Abstract
Objective
To evaluate impacts of state Medicaid expansions for low‐income parents on the health insurance coverage, pregnancy intention, and use of prenatal care among mothers who became pregnant.
Data Sources/Study Setting
Person‐level data for women with a live birth from the 1997–2012 Pregnancy Risk Assessment Monitoring System.
Data Collection/Extraction Methods
The sample was restricted to women who were already parents using information on previous live births and combined with information on state Medicaid policies for low‐income parents.
Study Design
I used a measure of expanded generosity of state Medicaid eligibility for low‐income parents to estimate changes in health insurance, pregnancy intention, and prenatal care for pregnant mothers associated with Medicaid expansion.
Principal Findings
I found an increase in prepregnancy health insurance coverage and coverage during pregnancy among pregnant mothers, as well as earlier initiation of prenatal care, associated with the expansions. Among pregnant mothers with less education, I found an increase in the adequacy of prenatal care utilization.
Conclusions
Expanded Medicaid coverage for low‐income adults has the potential to increase a woman's health insurance coverage prior to pregnancy, as well as her insurance coverage and medical care receipt during pregnancy.
Keywords: Medicaid, health insurance, pregnancy, prenatal care, Pregnancy Risk Assessment Monitoring System
The United States continues to lag behind other developed countries with high rates of infant mortality (MacDorman et al. 2014). This poor performance is primarily driven by worse infant health among lower socioeconomic groups (Chen, Oster, and Williams 2016). There is growing recognition that interventions to improve infant health may need to shift attention to the prepregnancy, or preconception, period (Floyd et al. 2013). While early and regular prenatal care visits are important for identifying and managing risks during pregnancy, maternal risk factors associated with poor pregnancy outcomes, such as chronic disease and substance abuse, often begin years before conception.
Expanding health insurance coverage and promoting the health of women of childbearing age prior to or between pregnancies, particularly among lower income women, may help mitigate poor pregnancy outcomes. Women with health insurance coverage are more likely to access needed medical care and receive screenings for health conditions (Salganicoff and Wyn 1999; Salganicoff, Ranji, and Wyn 2005). In addition, women with prepregnancy insurance coverage are less likely to have an unintended pregnancy and more likely to establish early prenatal care when compared to women without insurance (Rosenberg et al. 2007; Norwood 2014). Not only are women with lower incomes less likely than higher income women to have health insurance coverage prior to pregnancy (Adams et al. 2003), they are more likely to be in poor health and have chronic health conditions (Aizer and Currie 2014), more likely to have unintended births (Mosher, Jones, and Abma 2012), and less likely to receive timely and adequate prenatal care (McDonald and Coburn 1988; Centers for Disease Control and Prevention 2000). Increasing insurance coverage for low‐income women was one of the 10 recommendations issued by the Centers for Disease Control and Prevention (CDC) in 2006 to improve national preconception health (Johnson et al. 2006).
The Affordable Care Act (ACA) changed the insurance options available to low‐income women, with expectations to have major consequences for access to preconception health care and health going forward (Lu and Johnson 2014). While all states have been required to provide pregnancy‐related Medicaid coverage to pregnant women with incomes below 133 percent of the federal poverty line (FPL) since 1990, Medicaid eligibility for other women has primarily been limited to mothers with dependent children with very low income levels and no eligibility pathway for women without children. This left many low‐income women without access to insurance coverage during the periods when they were not pregnant. This has been changing under the ACA with 31 states and the District of Columbia opting to expand Medicaid for low‐income adults (Kaiser Family Foundation 2016). In these states, women with incomes below 138 percent FPL are now eligible for Medicaid coverage regardless of their pregnancy status. And, in all states, women with incomes between 138 and 400 percent FPL (or between 100 and 400 percent FPL in states not expanding Medicaid) are eligible for subsidized coverage through new marketplaces established under the ACA.
The data are not yet available to evaluate the consequences of the ACA Medicaid expansions on patterns of health insurance coverage and health care utilization prior to pregnancy. However, we are able to evaluate the consequences of state decisions to expand Medicaid coverage for certain low‐income adults prior to the ACA. Findings from the study of prior state expansions are relevant because they offer a preview for changes that we may later observe under the ACA expansions. In this way, evidence from prior expansions is valuable for states that may still consider expanding Medicaid for low‐income adults. The findings are also relevant as, in states choosing not to expand Medicaid under the ACA or if state options for these expansions change going forward, existing state decisions regarding their Medicaid programs are likely to critically affect the prepregnancy insurance options available to low‐income women.
In this study, I examine the impact of pre‐ACA state Medicaid expansions for low‐income parents on insurance coverage before pregnancy among women who were already mothers. The majority of low‐income pregnant women already have children, and their eligibility for Medicaid coverage prior to their pregnancy, therefore, depends on the eligibility rules for parents in their state.1 Although all states cover some parents under Medicaid, the eligibility thresholds have historically been very low (about 41 percent FPL on average). National welfare reform in 1996 provided states with options to expand eligibility for parents and, by 2000, many states had taken advantage of this flexibility (Kaiser Family Foundation 2002). In addition, a handful of states implemented expansions for low‐income parents or adults under demonstration waivers from the federal government. In the 34 states included in this study, Medicaid eligibility for mothers increased by 7 percentage points over the period of study, from 13 percent in 1996 to 20 percent in 2011 (Figure 1).2
Figure 1.
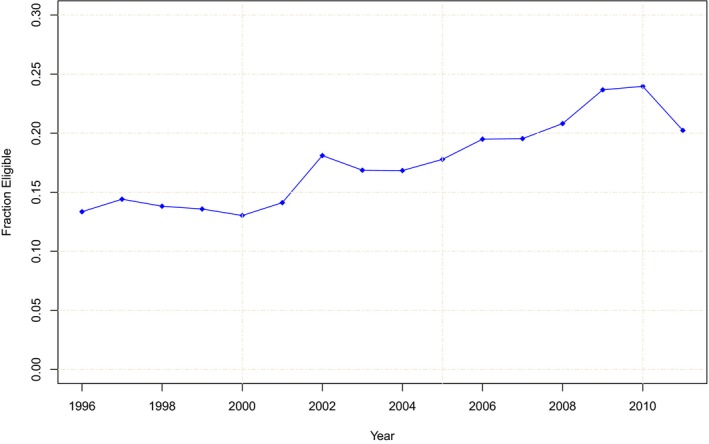
- Notes: Author's analysis of the 1997–2012 Annual Social and Economic Supplement of the Integrated Public Use Microdata Series, Current Population Survey (IPUMS‐CPS). The sample is restricted to nonelderly female parents aged 20–44 in families with at least one child under age 18. Parents are identified using family interrelationship variables in the IPUMS‐CPS, and these include biological, adoptive, and stepparent relationships.
In addition to evaluating how these expansions for parents changed insurance coverage before pregnancy, I examine whether there are changes in pregnancy intention status (as self‐reported by the mother) associated with the coverage expansions, as better access to preconception insurance coverage could increase contraception utilization and the planning of pregnancies. Finally, I also examine whether there were changes in insurance coverage during pregnancy and in the utilization of prenatal care. While state Medicaid rules for pregnant women are very generous and exceed eligibility thresholds for parents, women who receive Medicaid coverage prior to conception may be less likely to experience barriers to establishing care during pregnancy. Prior research has documented that among women receiving Medicaid during pregnancy, those with prepregnancy Medicaid coverage are more likely to initiate early prenatal care (Rosenberg et al. 2007). Alternatively, the parent expansions could reduce Medicaid coverage for prenatal care and delivery if improved access to family planning during the prepregnancy period reduces the number of Medicaid‐eligible pregnancies.
In each of these analyses, I also consider the role of state policies regarding public health insurance eligibility for pregnancy‐related care, as well as for family planning services. Medicaid eligibility for pregnant women has been documented to increase insurance coverage during pregnancy and improve the use of prenatal care (Currie and Gruber 1996b; Dubay et al. 2001; Howell 2001; Dave et al. 2008). In addition, optional state Medicaid programs that cover family planning services have been linked to increased receipt of reproductive health services, including contraception, and a reduction in birth rates (Lindrooth and McCullough 2007; Kearney and Levine 2009; Adams, Kenney, and Galactionova 2013; Wherry 2013; Adams, Galactionova, and Kenney 2015). For these reasons, concurrent state policies regarding coverage of pregnancy‐related care and family planning services are likely to also influence insurance coverage, prenatal care utilization, and pregnancy intention.
Relevant Literature
Relative to other types of eligibility expansions under the Medicaid program, such as expansions for pregnant women and children, expansions for parents have received considerably less attention. However, existing evaluations of pre‐ACA Medicaid eligibility expansions for parents find evidence of a significant increase in Medicaid coverage and little evidence of crowdout of private coverage for parents (Aizer and Grogger 2003; Busch and Duchovny 2005; Hamersma and Kim 2013; McMorrow et al. 2016), in addition to increased health care utilization (Busch and Duchovny 2005), better access to care (Busch and Duchovny 2005; McMorrow et al. 2016), and improved mental health (McMorrow et al. 2016). In addition, early evaluation of Medicaid expansions for parents under the ACA finds increased insurance coverage, improved affordability of care, and reductions in severe psychological distress (McMorrow et al. 2017).
While this is the first study to examine the role of parental Medicaid expansions on insurance coverage before and during pregnancy, it builds on an existing body of work that examines contractions or disruptions in Medicaid coverage among pregnant women following national welfare reform in 1996. Welfare reform delinked Medicaid and welfare eligibility and introduced other new restrictions on the welfare program. Researchers found that these changes led to a decrease in Medicaid coverage and increase in uninsurance prior to pregnancy (Adams et al. 2003, 2005; Handler et al. 2006; Gavin et al. 2007), a decrease in Medicaid coverage during and after pregnancy and increased uninsurance after pregnancy (Simon and Handler 2008), a small decline in first trimester prenatal care utilization (Kaestner and Lee 2005; Gavin et al. 2007), and fewer prenatal care visits (Kaestner and Lee 2005). Evidence from these studies suggests that expansions in Medicaid eligibility for parents might have the opposite effects.
Study Data and Methods
Data
To examine changes in insurance coverage before and during pregnancy and prenatal care utilization, I used data from the Pregnancy Risk Assessment Monitoring System (PRAMS). The PRAMS is the largest survey of women with a recent live birth in the United States and asks questions regarding the mother's experiences before, during, and shortly after pregnancy. With a few exceptions, data are collected by participating state health departments under a standardized data collection methodology prepared by the CDC. Women are sampled from each state's birth certificate file, and the data collected are state‐representative. Survey responses are linked to extracted birth certificate data items.
This analysis uses the PRAMS data for the years 1997 to 2012. The data available from states increased over the period with 13 states available in 1997 and 27 states available in 2012; survey participants in 2012 represented approximately 78 percent of all U.S. births (Centers for Disease Control and Prevention 2015). States rotate in and out from the survey from year to year due to a minimum overall response rate threshold policy. The analysis used information for all states available in each year; there were 34 states in the PRAMS for at least 1 year during the study period.3 Table 1 provides a detailed list of states in the PRAMS along with the years each state was included in the survey.
Table 1.
Pregnancy Risk Assessment Monitoring System (PRAMS) States and Medicaid Eligibility for Parents, Pregnant Women, and Family Planning Services
| Years in PRAMS | Regular Medicaid for Parents | Prenatal Medicaid | ||||||
|---|---|---|---|---|---|---|---|---|
| Simulated Eligibility for Female Parents Aged 20–44 | Simulated Eligibility for Women Aged 20–44 | Medicaid Family PlanningImplementation Date | ||||||
| 1996 | 2011 | Change | 1996 | 2011 | Change | |||
| Alabama | 1997–2003 | 0.08 | 0.09 | 0.01 | 0.31 | 0.39 | 0.08 | 2000 |
| Alaska | 1997–2010, 2012 | 0.17 | 0.23 | 0.06 | 0.39 | 0.56 | 0.17 | |
| Arkansas | 1997–2012 | 0.08 | 0.09 | 0.01 | 0.31 | 0.51 | 0.20 | 1997 |
| Colorado | 1998–2012 | 0.11 | 0.24 | 0.13 | 0.31 | 0.60 | 0.29 | |
| Delaware | 2007–2012 | 0.19 | 0.24 | 0.04 | 0.44 | 0.53 | 0.09 | |
| Florida | 1997–2005 | 0.09 | 0.10 | 0.01 | 0.44 | 0.51 | 0.07 | 1998 |
| Georgia | 1997, 2004–2012 | 0.09 | 0.11 | 0.02 | 0.44 | 0.53 | 0.09 | 2011 |
| Hawaii | 2000–2012 | 0.67 | 0.49 | −0.18 | 0.73 | 0.55 | −0.19 | |
| Illinois | 1997–2012 | 0.10 | 0.41 | 0.31 | 0.31 | 0.53 | 0.22 | 2007 |
| Louisiana | 1998–2004 | 0.08 | 0.09 | 0.01 | 0.31 | 0.53 | 0.22 | 2006 |
| Maine | 1997–2012 | 0.11 | 0.60 | 0.50 | 0.44 | 0.53 | 0.09 | |
| Maryland | 2001–2012 | 0.10 | 0.28 | 0.18 | 0.44 | 0.61 | 0.17 | 1995 |
| Massachusetts | 2007–2012 | 0.40 | 0.60 | 0.20 | 0.47 | 0.51 | 0.04 | |
| Michigan | 2001–2011 | 0.11 | 0.12 | 0.00 | 0.44 | 0.51 | 0.07 | 2006 |
| Minnesota | 2002–2012 | 0.55 | 0.56 | 0.02 | 0.62 | 0.65 | 0.03 | 2006 |
| Mississippi | 2003–2004, 2006, 2008–2009 | 0.07 | 0.11 | 0.03 | 0.44 | 0.51 | 0.07 | 2003 |
| Missouri | 2007 | 0.09 | 0.10 | 0.01 | 0.44 | 0.51 | 0.07 | 2009 |
| Nebraska | 2000–2012 | 0.10 | 0.13 | 0.03 | 0.35 | 0.51 | 0.16 | |
| New Jersey | 2002–2012 | 0.11 | 0.11 | 0.00 | 0.67 | 0.68 | 0.01 | |
| New Mexico | 1997–2005, 2011–2012 | 0.10 | 0.11 | 0.01 | 0.44 | 0.58 | 0.14 | 1998 |
| New York | 1997–2008, 2010–2011 | 0.14 | 0.35 | 0.21 | 0.44 | 0.53 | 0.09 | 2002 |
| North Carolina | 1997–2005, 2008 | 0.09 | 0.12 | 0.03 | 0.44 | 0.51 | 0.07 | 2005 |
| Ohio | 1999–2003, 2005–2010, 2012 | 0.10 | 0.22 | 0.12 | 0.31 | 0.51 | 0.20 | |
| Oklahoma | 1997–2012 | 0.09 | 0.44 | 0.34 | 0.35 | 0.52 | 0.17 | 2005 |
| Oregon | 2003–2012 | 0.19 | 0.44 | 0.25 | 0.31 | 0.49 | 0.18 | 1999 |
| Pennsylvania | 2007–2012 | 0.11 | 0.11 | 0.00 | 0.44 | 0.51 | 0.07 | 2007 |
| Rhode Island | 2002–2012 | 0.12 | 0.40 | 0.27 | 0.74 | 0.60 | −0.14 | 1994 |
| South Carolina | 1997–2007 | 0.08 | 0.13 | 0.06 | 0.44 | 0.51 | 0.07 | 1997 |
| Tennessee | 2008–2009, 2012 | 0.08 | 0.17 | 0.09 | 0.44 | 0.60 | 0.16 | |
| Utah | 1999–2012 | 0.11 | 0.12 | 0.01 | 0.31 | 0.39 | 0.08 | |
| Washington | 1997–2012 | 0.40 | 0.12 | −0.28 | 0.44 | 0.51 | 0.07 | 2001 |
| West Virginia | 1997–2011 | 0.08 | 0.10 | 0.01 | 0.35 | 0.43 | 0.08 | |
| Wisconsin | 2007–2009, 2011–2012 | 0.12 | 0.44 | 0.32 | 0.44 | 0.67 | 0.24 | 2003 |
| Wyoming | 2007–2012 | 0.10 | 0.12 | 0.02 | 0.31 | 0.43 | 0.11 | 2008 |
Source information is given in Section B and Tables A1 and A2 in Appendix SA1.
I restricted the sample to women aged 20 and older who were already parents (i.e., they had a previous live birth), and who had valid information on race, ethnicity, age, marital status, and educational attainment.4 Approximately 6.8 percent of respondents were excluded from the sample because of missing information on these characteristics. The sample was restricted to women who were already parents as this population was the target of Medicaid parental eligibility expansions. I used information on previous live births from the birth certificate record to identify women who were already mothers prior to pregnancy as other information regarding children was not available in the data.
The outcomes of interest were measures of health insurance coverage before and during pregnancy, pregnancy intention, and measures describing prenatal care utilization. Using questions asked in the core survey of the PRAMS, I examined overall health insurance coverage and Medicaid coverage before pregnancy, coverage for prenatal care during pregnancy, and coverage for delivery. I also considered whether the pregnancy was unintended, following the standard definition as either the pregnancy was unwanted or occurred too soon (Mosher, Jones, and Abma 2012). There were slight changes in the design of the survey questions collecting information on health insurance coverage and pregnancy intention status over the study period. Details on these changes and the coding of the outcome variables are provided in Section 1 in Appendix SA1.
Using information on the birth certificate record, I next examined the use of any prenatal care during pregnancy and whether prenatal care was initiated during the first trimester of pregnancy. I also constructed a measure indicating whether prenatal care was initiated as early as the mother wanted based on her response to the PRAMS survey; this measure was not available for the 2012 survey year. Finally, I examined whether prenatal care utilization was adequate as determined by the Kessner and Kotelchuck indices, respectively. Both indices combine information on the timing of prenatal care and number of prenatal care visits, while adjusting for gestation length, and are associated with better infant health at birth (VanderWeele et al. 2009).
Changes in Medicaid Eligibility
I constructed a measure of the generosity of Medicaid eligibility for female parents in each state and year following the existing literature (Currie and Gruber 1996a,b; Cutler and Gruber 1996). Using a national sample of 3,000 female parents of ages 20–44 from each 1997–2012 Annual Social and Economic Supplement (ASEC) of the Integrated Public Use Microdata Series of the Current Population Survey (IPUMS‐CPS; King et al. 2010), I estimated the fraction of this national sample that would be eligible for Medicaid in each state for a given year using state eligibility rules. This measure of “simulated eligibility” isolated changes in eligibility for parents that result from changes in state Medicaid policy, rather than changes in a state's socioeconomic characteristics. Additional details on the construction of this measure are in Section 2 in Appendix SA1.
Table 1 displays this measure of simulated eligibility for female parents in 1996 and 2011 for each state in the PRAMS. The table also reports the change in simulated eligibility over the study period for each state. For almost all states, the change is positive indicating an increase in eligibility, although the magnitude of the eligibility change varies. About half of the states (18) saw no or little change (<5 percentage points) in parental eligibility over the period. Eight states saw changes of 20 percentage points or greater. The average change in state eligibility was a 9‐percentage point increase.
Table 1 also provides information on other state Medicaid policies that are considered in the analysis. The next set of columns provides similarly constructed measures of the generosity of state prenatal coverage for women aged 20–44 in the event of a pregnancy for each state in 1996 and 2011, as well as the eligibility change over the period. While many prenatal expansions under Medicaid occurred prior to 1996, states did see changes in eligibility over the study period with an average eligibility gain of 10 percentage points.
The final column displays information on whether states had Medicaid family planning waivers and their date of implementation. Twenty‐two states had active Medicaid family planning programs at some point during the study period.
Statistical Analysis
To estimate the effect of state expansions in parental coverage during the study period, I estimated a regression model for each outcome where the main predictor was the simulated eligibility measure for female parents aged 20–44 in each year. I also controlled for changes in state Medicaid prenatal eligibility for women of these ages using a simulated eligibility measure, as well as for the presence of a state Medicaid family planning waiver program with an indicator variable. All regressions included state and year fixed effects to control for time‐invariant differences in outcomes across states and secular trends that were unrelated to state Medicaid policy changes. Regressions also included individual control variables (indicators for black and other race, Hispanic ethnicity, age group dummies (ages 25–29, 30–34, 35–39, and 40 and older), marital status, and years of schooling (12 years, 13–15 years, 16+ years), as well as time‐varying state characteristics and policy variables that were merged on using the year prior to childbirth to account for the 9‐month pregnancy period. These variables included state‐level measures of sociodemographic characteristics (age, sex, and race/ethnicity profiles and educational attainment), economic conditions (unemployment rate and median household income), and policies that might have influenced fertility decisions during this period (indicators for welfare reform and family cap policies and the maximum welfare benefit for a family of three; indicators for state mandates for private health insurance coverage of contraceptives, and availability of over‐the‐counter emergency contraception; indicators for state abortion restrictions on Medicaid funding and mandatory delay in abortion laws). Complete source information for these variables is available in Table A2 in Appendix SA1.
In addition to evaluating changes in outcomes for all pregnant mothers, I also examined whether there were differential effects of the expansions by maternal education. Under these regression models, I estimated separate effects for mothers with <12 years of education and those with 12 or more years of education by interacting dummy variables identifying these two groups with the measure of state Medicaid generosity for parents. This allowed for a different estimated impact of the policy change among women with less education, who were expected to have lower levels of income and fewer alternative options for health insurance coverage. Although both groups of mothers saw similarly sized changes in eligibility over the period, 41.6 percent of mothers with <12 years of education were eligible for parental Medicaid, compared to just 14.4 percent of higher education mothers.
All regressions used PRAMS analytic weights to account for sampling, nonresponse, and noncoverage in the survey. Heteroskedasticity‐robust standard errors were clustered by state to account for within‐state correlation of the error terms and the state‐level nature of the Medicaid expansions (Bertrand, Duflo, and Mullainathan 2004).
Limitations
There are limitations to this analysis. First, although the quasi‐experimental study design accounts for many potential state‐level differences in Medicaid and other policies, it is possible that unobserved time‐varying factors (such as hard to measure changes in attitudes toward pregnancy) could influence study outcomes, leading to biased estimates.
As a placebo test, I examined whether there was an association between changes in parental Medicaid eligibility and outcomes for pregnant women without prior births. For these women, we would only expect to see associated changes in outcomes if Medicaid parental eligibility policies were correlated with omitted variables related to insurance coverage and prenatal utilization. I found no significant evidence of changes in outcomes associated with parental Medicaid eligibility for this population.
A second limitation is that the PRAMS does not include all states. Therefore, the estimates presented here only represent the experiences of women residing in the available states. In addition, as the states included in the survey change over the length of study, a potential concern is that state data availability in the PRAMS might be somehow correlated with the parental expansions in Medicaid eligibility and bias the results. To investigate this further, I directly tested whether state data availability was correlated with state parental Medicaid eligibility. As discussed later, I found no evidence of a significant association.
Study Results
Sample Characteristics
Table 2 presents summary means for all mothers experiencing live births, overall and by mother's educational status. Mothers with <12 years of education were younger, more likely to be a minority or Hispanic, and less likely to be married. More than half (52.6 percent) of mothers with <12 years of education reported having no health insurance before pregnancy, compared with 19 percent of mothers with more education. Uninsurance for prenatal care and for delivery was less common for both groups (as Medicaid is available to more women once they become pregnant), although 15 percent of mothers with low education status reported no source of insurance for prenatal care and 8 percent reported no insurance for delivery. Mothers with low education status were more likely to report that their pregnancy was unintended and less likely to start prenatal care in the first trimester or as early as they wanted. They were also less likely to have adequate prenatal care utilization as measured by both the Kessner and Kotelchuck indices.
Table 2.
Sociodemographic Characteristics, Health Insurance Coverage, Pregnancy Intention, and Prenatal Care Utilization among Mothers by Educational Attainment
| %, Unless Otherwise Indicated | All Mothers | Mothers with <12 years of Education | Mothers with 12+ years of Education |
|---|---|---|---|
| Sociodemographic Characteristics | |||
| Age | |||
| 20–24 | 21.2 | 39.6 | 17.5 |
| 25–29 | 30.5 | 31.7 | 30.3 |
| 30–34 | 29.6 | 18.1 | 32.0 |
| 35–39 | 15.4 | 8.6 | 16.7 |
| 40+ | 3.3 | 2.0 | 3.6 |
| Race/ethnicity | |||
| White | 75.4 | 69.5 | 76.6 |
| Black | 15.6 | 17.2 | 15.3 |
| Other race | 9.0 | 13.3 | 8.1 |
| Hispanic | 15.3 | 42.9 | 9.7 |
| Education | |||
| <12 years of education | 16.8 | 100.0 | 0.0 |
| 12 years of education | 30.2 | 0.0 | 36.2 |
| 13–15 years of education | 25.0 | 0.0 | 30.1 |
| >=16 years of education | 28.0 | 0.0 | 33.7 |
| Married | 70.9 | 46.4 | 75.8 |
| Health Insurance Coverage | |||
| Health insurance before pregnancy | |||
| No insurance | 25.1 | 52.6 | 19.2 |
| Medicaid | 16.6 | 29.8 | 13.8 |
| Health insurance for prenatal care | |||
| No insurance | 6.5 | 14.7 | 4.8 |
| Medicaid | 34.5 | 65.6 | 28.0 |
| Health insurance for delivery | |||
| No insurance | 4.6 | 8.3 | 3.9 |
| Medicaid | 38.1 | 74.3 | 30.4 |
| Pregnancy Intention | |||
| Unintended birth | 40.8 | 52.8 | 38.4 |
| Prenatal Care Utilization | |||
| Any prenatal care utilization | 99.0 | 97.7 | 99.3 |
| Timing of prenatal care utilization | |||
| Started prenatal care as early as wanted | 84.6 | 78.0 | 85.9 |
| Started prenatal care in first trimester | 82.8 | 67.8 | 85.9 |
| Adequacy of prenatal care utilization | |||
| Adequate on Kessner Index | 73.7 | 56.4 | 77.3 |
| Adequate or Adequate Plus on Kotelchuck Index | 75.2 | 62.0 | 77.8 |
| N | 292,110 | 49,000 | 243,110 |
Author's analysis of the 1997–2012 Pregnancy Risk Assessment Monitoring System. All means estimated using survey weights. The estimation sample was defined as women aged 20 years and older with a previous live birth.
Regression Estimates
Table 3 presents estimates of the effect of expanding parental Medicaid eligibility on the health insurance coverage, pregnancy intention, and prenatal care utilization of pregnant mothers. The estimates suggest that a 10‐percentage point increase in parental Medicaid eligibility was associated with a 1.1‐percentage point increase in prepregnancy Medicaid coverage and a 0.8‐percentage point reduction in uninsurance. This represents approximately a 3.2 percent decrease in uninsurance when compared to the sample mean. In addition, the estimates indicate similarly sized changes in reported health insurance for prenatal care. A 10‐percentage point increase in parental Medicaid eligibility was associated with approximately a 1‐percentage point increase in Medicaid coverage and a 0.7‐percentage point reduction in uninsurance for prenatal care, which represents a 10.8 percent decrease over the sample mean. There was no significant change in health insurance coverage for delivery associated with expanded parental eligibility.
Table 3.
Estimated Effect of State Generosity of Medicaid for Parents
| Health Insurance before Pregnancy | Health Insurance during Pregnancy | Pregnancy Intention | Prenatal Care Utilization | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No Insurance | Medicaid | Prenatal Care | Delivery Care | Unintended Birth | Any Prenatal Care | Initiation | Adequacy | |||||
| No Insurance | Medicaid | No Insurance | Medicaid | As Early as Wanted | First Trimester | Kessner Index | Kotelchuck Index | |||||
| Parent Medicaid eligibility | −0.084*** | 0.112*** | −0.073*** | 0.095*** | −0.025 | 0.032 | −0.028 | −0.005 | 0.049** | 0.013 | 0.085 | 0.084 |
| (0.028) | (0.031) | (0.022) | (0.030) | (0.023) | (0.032) | (0.023) | (0.008) | (0.024) | (0.017) | (0.061) | (0.072) | |
| Other eligibility pathways | ||||||||||||
| Prenatal eligibility | 0.020 | −0.040 | −0.037 | 0.167** | −0.074 | 0.202*** | −0.033 | −0.001 | −0.073** | 0.040 | 0.030 | −0.069 |
| (0.047) | (0.085) | (0.071) | (0.079) | (0.069) | (0.063) | (0.038) | (0.016) | (0.030) | (0.055) | (0.130) | (0.119) | |
| Family planning waiver | 0.014** | −0.013* | −0.005 | 0.002 | −0.001 | −0.001 | −0.011** | −0.002 | −0.002 | 0.008 | 0.011 | 0.001 |
| (0.006) | (0.007) | (0.005) | (0.007) | (0.005) | (0.007) | (0.004) | (0.002) | (0.003) | (0.006) | (0.011) | (0.010) | |
| Sample mean | 0.251 | 0.161 | 0.065 | 0.345 | 0.046 | 0.381 | 0.408 | 0.990 | 0.846 | 0.828 | 0.737 | 0.752 |
| N | 291,352 | 291,242 | 288,420 | 288,239 | 288,449 | 288,309 | 279,055 | 279,055 | 280,448 | 279,055 | 277,747 | 282,764 |
Author's analysis of the 1997–2012 Pregnancy Risk Assessment Monitoring System. This table reports the estimated coefficient for the simulated eligibility measure in a regression that also includes state and year fixed effects, individual control variables (indicators for black and other races, Hispanic ethnicity, age group dummies, indicator for currently being married, and indicators for different amounts of schooling), and state–year measures of sociodemographic characteristics, economic conditions, and policies that may have influenced fertility decisions during this period. See text for additional details on these variables. Estimation sample is defined as women aged 20 years and older with a previous live birth. All regressions use PRAMS analytic weights, and heteroskedasticity‐robust standard errors are clustered by state. The symbols ***, **, and * indicate statistical significance at the 1, 5, and 10 percent levels, respectively.
Prenatal eligibility was not significantly associated with health insurance coverage before pregnancy. However, changes in prenatal eligibility were associated with significant increases in Medicaid coverage for prenatal care and for delivery. The coefficient estimates for uninsurance were smaller in magnitude and not statistically significant, suggesting that expanded Medicaid coverage during pregnancy may crowd out other sources of insurance. In contrast, state Medicaid family planning programs appear to have no impact on insurance coverage during pregnancy. The presence of a family planning program, however, did increase the likelihood that a mother was without prepregnancy insurance coverage.
Next, I examined pregnancy intention and prenatal care utilization. There was no significant change in the report of an unintended pregnancy or on measures of prenatal care utilization as measured from the birth certificate records associated with the parental Medicaid expansions. However, mothers were more likely to report that they started prenatal care as early as they wanted to with a 10‐percentage point increase in Medicaid eligibility associated with a 0.5‐percentage point increase on this measure. I found evidence of a different relationship with Medicaid prenatal eligibility, with mothers less likely to report starting prenatal care as early as they wanted. Finally, state Medicaid family planning programs had no impact on prenatal care utilization but did decrease the incidence of unintended births.
In Table 4, I estimate the effect of state Medicaid generosity for parents separately for mothers with <12 years of education and mothers with 12 or more years of education. The estimated effect of expanded parental eligibility on prepregnancy insurance coverage was larger for mothers with <12 years of education. A 10‐percentage point increase in Medicaid eligibility was associated with a 2.1‐percentage point decrease in uninsurance for mothers with low education status, compared to a 0.6‐percentage point (and not statistically significant) decrease for mothers with high education status. The estimated coefficient for health insurance for prenatal care associated with parental Medicaid eligibility, although not statistically significant, was also larger for mothers with low education status compared to mothers with 12 years or more of education.
Table 4.
Estimated Effect of State Generosity of Medicaid for Parents by Mother's Education Status
| Health Insurance before Pregnancy | Health Insurance during Pregnancy | Pregnancy Intention | Prenatal Care Utilization | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No Insurance | Medicaid | Prenatal Care | Delivery Care | Unintended Birth | Any Prenatal Care | Initiation | Adequacy | |||||
| No Insurance | Medicaid | No Insurance | Medicaid | As Early as Wanted | First Trimester | Kessner Index | Kotelchuck Index | |||||
| Parent Medicaid eligibility | ||||||||||||
| Mothers with <12 years of education | −0.208*** | 0.181*** | −0.141 | 0.172 | 0.038 | −0.002 | −0.061* | 0.019* | 0.133*** | 0.084* | 0.183** | 0.178** |
| (0.069) | (0.066) | (0.092) | (0.106) | (0.086) | (0.085) | (0.036) | (0.010) | (0.022) | (0.042) | (0.070) | (0.074) | |
| Sample mean | 0.526 | 0.298 | 0.147 | 0.656 | 0.083 | 0.743 | 0.528 | 0.977 | 0.780 | 0.676 | 0.564 | 0.620 |
| Mothers with >=12 years of education | −0.060* | 0.099*** | −0.061** | 0.080** | −0.037* | 0.039 | −0.022 | −0.009 | 0.033 | −0.000 | 0.067 | 0.066 |
| (0.032) | (0.032) | (0.022) | (0.030) | (0.021) | (0.032) | (0.024) | (0.008) | (0.026) | (0.020) | (0.062) | (0.073) | |
| Sample mean | 0.192 | 0.138 | 0.048 | 0.28 | 0.039 | 0.304 | 0.384 | 0.993 | 0.859 | 0.859 | 0.773 | 0.778 |
| N | 291,352 | 291,242 | 288,420 | 288,239 | 288,449 | 288,309 | 279,055 | 279,055 | 280,448 | 279,055 | 277,747 | 282,764 |
Author's analysis of the 1997–2012 Pregnancy Risk Assessment Monitoring System. This table reports the estimated coefficient for the simulated eligibility measure interacted with indicators for mother's education level in a regression that also includes state and year fixed effects, individual control variables (indicators for black and other races, Hispanic ethnicity, age group dummies, indicator for currently being married, and indicators for different amounts of schooling), and state–year measures of sociodemographic characteristics, economic conditions, and policies that may have influenced fertility decisions during this period. See text for additional details on these variables. Estimation sample is defined as women aged 20 years and older with a previous live birth. All regressions use PRAMS analytic weights and heteroskedasticity‐robust standard errors are clustered by state. The symbols ***, **, and * indicate statistical significance at the 1, 5, and 10 percent levels, respectively.
While there was no significant change in reported pregnancy intention or the use of any prenatal care, there were significant changes in the timing and adequacy of prenatal care utilization for low‐education mothers associated with expanded parental eligibility. A 10‐percentage point increase in eligibility was associated with a 1.3‐percentage point increase in low‐education mothers starting prenatal care as early as they wanted, a 1.8‐percentage point increase in the adequacy of prenatal care utilization as measured on the Kessner index, and a 1.8‐percentage point increase in prenatal care adequacy as measured on the Kotelchuck index.
Placebo and Sensitivity Tests
To further test these results, I ran several additional placebo and sensitivity checks. First, I conducted a placebo test that examined whether there was an association between changes in parental Medicaid eligibility and outcomes for pregnant women without prior births, or those women that we would not expect to be affected by changes in Medicaid rules for parents. The results are reported in Table A3 in Appendix SA1. I found no evidence of significant changes in any of the outcome measures for this sample.
I also further examined the changing data availability for states in the PRAMS in each year. For all states in the United States, I tested whether data availability for a given year was associated with parental Medicaid eligibility. I found no evidence of a significant relationship (see Table A4 in Appendix SA1). Next, I tested the robustness of the findings to an alternative method of conducting inference, given the small number of states available in the PRAMS and their uneven participation in the survey over time. I calculated the p‐value using a wild cluster bootstrap‐t procedure, which has been shown to perform well under these circumstances (Cameron and Miller 2015). The results are reported in Table A5 in Appendix SA1. All estimates for changes in health insurance before pregnancy and changes in prenatal care utilization for the full sample of mothers and for those with lower education status remained significant at the 5 percent level.
Discussion
Changes in state Medicaid eligibility rules for parents following welfare reform increased access to health insurance coverage prior to pregnancy among women who were already mothers. Using PRAMS data, I found an increase in Medicaid coverage prior to pregnancy and a decrease in uninsurance among pregnant mothers in states expanding eligibility for parents during the 1996–2011 period. Not only did expanded Medicaid eligibility improve insurance coverage prior to pregnancy, but there was also a significant increase in reported Medicaid coverage and a decrease in uninsurance for prenatal care during pregnancy. Given the existing generosity of Medicaid prenatal coverage for women required of all states, one potential explanation for this finding is that women who receive Medicaid coverage prior to conception might be more likely to use Medicaid coverage for prenatal care. There was no change observed in Medicaid or insurance coverage for deliveries, which is perhaps unsurprising given that labor and delivery services were already covered by Medicaid and the financial incentives for hospitals to seek reimbursement for these services.
Although an important component of preconception care for women is family planning services (Lu 2007), I did not detect a significant change in reports of unintended births associated with expanded Medicaid parental eligibility. This does not, however, rule out changes in unintended pregnancies that did not result in live births. Given that the PRAMS samples from birth certificate records, it is not possible to examine changes in birth rates or the termination of pregnancies associated with expanded Medicaid parental eligibility using this data source.
Finally, I found a significant increase in pregnant mothers reporting that they were able to start prenatal care as early as they wanted. This is likely related to the increase in Medicaid coverage for prenatal care that was also observed, as Medicaid ensures payment for prenatal care once a woman enters care. In addition, the majority of states have presumptive eligibility or other expedited enrollment processes for pregnant women to encourage timely prenatal care (Broaddus 2008). When examining the effect of Medicaid parental expansions separately for mothers with <12 years of education, I found further evidence of improvements in prenatal care utilization for this vulnerable subgroup. There were increases in the adequacy of prenatal care utilization as measured on both the Kessner and Kotelchuck indices associated with expanded Medicaid parental eligibility for these mothers. Adequacy of prenatal care utilization measured using both of these indices has been linked to better birth outcomes as measured by the occurrence of small‐for‐gestational‐age, preterm birth, and infant mortality (VanderWeele et al. 2009).
Conclusion
This study documents that prior to the ACA, optional state expansions in Medicaid coverage for parents significantly increased the prepregnancy health insurance coverage of pregnant mothers. In addition, expanded insurance coverage prior to pregnancy led to earlier initiation and improved adequacy of prenatal care among pregnant mothers. These findings suggest that expanding health insurance coverage for low‐income women may have important consequences not only for the health of the mother but also for her children by increasing access to needed medical care. Furthermore, access to health coverage during periods of nonpregnancy, including family planning services, may further impact pregnancy outcomes if women are more likely to plan pregnancies during periods of optimal health or spacing between births, as well as improve their health behaviors prior to conception.
More recent state expansions in Medicaid under the ACA have the potential to impact even more women and children as they extend eligibility to all low‐income women regardless of parental or pregnancy status. As the data become available, evaluating the role of these new expansions in Medicaid on preconception health and health care, and whether they lead to reduced disparities in maternal and infant health, will be critical. If expanding insurance coverage for low‐income adults and parents leads to better outcomes for the next generation, this will be an important benefit to document and to be considered by states deciding whether to expand or if faced with new decisions regarding their Medicaid programs, as well as by policy makers aiming to improve population health.
Supporting information
Appendix SA1. Supplemental Appendix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: I would like to acknowledge the PRAMS Working Group and the Centers for Disease Control and Prevention for assistance in accessing and interpreting the PRAMS data. In addition, I am grateful to Michel Boudreaux and Brendan Saloner for helpful comments on earlier versions of this manuscript. Finally, I would like to acknowledge nonfinancial support received from facilities and resources provided by the California Center for Population Research at UCLA (CCPR), which receives core support (R24‐HD041022) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
Disclosures: None.
Disclaimer: None.
Notes
In 2012, 67 percent of women with <12 years of education giving birth had previously had at least one live birth. Author's calculation from the 2012 Vital Statistics Birth Data files available for download from the National Center for Health Statistics at http://www.cdc.gov/nchs/data_access/vitalstatsonline.htm.
Author's calculation of actual eligibility changes; see Figure 1 note for details.
While Vermont was available in the PRAMS, observations from this state were dropped from the analysis due to missing information on mother's race.
Information on mother's age is limited to the following age groups: <17, 18–19, 20–24, 25–29, 30–34, 35–39, and 40+. I focus on women aged 20 and older as those aged 18 may still qualify for public health insurance under child coverage provisions. Only 0.1 percent of women were missing age information and were excluded from the sample. In addition, <0.6 percent of PRAMS respondents were missing information on the number of previous live births and were excluded.
References
- Adams, E. K. , Galactionova K., and Kenney G. M.. 2015. “Medicaid Family Planning Waivers in Three States: Did They Reduce Unwanted Births?” Inquiry 52: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams, E. K. , Kenney G. M., and Galactionova K.. 2013. “Preventive and Reproductive Health Services for Women: The Role of California's Family Planning Waiver.” American Journal of Health Promotion 27 (3 Supplement): eS1–10. [DOI] [PubMed] [Google Scholar]
- Adams, E. K. , Gavin N. I., Handler A., Manning W., and Raskind‐Hood C.. 2003. “Transitions in Insurance Coverage from before Pregnancy through Delivery In Nine States, 1996–1999.” Health Affairs 22 (1): 219–29. [DOI] [PubMed] [Google Scholar]
- Adams, E. K. , Gavin N. I., Manning W. G., and Handler A.. 2005. “Welfare Reform, Insurance Coverage Pre‐Pregnancy, and Timely Enrollment: An Eight‐State Study.” Inquiry 42: 129–44. [DOI] [PubMed] [Google Scholar]
- Aizer, A. , and Currie J.. 2014. “The Intergenerational Transmission of Inequality: Maternal Disadvantage and Health at Birth.” Science 344 (6186): 856–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aizer, A. , and Grogger J.. 2003. Parental Medicaid Expansions and Health Insurance Coverage. National Bureau of Economic Research Working Paper No. 9907.
- Bertrand, M. , Duflo E., and Mullainathan S.. 2004. “How Much Should We Trust Differences‐in‐Differences Estimates?” Quarterly Journal of Economics 119 (1): 249–75. [Google Scholar]
- Broaddus, E. T. 2008. Presumptive Eligibility for Pregnant Women. State Health Policy Monitor. Washington, DC: National Academy for State Health Policy. [Google Scholar]
- Busch, S. H. , and Duchovny N.. 2005. “Family Coverage Expansions: Impact on Insurance Coverage and Health Care Utilization of Parents.” Journal of Health Economics 24: 876–90. [DOI] [PubMed] [Google Scholar]
- Cameron, A. C. , and Miller D. L.. 2015. “A Practitioner's Guide to Cluster‐Robust Inference.” Journal of Human Resources 50 (2): 317–72. [Google Scholar]
- Centers for Disease Control and Prevention . 2000. “Entry into Prenatal Care, United States, 1989–1997.” Morbidity and Mortality Weekly Report 49 (18): 393–8. [Google Scholar]
- Centers for Disease Control and Prevention . 2015. “PRAMS: Using Surveillance to Improve the Health of Mothers and Babies” National Center for Chronic Disease Prevention and Health Promotion, Division of Reproductive Health [accessed on March 31, 2016]. Available at http://www.cdc.gov/prams/pdf/about/what-is-prams-2015_tag508.pdf
- Chen, A. , Oster E., and Williams H.. 2016. “Why Is Infant Mortality Higher in the United States Than in Europe?” American Economic Journal: Economic Policy 8: 89–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie, J. , and Gruber J.. 1996a. “Health Insurance Eligibility, Utilization of Medical Care, and Child Health.” The Quarterly Journal of Economics 111 (2): 431–66. [Google Scholar]
- Gruber J.. 1996b. “Saving Babies: The Efficacy and Cost of Recent Changes in the Medicaid Eligibility of Pregnant Women.” Journal of Political Economy 104 (6): 1263–96. [Google Scholar]
- Cutler, D. M. , and Gruber J.. 1996. “The Effect of Medicaid Expansions on Public Insurance, Private Insurance, and Redistribution.” The American Economic Review 86 (2): 378–83. [PubMed] [Google Scholar]
- Dave, D. M. , Decker S., Kaestner R., and Simon K. I.. 2008. Re‐Examining the Effects of the Medicaid Expansions for Pregnant Women. NBER Working Paper No. 14591.
- Dubay, L. , Joyce T., Kaestner R., and Kenney G. M.. 2001. “Changes in Prenatal Care Timing and Low Birth Weight by Race and Socioeconomic Status: Implications for the Medicaid Expansions for Pregnant Women.” Health Services Research 36 (2): 373–98. [PMC free article] [PubMed] [Google Scholar]
- Floyd, R. L. , Johnson K. A., Owens J. R., Verbiest S., Moore C. A., and Boyle C.. 2013. “A National Action Plan for Promoting Preconception Health and Health Care in the United States (2012–2014).” Journal of Women's Health 22 (1): 797–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavin, N. I. , Adams E. K., Manning W. G., Raskind‐Hood C., and Urato M.. 2007. “The Impact of Welfare Reform on Insurance Coverage before Pregnancy and the Timing of Prenatal Care Initiation.” Health Services Research 42 (4): 1564–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamersma, S. , and Kim M.. 2013. “Participation and Crowd Out: Assessing the Effects of Parental Medicaid Expansions.” Journal of Health Economics 32: 160–71. [DOI] [PubMed] [Google Scholar]
- Handler, A. , Rosenberg D. M., Rankin K. M., Zimbeck M., and Adams E. K.. 2006. “The Pre‐Pregnancy Insurance Status of Public Aid Recipients in the Aftermath of Welfare Reform: Women in the Medicaid Gap.” Journal of Health Care for the Poor and Underserved 17 (1): 162–79. [DOI] [PubMed] [Google Scholar]
- Howell, E. M. 2001. “The Impact of the Medicaid Expansions for Pregnant Women: A Synthesis of the Evidence.” Medical Care Research and Review 58 (1): 3–30. [DOI] [PubMed] [Google Scholar]
- Johnson, K. , Posner S. F., Biermann J., Cordero J. F., Atrash H. K., Parker C. S., Boulet S., and Curtis M. G.. 2006. “Recommendations to Improve Preconception Health and Health Care: A Report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care.” Morbidity and Mortality Weekly Report 55: 1–23. [PubMed] [Google Scholar]
- Kaestner, R. , and Lee W. C.. 2005. “The Effect of Welfare Reform on Prenatal Care and Birth Weight.” Health Economics 14: 497–511. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation . 2002. The Kaiser Commission on Medicaid and the Uninsured. Medicaid Resources Book. Washington, DC: The Henry J Kaiser Family Foundation. [Google Scholar]
- Kaiser Family Foundation . 2016. “Status of State Action on the Medicaid Expansion Decision” [accessed on October 17, 2016]. Available at http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-theaffordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
- Kearney, M. S. , and Levine P. B.. 2009. “Subsidized Contraception, Fertility, and Sexual Behavior.” Review of Economics and Statistics 91 (1): 137–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, M. , Ruggles S., Alexander J. T., Flood S., Genadek K., Schroeder M. B., Trampe B., and Vick R.. 2010. Integrated Public Use Microdata Series, Current Population Survey: Version 3.0. [Machine‐Readable Database]. Minneapolis: University of Minnesota. [Google Scholar]
- Lindrooth, R. C. , and McCullough J. S.. 2007. “The Effect of Medicaid Family Planning Expansions on Unplanned Births.” Women's Health Issues 17: 66–74. [DOI] [PubMed] [Google Scholar]
- Lu, M. C. 2007. “Recommendations for Preconception Care.” American Family Physician 76 (3): 397–400. [PubMed] [Google Scholar]
- Lu, M. C. , and Johnson K. A.. 2014. “Toward a National Strategy on Infant Mortality.” American Journal of Public Health 104 (S1): S13–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDorman, M. F. , Matthews T. J., Mohangoo A. D., and Zeitlin J.. 2014. “International Comparisons of Infant Mortality and Related Factors: United States and Europe, 2010.” National Vital Statistics Reports 63: 1–6. [PubMed] [Google Scholar]
- McDonald, T. P. , and Coburn A. F.. 1988. “Predictors of Prenatal Care Utilization.” Social Science & Medicine 27 (2): 167–72. [DOI] [PubMed] [Google Scholar]
- McMorrow, S. , Kenney G. M., Long S. K., and Goin D. E.. 2016. “Medicaid Expansions from 1997 to 2009 Increased Coverage and Improved Access and Mental Health Outcomes for Low‐Income Parents.” Health Services Research 51 (4): 1347–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMorrow, S. , Gates J. A., Long S. K., and Kenney G. M.. 2017. “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low‐Income Parents.” Health Affairs 36 (5): 808–18. [DOI] [PubMed] [Google Scholar]
- Mosher, W. D. , Jones J., and Abma J. C.. 2012. Intended and Unintended Births in the United States: 1982–2010. National Health Statistics Reports, Number 55. U.S. Department of Health and Human Services. [PubMed]
- Norwood, T. 2014. “Pregnancy Intention. Pennsylvania Department of Health, Bureau of Family Health, Division of Child and Adult Health Services” [accessed on October 16, 2016]. Available at http://www.health.pa.gov/MyRecords/Health-Research/Documents/Pregnancy_Intention_Report_11_19_2014.pdf
- Rosenberg, D. , Handler A., Rankin K. M., Zimbeck M., and Adams E. K.. 2007. “Prenatal Care Initiation among Very low‐Income Women in the Aftermath of Welfare Reform: Does Pre‐Pregnancy Medicaid Coverage Make a Difference?” Maternal and Child Health Journal 11 (1): 11–7. [DOI] [PubMed] [Google Scholar]
- Salganicoff, A. , Ranji U., and Wyn R.. 2005. Women and Health Care: A National Profile. Menlo Park, CA: The Henry J Kaiser Family Foundation:1–62. [Google Scholar]
- Salganicoff, A. , and Wyn R.. 1999. “Access to Care for Low‐Income Women: The Impact of Medicaid.” Journal of Health Care for the Poor and Underserved 10 (4): 453–67. [DOI] [PubMed] [Google Scholar]
- Simon, K. I. , and Handler A.. 2008. “Welfare Reform and Insurance Coverage during the Pregnancy Period: Implications for Preconception and Interconception Care.” Women's Health Issues 18s: S97–106. [DOI] [PubMed] [Google Scholar]
- VanderWeele, T. J. , Lantos J. D., Siddique J., and Lauderdale D. S.. 2009. “A Comparison of Four Prenatal Care Indices in Birth Outcome Models: Comparable Results for Predicting Small‐for‐Gestational‐Age Outcome but Different Results for Preterm Birth or Infant Mortality.” Journal of Clinical Epidemiology 62: 438–45. [DOI] [PubMed] [Google Scholar]
- Wherry, L. R. 2013. “Medicaid Family Planning and Related Preventive Care.” American Journal of Public Health 103 (9): 1577–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1. Supplemental Appendix.


