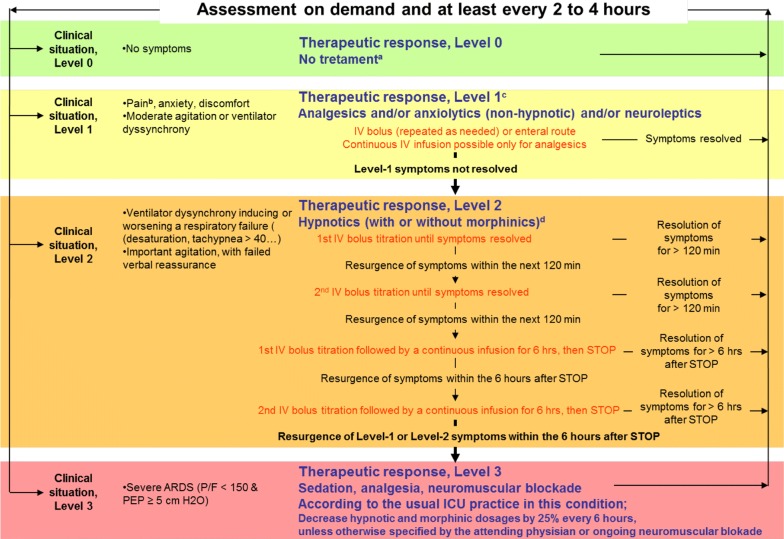
Fig. 1.
Oversedation prevention (OSP) strategy was centred on patients’ level of agitation, ventilator dyssynchrony, and pain, assessed on a 4-level scale, with gradual on-demand responses, frequent reassessments, and promotion of alternatives to continuous around-the-clock infusion of intravenous hypnotics. These alternatives included frequent (every 6 h) intravenous hypnotic interruptions, intravenous boluses of hypnotics without continuous intravenous infusion, and the use of non-hypnotic drugs, including neuroleptics, hydroxyzine, and anxiolytic benzodiazepines. The choice of the non-hypnotic drugs and their route of administration (intravenous boluses or nasogastric tube) were left to the preference of the attending physician. There was no restriction for the use of morphinics and non-morphinic analgesics. Patient at Level 0, who showed no discomfort, received no treatment, or continuation of a successful level-1 therapeutic response (a). Patient at Level 1, with only moderate discomfort, pain, or anticipated procedural pain (b), received any form of analgesics as deemed necessary by the attending physician and/or non-hypnotic drugs as well as verbal reassurance and, if appropriate, changing of ventilator settings (c). Patients at Level 2, with severe agitation or ventilator dyssynchrony first received repeated intravenous boluses of either propofol or midazolam according to physician preferences, and, if discomfort persisted, 6-h continuous intravenous infusion of midazolam or propofol. This treatment was also applied in case of Level 1 therapy failure (which was maintained or stopped according to physician preference (d). Patients at Level 3, with ARDS and a PaO2/FiO2 ratio < 150 mmHg, were treated with a continuous intravenous infusion of midazolam or propofol, with neuromuscular blocking agents administered according to physician preference. This treatment was also applied in the case of Level 2 therapy failure