commonly-reported exercise activities were active housework (14.2% of people without SCD and 11.8% of people with SCD, p=0.0014), bicycling (7.8% of people without SCD and 6.9% of people with SCD, p=0.19), running or jogging (4.3% of people without SCD and 2.5% of people with SCD, p=0.0006), and aerobics or video class (3.0% of people without SCD and 1.8% of people with SCD, p=0.001). For all activities, the percentage of respondents engaging in the activity was highest among people without SCD and lowest for people with SCD who received regular care.
Table 4.
Weighted percentage of respondents aged 45 years and older who reported an activity* by subjective cognitive decline (SCD) status and receipt of regular care for SCD†, Behavioral Risk Factor Surveillance System (BRFSS) 2011.
| Activity or Activity Category | |||||
|---|---|---|---|---|---|
| SCD Status | Walking | Active housework§ |
Bicycling | Running or Jogging |
Aerobics video or class |
| Weighted % (95% CI) | |||||
| Without SCD | 51.9 (51.1–52.7) |
14.2 (13.7–14.7) |
7.8 (7.4–8.2) |
4.3 (4.0–4.7) |
3.0 (2.8–3.2) |
| With SCD | 45.6ǂ (43.3–47.9) |
11.8ǂ (10.5–13.1) |
6.9 (5.8–8.2) |
2.5ǂ (1.9–3.4) |
1.8ǂ (1.3–2.4) |
| With SCD and no regular informal care |
46.8 (44.2–49.4) |
13.2 (11.7–14.8) |
7.6 (6.3–9.2) |
3.1 (2.3–4.3) |
2.0 (1.4–2.9) |
| With SCD and regular informal care |
41.4 (36.6–46.3) |
7.2¶ (5.2–9.7) |
4.5 (2.9–6.9) |
0.5¶ (0.2–1.5) |
1.0 (0.6–1.8) |
Respondents could identify up to two activities they did most frequently in the past month.
Regular informal care for SCD was defined as always, usually, or sometimes receiving care or assistance in the past 30 days from a family member or friend because of confusion or memory loss.
Active housework includes gardening, raking, mowing, and shoveling snow.
p-value for chi-square test comparing people with SCD to people without SCD <0.0167.
p-value for chi-square test comparing people who received regular informal care for SCD to people who did not receive regular informal care for SCD <0.0167.
Discussion
Using population-based data from community-dwelling middle-aged and older adults in 21 states, we found that people with SCD were more likely to be physically inactive and less likely to be sufficiently active (meet physical activity guidelines for aerobic activities) than people without SCD, particularly if they reported receiving regular SCD-related informal care. After accounting for demographic and health differences, people with SCD who received informal care had lower levels of sufficient activity than people without SCD. Previous studies have also documented less physical activity among older adults with SCD, including walking. For example, Prohaska and colleagues found that older adults with cognitive impairment participated in neighborhood walking less frequently than those with no cognitive impairment [14]. We also found that walking was the most commonly reported activity across all groups; however, people with SCD were significantly less likely to report walking than people without SCD.
Overall, the proportion of middle-aged and older adults meeting guidelines for aerobic activity was low, consistent with previous population-based studies. People with SCD were particularly likely to be inactive. This underscores a need to improve aerobic physical activity among middle-aged and older adults with SCD. Higher levels of physical activity may reduce further cognitive decline or prevent or control chronic diseases such as hypertension, which also are associated with cognitive decline [36]. Increasing activity levels among people with SCD who receive care could also help improve the prevalence and progression of chronic disease, which could be particularly important given the high burden of chronic conditions observed in this study.
The most commonly reported physical activity across all respondents regardless of SCD status and receipt of informal care for SCD was walking. A recent study by Szanton and colleagues found that walking/jogging was the most favored activity among older adults [37]. Hence, one potential strategy to improve physical activity and to reap the health benefits of physical exercise among older adults with and without SCD is to encourage walking. The 2008 Physical Activity Guidelines for Americans [30] and Healthy People 2020 [38] recommended increased walking among middle-aged and older adults. The Surgeon General’s recent Call to Action released in 2015 Step it Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities [13] promotes environments that include safe and convenient places to walk for people of all ages and abilities across the U.S. Walking has physical health benefits as well as may have association with better cognitive health of older adults such as delaying the onset and progression of dementia [14, 15]. In response to these national calls for action, as well as from the results of this study, our paper will focus on how we can incorporate walking into our daily lifestyle as one tool to improve the well-being of the target populations.
Walking is the most commonly reported activity among middle-aged and older adults; however, people who are interested in walking may face some barriers to walking. Environmental barriers such as uneven surfaces, traffic, lack of resting places, poor lighting, crime, and weather are some of the challenges that may prevent older adults from walking in their neighborhoods [39–42]. Additionally, the fear of getting lost is a barrier to walking for some, and may be particularly important for people with SCD. Wayfinding, “the process of finding our way from place to place” [43, p. 5], can be particularly difficult for those with SCD [43–45]. Wayfinding utilizes environmental cues such as clear street signs and large landmarks [44]. Marquez and colleagues found a high percentage of older adults relying on others for directions and wayfinding assistance in unfamiliar places [44], suggesting that having someone to provide assistance with wayfinding – a caregiver or community member – could make it easier for older adults with SCD improve their opportunities for walking. However, research is limited on both the use of assistance for wayfinding and interventions to improve wayfinding for middle-aged and older adults with cognitive decline.
Walking in shopping malls may provide fewer potential barriers for middle-aged and older adults with SCD and can be a preferred walking site for older adults [46]. Prohaska and colleagues found that older adults with SCD tended to walk in shopping malls or indoor gyms more often compared to outside facilities such as parks or trails; further, older adults with SCD less frequently walked in neighborhoods compared to those without SCD [14]. Malls have fewer environmental barriers to walking because they have climate control, even surfaces, relative safety, good lighting, and accessible features (e.g., resting places, water fountain, restrooms, attached parking spaces) [47, 48]. Organized mall walking programs found throughout the U.S. can also provide social support such as making new friends by joining the mall walking programs as walkers become walking buddies, a potential facilitator of physical activity [47, 49].
In terms of caregiver’s involvement, the receipt of informal care due to SCD can positively impact peoples’ functioning including physical functioning [50–54]. For example, several randomized control studies involving walking programs with Alzheimer’s patients assisted by care workers in nursing homes have shown an increasing exercise time [55, 56]. Teri and colleagues in their longitudinal randomized control study successfully showed positive physical health and depression effects for adults with Alzheimer’s disease and their caregiver dyads utilizing a home-based exercise program combined with caregiver training in behavioral management techniques [54]. Nonetheless, in our study, after adjusting for health status and limitation, people receiving SCD-related care had a lower prevalence of meeting physical activity guidelines. It is not clear if this is due to residual confounding by functional status (i.e., people who need care have higher levels of physical and cognitive impairment) or if caregivers need help or training to increase physical activity among care recipients with SCD. However, given the physical health benefits in adults with SCD, due to caregiver’s involvement shown in previous studies [54], having the caregivers trained and working as dyads can be considered when developing walking training programs for people with SCD and caregivers. Most of all, caregivers can remind care recipients with SCD of daily exercise. In addition, if caregivers can accompany and walk together on a regular basis, that would be beneficial to both caregivers and care recipients in maintaining the recommended amount of physical activity per week.
There are several limitations to this study. First, the BRFSS is a cross-sectional survey and relies upon self-report for both SCD experience and reported physical activity. Although the cognitive impairment module was cognitively tested and piloted, the SCD measure has not been validated with clinical symptoms or measures of mild cognitive impairment. The cognitive status of respondents who experienced SCD may result in additional errors in reporting the physical activity level [57]. However, all BRFSS respondents must be capable of completing the interview and there were no differences in the proportion of missing responses among people with SCD compared to those without SCD. It is likely that people who completed the BRFSS survey have less cognitive impairment than people who were excluded from the survey or chose not to participate, and therefore, these findings may not extend to all people with cognitive impairment. The BRFSS also is limited to non-institutional settings so middle-aged and older adults living in nursing homes or other congregate care facilities were not included. Approximately 4% of older adults live in an institutional setting and another 2% live in senior housing [58]. Therefore, these results may not represent the levels of activity among people with and without SCD in congregate care settings. Finally, the 2008 Physical Activity Guidelines for Americans recommends regular strength training in addition to aerobic activity. Although the BRFSS includes a question about strength training, we focused only on aerobic activity in this study.
Conclusion
This study examined the association between physical activity and cognitive impairment in relation to care receipt status using a large population-based sample of community-dwelling middle-aged and older adults. Physical activity is important for all adults at any age. Walking was the most preferred physical activity among middle-aged and older adults and can potentially delay progression of cognitive impairment. Employing strategies outlined in the Surgeon General’s Call to Action to Promote Walking and Walkable Communities can enhance access to walkable environments, which can promote walking and create a culture of walking for everyone with various levels of physical and cognitive abilities. This may be of particular importance for older adults with SCD as they are involved in fewer physical activities. Understanding the specific needs and barriers to physical activity for older adults with SCD and their caregivers is a vital area for future research. This work can inform public health interventions and bring us closer to all middle-aged and older adults becoming more active and toward meeting the physical activity guidelines for Americans.
Supplementary Material
Acknowledgments
Funding
This project is the result of work conducted by the Centers for Disease Control and Prevention (CDC) Healthy Brain Research Network. The CDC Healthy Brain Research Network is a Prevention Research Centers program funded by the CDC Healthy Aging Program-Healthy Brain Initiative. This project was supported in part by cooperative agreements from CDC’s Prevention Research Centers Program: U48 DP 005013. Miyawaki was funded by the T32 Women’s Health Postdoctoral Fellowship, National Institutes of Health (NIH), through Grant AG027677 as well as the Michigan Public Health Institute (MPHI), Grant I-98113–117. Bouldin was supported by a Department of Veteran’s Affairs Health Services Research & Development post-doctoral fellowship. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC, NIH, VA, or MPHI.
Footnotes
Ethical Standards
This study was reviewed by the University of Houston Institutional Review Board and determined to be exempt as a minimal risk study.
Conflict of Interest
The authors declare no conflict of interest.
Contributor Information
Christina E. Miyawaki, Graduate College of Social Work, University of Houston, Houston, TX.
Erin D. Bouldin, VA Puget Sound Health Care System, Seattle, WA, Department of Health Services, University of Washington, Seattle, WA.
Gayathri Suresh Kumar, Division of Nutrition, Physical Activity, and Obesity, Centers for Disease Control and Prevention, Atlanta, GA.
Lisa C. McGuire, Healthy Aging Program, Centers for Disease Control and Prevention, Atlanta, GA.
References
- 1.The National Institute of Aging (NIA) (2015). https://www.nia.nih.gov/health/publication/healthy-aging-lessons-baltimore-longitudinal-study-aging/what-does-all-mean-you. Accessed 9 January 2016
- 2.Sun F, Norman IJ, While AE (2013) Physical activity in older people: a systematic review. BMC Public Health 13:449 10.1186/1471-2458-13-449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Makizako H, Shimada H, Doi T, Park H, Yoshida D, Uemura K, Tsutsumimoto K, Liu-Ambrose T, Takao Suzuki T (2013) Poor balance and lower gray matter volume predict falls in older adults with mild cognitive impairment. BMC Neurology 13:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Winter H, Watt K, Peel NM (2013) Falls prevention interventions for community-dwelling older persons with cognitive impairment: a systematic review. Int Psychogeriatr 25(2):215–227 [DOI] [PubMed] [Google Scholar]
- 5.Taylor ME, Delbaere K, Lord SR, Mikolaizak AS, Close JCT (2013) Physical impairments in cognitively impaired older people: implications for risk of falls. Int Psychogeriatr 25(1):148–156 [DOI] [PubMed] [Google Scholar]
- 6.Morris MT (2001) Epidemiology of falls. Age Ageing 30(Suppl4):3–7 [DOI] [PubMed] [Google Scholar]
- 7.Muir SW, Gopaul K, Montero-Odasso MM (2012) The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing 41(3):299–308 [DOI] [PubMed] [Google Scholar]
- 8.Tinetti ME, Kumar C (2010) The patient who falls: “It’s always a trade-off”. JAMA 303:258–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Proper KI, Singh AS, van Mechelen W, Chinapaw MJ (2011) Sedentary behaviors and health outcomes among adults: a systematic review of prospective studies. Am J Prev Med 40(2):174–182 [DOI] [PubMed] [Google Scholar]
- 10.Thorp AA, Owen N, Neuhaus M, Dunstan DW (2011) Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med 41(2):207–215 [DOI] [PubMed] [Google Scholar]
- 11.Edwardson CL, Gorely T, Davies MJ et al. (2012) Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PLoS One 7(4):e34916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev 2010;38:105–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.U.S. Department of Health and Human Services (DHHS) (2015) The Surgeon General’s recent Call to Action released in 2015 (‘Step it Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities) Accessed http://www.surgeongeneral.gov/library/calls/walking-and-walkable-communities/ [PubMed] [Google Scholar]
- 14.Prohaska TR, Eisenstein AR, Satariano WA, Hunter R, Bayles CM, Kurtovich E, Kealey M, Ivey SL (2009) Walking and the preservation of cognitive function in older populations. Gerontologist 49(S1):S86–S93. 10.1093/geront/gnp079 [DOI] [PubMed] [Google Scholar]
- 15.Abbott RD, White LR, Ross GW, Masaki KH, Curb JD, Petrovitch H (2004) Walking and dementia in physically capable elderly men. JAMA 292:1447–1453 [DOI] [PubMed] [Google Scholar]
- 16.Adams ML, Deokar AJ, Anderson LA, Edwards VJ (2013) Self-reported increased confusion or memory loss and associated functional difficulties among adults aged ≥60 years - 21 States, 2011. MMWR 62(18):347–350. [PubMed] [Google Scholar]
- 17.Alzheimer’s Disease International: World Alzheimer’s Report 2010 (2011) The global economic impact of dementia. London 52 Available from: http://www.alz.co.uk/research/files/WorldAlzheimerReport2010.pdf
- 18.Wimo A, Prince M. (2010). World Alzheimer report 2010: the global economic impact of dementia. Alzheimer’s Disease International
- 19.Shaw FE, Kenny RA (1998) Can falls in patients with dementia be prevented? Age Ageing 27:7–9 [DOI] [PubMed] [Google Scholar]
- 20.Boyle PA, Wilson RS, Buchman AS, et al. (2007) Lower extremity motor function and disability in mild cognitive impairment. Exp Aging Res 33:355–371 [DOI] [PubMed] [Google Scholar]
- 21.Pettersson AF, Olsson E, Wahlund LO (2005) Motor function in subjects with mild cognitive impairment and early Alzheimer’s disease. Dement Geriatr Cogn Disord 19:299–304. [DOI] [PubMed] [Google Scholar]
- 22.Tangen CG, Engedal K, Bergland A, Moger TA, Mengshoel AM (2014) Relationships between balance and cognition in patients with subjective cognitive impairment, mild cognitive impairment, and Alzheimer disease. Physical Therapy 94(8); 1123–1134 [DOI] [PubMed] [Google Scholar]
- 23.Waite LM, Broe GA, Grayson DA, Creasey H (2000) Motor function and disability in the dementias. Int. J. Geriatr. Psychiatry 15:897–903 [DOI] [PubMed] [Google Scholar]
- 24.Young J, Angevaren M, Rusted J, Tabet N (2015) Aerobic exercise to improve cognitive function in older people without known cognitive impairment. Cochrane Database of Systematic Reviews 4 10.1002/14651858.CD005381.pub4 [DOI] [PMC free article] [PubMed]
- 25.Angevaren M, Aufdemkampe G, Verhaar HJJ, Aleman A, Vanhees L (2008) Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database of Systematic Reviews 2 10.1002/14651858.CD005381.pub2 [DOI] [PubMed]
- 26.Feinberg L, Reinhard SC, Houser A, Choula R (2011) Valuing the invaluable: 2011 update, the growing contributions and costs of family caregiving AARP Public Policy Institute Insight 51 Washington, DC: AARP. [Google Scholar]
- 27.Coughlin J (2010) Estimating the impact of caregiving and employment on well-being. Outcomes & Insights in Health Management 2(1) [Google Scholar]
- 28.Mokdad AH (2009) The Behavioral Risk Factor Surveillance System: past, present, and future. Annu Rev Public Health 30:43–54 [DOI] [PubMed] [Google Scholar]
- 29.BRFSS. Summary Data Quality Report, Version #5--Revised: 2/04/2013. 2011 http://www.cdc.gov/brfss/annual_data/2011/pdf/2011_summary_data_quality_report.pdf. Accessed 2 October 2015.
- 30.U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion (2008) Physical Activity Guidelines for Americans, October 2008. ODPHP Publication No. U0036. http://health.gov/paguidelines/pdf/paguide.pdf. Accessed August 19, 2015.
- 31.CDC Division of Nutrition, Physical Activity, and Obesity. A data users guide to the BRFSS physical activity questions: how to assess the 2008 physical activity guidelines for Americans http://www.cdc.gov/brfss/pdf/PA%20RotatingCore_BRFSSGuide_508Comp_07252013FINAL.pdf. Accessed August 19, 2015.
- 32.Centers for Disease Control and Prevention (2015). Disability and Health Data System. Data Guide – Limitation Status Available at http://dhds.cdc.gov/guides/limitation
- 33.Barros AJ, Hirakata VN (2003) Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization; Towards a Common Language for Functioning, Disability and Health Geneva, Switzerland; 2002. Available at: http://www.who.int/classifications/icf/icfbeginnersguide.pdf?ua=1. Accessed 22 January 2016 [Google Scholar]
- 35.CDC Division of Behavioral Surveillance (2013) Preparing 2011 BRFSS module data for analysis http://www.cdc.gov/brfss/annual_data/2011/pdf/brfss2011_analysis.pdf. Accessed 19 August 2015
- 36.Daviglus ML, Bell CC, Berrettini W, Bowen PE, Connolly ES Jr., Cox NJ, Dunbar-Jacob JM, Granieri EC, Hunt G, McGarry K, Patel D, Potosky AL, Sanders-Bush E, Silberberg D, Trevisan M (2010) National Institutes of Health State-of-the-Science Conference Statement: Preventing Alzheimer Disease and cognitive decline. Ann Intern Med 153:176–181 [DOI] [PubMed] [Google Scholar]
- 37.Szanton SL, Walker RK, Roberts L, Thorpe RJ, Wolff J, Agree E, Roth DL, Gitlin LN, Seplaki C (2015) Older adults’ favorite activities are resoundingly active: findings from the NHATS study. Geriatric Nursing 36(2):131–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.<au>U.S. Department of Health</au> and Human Services. Healthy People 2020 (2010) Available at http://www.healthypeople.gov/
- 39.Clarke P, Ailshire JA, Lantz P (2009) Urban built environments and trajectories of mobility disability: Findings from a national sample of community-dwelling American adults (1986–2001). Social Science & Medicine 69(6):964–970. 10.1016/j.socscimed.2009.06.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.King D (2008) Neighborhood and individual factors in activity in older adults: results from the neighborhood and senior health study. J Aging Phys Act 16:144–170 [DOI] [PubMed] [Google Scholar]
- 41.Rosenberg DE, Huang DL, Simonovich SD, Belza B (2013) Outdoor built environment barriers and facilitators to activity among midlife and older adults with mobility disabilities. Gerontologist 53(2):268–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li W, Keegan TH, Sternfeld B, Sidney S, Quesenberry CP Jr., Kelsey JL (2006) Outdoor falls among middle-aged and older adults: a neglected public health problem. [Research Support, N.I.H., Extramural]. Am J Public Health 96(7):1192–1200. 10.2105/AJPH.2005.083055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hunter RH, Potts S, Beyerle R, Stollof E, Lee C, Duncan R, Vandenberg A, Belza B, Marquez DX, Friedman DB, Bryant LL (2013) Pathways to better community wayfinding. Seattle, WA; Washington, DC: CDC Healthy Aging Research Network and Easter Seals Project ACTION; http://www.prc-han.org. [Google Scholar]
- 44.Marquez DX, Hunter RH, Griffith MH, Brynant LL, Janicek SJ, Atherly AJ (2015) Older adult strategies for community wayfinding. J Appl Gerontol doi: 0733464815581481 [DOI] [PubMed]
- 45.Vandenberg AE, Hunter RH, Anderson LA, Bryant LL, Hooker S, Satariano W (2015) Walking and walkability: is wayfinding a missing link? Implications for public health practice. J Phys Act Health May 12. [DOI] [PMC free article] [PubMed]
- 46.Eyler AA, Brownson RC, Bacak SJ, Housemann RA (2003) The epidemiology of walking for physical activity in the United States. Med Sci Sports Exerc 35(9):1529–36 [DOI] [PubMed] [Google Scholar]
- 47.Belza B, Allen P, Brown DR, Farren L, Janicek S, Jones DL, King DK, Marquez DX, Miyawaki CE, Rosenberg D (2015) Mall walking: a program resource guide Seattle, WA: University of Washington Health Promotion Research Center; 2015. Available at http://www.cdc.gov/physicalactivity/downloads/mallwalking-guide.pdf [Google Scholar]
- 48.Duncan HH, Travis SS, McAuley WJ (1995) An emergent theoretical-model for interventions encouraging physical-activity (mall-walking) among older adults. J Appl Gerontol 14(1):64–77 [Google Scholar]
- 49.Farren L, Belza B, Allen P, Brolliar S, Brown DR, Cormier SCD et al. (2015) Mall walking program environments, features, and participants: a scoping review. Prev Chronic Dis 12:150027 10.5888/pcd12.150027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arkin SM (1999) Elder rehab: a student-supervised exercise program for Alzheimer’s patients. Gerontologist 39(6):729–735 [DOI] [PubMed] [Google Scholar]
- 51.Arkin SM (2003) Student-led exercise sessions yield significant fitness gains for Alzheimer’s patients. Am J Alzheimer Dis Other Demen 18(3):159–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Heyn P, Abreu B, Ottenbacher K (2004) The effects of exercise training on elderly persons with cognitive impairment and dementia: a meta-analysis. Arch Phys Med Rehabil 85:1694–1704 [DOI] [PubMed] [Google Scholar]
- 53.Logsdon RG, McCurry SM, Teri L (2005) A home health care approach to exercise for persons with Alzheimer’s disease. Care Manag J 6(2):90–97 [DOI] [PubMed] [Google Scholar]
- 54.Teri L, Gibbons LE, McCurry SM et al. (2003). Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial. JAMA 290(15):2015–2022 [DOI] [PubMed] [Google Scholar]
- 55.Venturelli M, Scarsini R, Schen F (2011) Six-month walking program changes cognitive and ADL performance in patients with Alzheimer. Am J Alzheimers Dis Other Demen 26(5):381–388. 10.1177/1533317511418956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tappen RM, Roach KE, Applegate EB, Stowell P (2000) Effect of a combined walking and conversation intervention on functional mobility of nursing home residents with Alzheimer Disease. Alzheimer Dis Assoc Disord 14(4):196–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Farias ST, Mungas D, Jaqust W (2005) Degree of discrepancy between self and other-reported everyday functioning by cognitive status: dementia, mild cognitive impairment, and healthy elders. Int J Geriatr Psychiatry 20(9):827–834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Administration on Aging. A Profile of Older Americans: 2011. Available at: http://www.aoa.acl.gov/Aging_Statistics/Profile/2011/6.aspx. Accessed 22 January 2016
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


