Abstract
Background and objectives
Overweight and obesity are among the important challenges in health issues and survival of elderly people. The current study aimed to evaluate the survival rate of elderly patients with diabetes, and its influencing factors, on the basis of body mass index (BMI).
Methods and materials
The design of the current study was based on the Amirkola Health and Aging Project (AHAP) cohort. The 5–year survival rate of elderly people with diabetes and the factors that influence the mortality rate by Cox regression model were analyzed.
Results
Out of 1616 elderly people who were evaluated in the current study, 501 (31%) had diabetes. The results showed that diabetes significantly increased the mortality rate (adjusted hazard ratio [HR] = 2.10; 95% confidence interval [CI]: 1.57–2.81; P < 0.001). Furthermore, overweight (HR = 0.41; 95%CI: 0.24–0.75; P = 0.002), obesity (HR = 0.30; 95% CI: 0.41–0.63; P = 0.002), history of diabetes (HR = 0.56; 95%CI: 0.34–0.93; P = 0.024), moderate and high physical activity level (HR = 0.36; 95%CI: 0.13–0.99; P = 0.049) decreased the risk of mortality and central obesity (HR = 1.76; 95% CI: 1.01–3.11; P = 0.049), fasting blood sugar ≥200 (HR = 2.46; 95% CI: 1.46–4.15; P < 0.001), brain stroke, and neurological diseases (HR = 3.12; 95% CI: 1.78–5.49; P < 0.001) increased the risk of mortality.
Conclusion
Although overweight and obesity significantly improved the risk of mortality in elderly patients with diabetes, central obesity is still considered as an important risk factor.
Keywords: Obesity, Survival, Diabetes mellitus, Aging
Introduction
The prevalence of diabetes is increasing in several countries, and according to the International Diabetes Federation (IDF) 2015, about 415 million people have diabetes worldwide, which will increase to about 650 million people by 2040 [1]. Since diabetes is one of the most important non-communicable diseases worldwide, it has been a topic of interest. The number of studies on diabetes also increased in Iran, and most of these studies emphasize the outcomes, management, and genetic causes of diabetes [2]. Overweight and obesity are among the main important factors that are associated with type 2 diabetes, and several studies showed that a significant portion of patients with diabetes are also overweight or obese [3, 4]. However, recently, the obesity paradox, which addresses the lower rate of mortality in patients with diabetes [5], is one of the most controversial topics evaluated in a meta-analysis on [20] studies, and more than 250,000 patients showed the positive effect of overweight on the survival rate of patients with diabetes among all age groups and the positive effects of obesity on the survival rate of elderly people with diabetes [6].
Since diabetes, obesity, and old age are among the major health concerns in Iranian addition to the increasing prevalence of diabetes and obesity, the aging population has also become a threat in Iran [2, 7, 8]. At first, the survival rate of elderly people with diabetes and non-diabetes were compared, but the main aim of this study was to assess the effective factors on the survival of elderly patients with diabetes with special emphasis on the role of obesity and also to differentiate the effect of overweighting and obesity (Based on BMI) with central obesity (Based on waist circumference) on this patients, according to the Amirkola Health and Aging Project (AHAP) cohort [9, 10].
Materials and methods
The current study [9] was designed according to the AHAP cohort, which is the first cohort of the Iranian elderly population. Accordingly, a total of 1616 elderly people were recruited from 2011 to 2012, and their clinical and laboratory results were recorded, of which 501 participants had diabetes mellitus. The survival and mortality rates of the participants were recorded based on the follow-up data and second phase of AHAP in 2016 and 2017. In addition, the data of less than 5% of the participants were collected from the Iranian national mortality databases of the Iranian Ministry of Health and Medical Education, cemetery information systems, and the systems affiliated to the civil registration organization.
The study protocol was designed based on the ethical considerations in biomedical researchers, and it was approved by the Ethics Committee of Babol University of Medical Sciences, Babol, Iran. To assess the survival and mortality rates of the elderly people in the current study, the following variables were evaluated: age, gender, marital status, anthropometric indices, history of cardiovascular and neurological diseases, blood pressure, renal and liver failures, depression (based on the geriatric depression scale [GDS]), other chronic diseases (total of [25] diseases), social support (based on the Duke social support index [DSSI]), physical activity (based on the physical activity scale for the elderly [PASE]), muscular strength of the arm and quadriceps, history of smoking, and paraclinical parameters, such as fasting blood sugar (FBS) and ferritin (as an inflammatory index for chronic diseases). The method used for completing the questionnaires and scales was described in the AHAP cohort profile [9].
To diagnose patients with diabetes, the American Diabetes Association (ADA) guidelines [11] and/or the confirmed diagnosis of diabetes mellitus that is enclosed to the medical profile, including the consumption of antidiabetic drugs, were used. First, the crude and adjusted survival rate (based on age, gender, and number of chronic diseases) of the patients with diabetes, compared with patients who are not diabetic, were presented, and the factors that affect the survival rate of elderly patients with diabetes and the main objective of the study were also depicted.
Data were analyzed with SPSS. The qualitative data were analyzed using the chi-square test and compared with t-test.
The survival rate was analyzed using the Kaplan–Meier method, and the log-rank test was used to compare the survival rate among the different groups. The survival plot showed the 60-month survival rate of the elderly patients in the current study.
Crude and adjusted hazard ratios of Cox proportional hazard regressions and 95% confidence interval with performing bootstrapping technique for death during the follow-up period were calculated. The 2–tailed tests were used in the current study. A P value of <0.05 was considered as statistically significant.
Data availability
Please contact corresponding author for data requests.
Results
Out of 1616 elderly people enrolled in the current study, 501 (31%) had diabetes and 1115 (69%) were not diabetic. The mean ± standard deviation (SD) of the age of patients with and without diabetes was 68.69 ± 7.09 years and 69.67 ± 7.55 years, respectively (P = 0.014). Among the patients with diabetes, 46.5% were men and 53.5% were women. In non-diabetic cases, the rates were 58.3% and 41.7% in non-diabetic cases, respectively (P < 0.001). The mean values of non-diabetic chronic diseases in elderly patients with and without diabetes were 2.74 ± 1.97 and 2.29±1.77, respectively (P < 0.001). The 5–year survival rate and standard error of patients with and without diabetes were 82.8% ± 1.7% and 90.2% ± 0.9%, and the mean survival time of patients with and without diabetes were 55.34 months (95%CI: 54.27–56.41) and 57.20 (95%CI: 56.62–57.78) months, respectively(P < 0.001). Figure 1 shows the 60-month survival rate of the study groups.
Fig. 1.
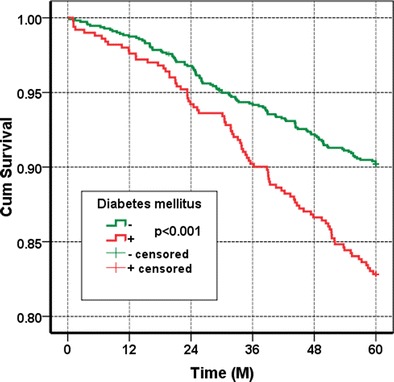
The 5-year survival curve of elderly individuals with and without diabetes
The crude hazard ratio of survival in diabetes 1.82 (95%CI: 1.37–2.41, P < 0.001), which was 2.10 (95%CI: 1.57–2.81, P < 0.001) for the adjusted HR.
Out of 501 elderly patients with diabetes, 7 were excluded because of incomplete data and missing test results, and 494 participants were continually assessed, of which 84 (17%) died within 5 years. The profile and mortality rate of the participants with diabetes for the evaluated variables are shown in Table 1.
Table 1.
The medical profile of Amirkola elderly patients with diabetes and the mortality rate based on the study variables
| Factors | Alive N = 410 | Dead N = 84 | p. value |
|---|---|---|---|
| BMI (kg/m2) | 0.001 | ||
| < 25 25–29.9 ≥ 30 |
80 (71.4%) 201 (85.2%) 129 (88.4%) |
32 (28.6%) 35 (14.8%) 17 (11.6%) |
|
| Gender | 0.044 | ||
| Male Female |
185 (79.4%) 225 (86.2%) |
48 (20.6%) 36 (13.8%) |
|
| Age (year) | 0.000 | ||
| 60–69 70–70 ≥ 80 |
269 (90.9%) 122 (77.2%) 19 (47.5%) |
27 (9.1%) 36 (22.8%) 21 (52.5%) |
|
| Cardiovascular diseases | 0.000 | ||
| + - |
132 (78.6%) 278 (85.3%) |
36 (21.4%) 48 (14.7%) |
|
| Hypertension | 0.273 | ||
| + - |
288 (81.8%) 122 (85.9%) |
64 (18.2%) 20 (14.1%) |
|
| CVA and neurological diseases | 0.000 | ||
| + - |
27 (57.4%) 383 (85.7%) |
20 (42.6%) 64 (14.3%) |
|
| WC | 0.869 | ||
| ≥ 95 < 95 |
248 (83.2%) 162 (82.1%) |
50 (16.8%) 34 (17.3%) |
|
| Marital status | 0.051 | ||
| Single Married |
66 (75.9%) 344 (84.5%) |
21 (24.1%) 63 (15.5%) |
|
| Smoking | 0.068 | ||
| + - |
64 (76.2%) 346 (84.4%) |
20 (23.8%) 64 (15.6%) |
|
| Depression | 0.068 | ||
| + - |
209 (81.6%) 201 (84.5%) |
47 (18.4%) 37 (15.5%) |
|
| Known DM | 0.044 | ||
| + - |
316 (84.9%) 94 (77%) |
56 (15.1%) 28 (23%) |
|
| FBS | 0.064 | ||
| ≥ 200 mg/dL < 200 mg/dL |
80 (76.9%) 330 (84.6%) |
24 (23.1%) 60 (15.4%) |
|
| Ferritin | 0.167 | ||
| ≥ 200 ng/mL < 200 ng/mL |
181 (80.4%) 229 (85.1%) |
44 (19.6%) 40 (14.9%) |
|
| Creatinine | 0.030 | ||
| ≥ 1 mg/dL < 1 mg/dL |
117 (77.5%) 293 (85.4%) |
34 (22.5%) 50 (14.6%) |
|
| Social support | 0.016 | ||
| DSSI≥ 25 DSSI< 25 |
315 (85.4%) 95 (76%) |
54 (14.6%) 30 (24%) |
|
| Physical activity | 0.001 | ||
| ≥ 150 < 150 |
83 (95.4%) 527 (80.3%) |
4 (4.6%) 80 (19.7%) |
|
| Muscle strength (arm) | 0.349 | ||
| ≥ 25 kg < 25 kg |
169 (84.9%) 241 (81.7%) |
30 (15.1%) 54 (18.3%) |
|
| Muscle strength (quadriceps) | 0.258 | ||
| ≥ 25 kg < 25 kg |
128 (85.9%) 282 (81.7%) |
21 (14.1%) 63 (18.3%) |
According to the main objective of the study, the association between mortality and body mass index (BMI) in elderly patients with diabetes was assessed using the survival analysis method and the Kaplan–Meier elderly survival curve based on BMI (Fig. 2), according to which, the 5–year survival rate and standard error for the elderly patients with diabetes for BMI<25–29.9, and ≥30 kg/m2 was 71.4% ± 4.3%, 85.2% ± 2.3%, and 88.4% ± 2.7%, respectively (P = 0.001).
Fig. 2.
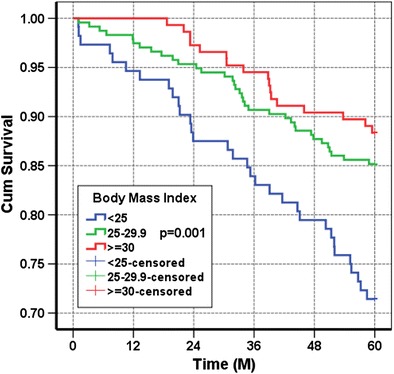
The 5–year survival curve of elderly patients with diabetes based on the BMI score
Using the Cox regression method, the crude and adjusted HRs was calculated for all study variables, including BMI (Table 2).
Table 2.
The Cox regression analysis for the indices that influence the survival rate of elderly patients with diabetes
| Factorsa | Simple | Multivariable (Model 1) b | Multivariable Model 2)c | Multivariable (Model 3) d | ||||
|---|---|---|---|---|---|---|---|---|
| Crude hazard ratio (CI95%) | P.value | Adjusted Hazard ratio (CI95%) | P.value | Adjusted hazard ratio (CI95%) | P.value | Adjusted hazard ratio (CI95%) | P.value | |
| BMI (kg/m2) | ||||||||
| < 25 25–29.9 ≥ 30 | 10.48 (0. 29–0.78) 0.37 (0. 20–0.66) |
0.001 0.003 0.001 |
10.41 (0. 24–0.72) 0. 30 (0. 14–0.63) |
- 0.002 0.002 |
1 0.41 (0. 19–0.79) 0. 30 (0. 11-0.70) |
- 0.009 0.009 |
1 0.41 (0. 24–0.70) 0.34 (0. 17–0.69) |
- 0.001 0.003 |
| Gender (male) | 1.54 (0.99–2.37) | 0.051 | 1. 21 (0.65–2. 28) | 0.545 | 1. 21 (0.56–2.78) | 0.622 | ||
| Age (1 year) | 1.11 (1.08–1. 14) | 0.000 | 1.08 (1.05–1. 12) | 0.000 | 1.08 (1.05–1. 13) | 0.001 | 1.09 (1.06–1. 13) | 0.000 |
| Cardio vascular diseases | 1.51 (0.98–2.33) | 0.060 | 1.38 (0.86–2. 20) | 0.180 | 1.38 (0.82–2.45) | 0.226 | ||
| Hypertension | 1.32 (0.80–2. 18) | 0.278 | 1.11 (0.66–1.88) | 0.688 | 1.11 (0.70–2. 15) | 0.679 | ||
| CVA and neurological diseases | 3.47 (2. 10-5.73) | 0.000 | 3. 12 (1.78–5.49) | 0.000 | 3. 12 (1.60–6.2) | 0.001 | 3. 29 (1.91–5.64) | 0.000 |
| WC ≥95 cm | 0.96 (0.62–1.48) | 0.847 | 1.76 (1.01–3.11) | 0.049 | 1.76 (0.94–3.94) | 0.083 | 1.75 (1.03–2.98) | 0.040 |
| Marital status (single) | 1.63 (0.99–2.67) | 0.052 | 1.39 (0.82–2.38) | 0.225 | 1.39 (0.74–2.53) | 0.226 | ||
| Smoking | 1.62 (0.98–2.67) | 0.061 | 1.62 (0.86–2.99) | 0.125 | 1.62 (0.73–3.58) | 0.198 | 1.58 (0.94–2.65) | 0.083 |
| Depression | 1. 19 (0.78–1.84) | 0.423 | 1.02 (0.61–1.70) | 0.936 | 1.02 (0.58–1.89) | 0.947 | ||
| Known DM | 0.63 (0.40–0.99) | 0.627 | 0.56 (0.34–0.93) | 0.024 | 0.56 (0.31–0.96) | 0.028 | 0.62 (0.38–1.01) | 0.053 |
| FBS ≥ 200 mg/dL | 1.57 (0.98–2.53) | 0.061 | 2.46 (1.46–4. 15) | 0.001 | 2.46 (1.35–4.57) | 0.001 | 2. 29 (1.38–3.80) | 0.001 |
| Ferritin ≥200 ng/mL | 1.35 (0.88–2.07) | 0.169 | 1.56 (0.99–2.46) | 0.053 | 1.56 (0.96–2.73) | 0.071 | ||
| Creatinine≥1 mg/dL | 1.61 (1.04–2.49) | 0.031 | 1.10 (0.66–1.83) | 0.726 | 1.10 (0.57–1.99) | 0.757 | ||
| Social support (DSSI≥ 25) | 0.58 (0.37–0.90) | 0.016 | 0.93 (0.57–1.54) | 0.781 | 0.93 (0.51–1.68) | 0.786 | ||
| Physical activity (≥150) | 0. 22 (0.08–0.59) | 0.003 | 0.36 (0. 13–0.99) | 0.049 | 0.36 (0.06–0.81) | 0.034 | 0.34 (0. 12–0.93) | 0.035 |
| Muscular strength (arm ≥25 kg) | 0.80 (0.51–1. 25) | 0.321 | 0.63 (0.32–1. 22) | 0.168 | 0.63 (0.32–1. 22) | 0.231 | ||
| Muscular strength (quadriceps ≥25 kg) | 0.74 (0.45–1. 22) | 0.742 | 1. 12 (0.56–2. 24) | 0.744 | 1. 12 (0.56–2. 24) | 0.767 | ||
aAll calculations were performed as the presence of these factors versus the absence of the factors.
bModel 1: The all independent variables/predictors were included Cox Proportional Hazard (CPH) regression.
cModel 2: The all independent variables/predictors were included CPH regression and performing the Bootstrap method.
dModel 4: The automatic backward CPH regression method that excluding p value criteria are 0.10.
Data in Table 2 are shown, including all the variables in the model. The Cox regression analysis was performed using the backward method, and lastly, age, BMI, level of FBS, brain stroke and other neurological diseases, physical activity, waist circumference (WC), previously diagnosed diabetes, and history of smoking were the only variables retained in the model. In the last step, when the remaining variables were included, overweight and obesity significantly declined the risk of mortality in elderly patients with diabetes, while central obesity (WC ≥ 95 cm) is still considered as an important risk factor.
When the paradoxical effect of obesity and central obesity on the survival rate of elderly patients with diabetes is considered, the effect of BMI was also assessed on the same population, based on WC, and the results showed that BMI had a significant protective effect on the survival rate of elderly patients without central obesity (age and gender were adjusted; HR =0.39; 95%CI: 0.18–0.87; P = 0.021). In patients with central obesity (WC ≥95), BMI was also considered a protective index. However, it was not statistically significant (age and gender were adjusted; HR = 0.60; 95%CI: 0.27–1.37; P = 0.231).
Discussion
According to the results of the current study, more than 30% of elderly patients had diabetes, while in a study in 2011 that used the same sample size, the prevalence of diabetes was 23%, which was based on the data collected via questionnaires and medical records [12]. The difference between the rates can be attributed to the tests and unknown diabetic cases in the current study. In a study conducted in UK, Zghebi SS et al. [13] evaluated the prevalence, incidence, and mortality rate of diabetes from 2004 to 2014, and despite the increasing prevalence of diabetes, a lower mortality rate and HR of<1.5 were observed in patients with diabetes compared with patients without diabetes. In Turkey, another study also showed that diabetes was not associated with mortality rate [14]; however, in the current study, a higher HR of 2 was observed in elderly patients with diabetes compared with patients who were not diabetic after adjusting for age, gender, and chronic diseases. In the current study, a higher HR was observed, and this might be due to the substantial role of healthcare systems in the survival of elderly patients with diabetes. However, the world population is aging, and the prevalence of diabetes is significantly increasing. Hence, the number of elderly patients with diabetes has unexpectedly increased. Old age and diabetes are among the risk factors for functional disability, and the results of a meta-analysis by Wong et al. also showed that diabetes is associated with the increased risk of physical impairments, particularly in elderly people [15]. Therefore, the health policy-makers should focus on the factors that influence the health status of elderly patients with diabetes, particularly in developing countries. Anthropometric indices are among the simplest and most acceptable health status measurement tools that are applicable to all age groups, including the elderly population, and these tools are also used in epidemiologic studies, particularly in survival analyses [16]. Advanced reduction in muscular mass, specifically in the lower limbs, and increase in fat mass, particularly visceral and intramuscular fat, are among the main aging-associated changes [17, 18]. Elderly patients with diabetes usually have lower muscular mass and strength. In addition, the muscular quality is poor among these patients [19]. Although the association between obesity and diabetes is well known, dynapenic obesity with a high BMI score and low muscular strength is a remarkable challenge for elderly people. Moreover, these conditions reduce functioning abilities [20]. In a longitudinal study by Cuthbertson et al., a relationship was observed between dynapenic obesity with a high BMI score and low muscular strength and diabetes in elderly people [3].
Different studies indicated the relationship between sarcopenia and mortality in elderly people [21, 22]. Since sarcopenia could not be identified during the first phase of the current study, this weakness was obvited in the second phase of the study by using the soft tissue scan and some recently developed tests [10]. But, we considered approximate index for evaluating the muscular performance with measuring muscular strength of the arm and quadriceps, and also the physical activity of the patients and as shown increased physical activity reduced the risk of mortality in the studied participants. Therefore, a low muscle mass, which is associated with muscular dystrophy, increases the risk of mortality. In fact, the evaluation of muscular strength is an intermediary factor to determine the positive effect of BMI on the survival rate of elderly patients with diabetes. In a study by Murphy RA et al., similar results were observed, and the leg muscle mass had a significant role in the reduction of mortality rate in such patients [23]. In this study, with multivariable analysis, we also showed that in spite of central obesity induced by fat mass increases the risk of mortality in the elderly patients with diabetes thus, BMI has positive effect on the survival of these individuals that it can be related to the role of muscle mass. Different studies also showed the relationship between muscular dystrophy and insulin resistance [24, 25]. For examples, the studies showed patients find it hard to control diabetes after the reduction of muscular mass and increase of insulin resistance, which exacerbates the health status of elderly patients and increases the risk of mortality. On the other hand, other studies evaluated the relationship between serum ferritin level and insulin resistance [26] as well as the effect of smoking on the reduction of insulin secretion and increase of insulin resistance [27]. In the present study, a higher mortality rate was observed in smokers with high ferritin level, although the relationship was statistically insignificant, which can be attributed to the small sample size of the current study or the ethnic habits of elderly people from the North of Iran, of which a small number of elderly women in this region smoke and most of the smokers are men. Another remarkable finding of the current study was the significant association of neurological diseases and brain stroke with diabetes, which affects the increased mortality among elderly people. Based on the results of other studies, about 20% of total death from diabetes was caused by brain stroke, which is more frequent than in non-diabetic cases [28]. Since the control of diabetes can reduce the risk of brain stroke and even decrease the risk of mortality in individuals who developed brain stroke [29], such patients should be the main focus. In addition, the role of BMI and muscular strength in the rehabilitation of elderly patients with diabetes and brain stroke and the reduction of mortality rate in such patients should be further investigated. Also, high consumption of carbohydrate and low intake of protein along with declined physical activity from preliminary analysis of second phase of AHAP [30] could explain dynapenic obesity in this population so this issue should be considered in dietary intervention for improving life expectancy.
The current study included a community-based cohort that was the first elderly cohort in Iran, and comprehensive information was provided, which is considered the strength of the current study. However, some of the limitations of the present study include the use of a small sample size, as well as incomplete results of serum HbA1c. To overcome this limitation, this index was excluded, and FBS was replaced with a weaker index to indicate the control of diabetes. However, other studies should be conducted to check the succeeding phases of the AHAP cohort via longer follow-up periods and to resolve the study limitations.
Conclusion
In the present study, although overweight and obesity could significantly decrease the risk of mortality among elderly patients with diabetes through positive effects in muscular mass, central obesity is still considered as a risk factor.
Acknowledgements
The authors would like to thank all authorities of Babol University of Medical Sciences,
AHAP collaboration and the elderly participants of this project.
Abbreviations
- AHAP
amirkola health and ageing project
- BMI
body mass index
- CI
confidence interval
- CPH
cox proportional hazard
- CVA
cerebrovascular accident
- DM
diabetes mellitus
- DSSI
duke social support index
- FBS
fasting blood sugar
- GDS
geriatric depression scale
- IDF
international diabetes federation
- PASE
physical activity scale for elderly
- WC
waist circumference
Author contributions
AB, SRH, RC and RG conceived and designed the study. AB, MY, RR and AS gathered the data. AB performed the statistical analysis. AB drafted the manuscript. SRH and RG critically revised the manuscript. All authors read and approved the final manuscript.
Funding
This study has been financially supported by the Research and Technology Deputy of Babol University of Medical Sciences with grant number 9440021.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Our study was reviewed and approved by ethics committee, Babol University of Medical Sciences.
References
- 1.Rahelić D. 7th edition of IDF diabetes atlas-call for immediate action. Lijec Vjesn. 2016;138(1–2):57–58. [PubMed] [Google Scholar]
- 2.Nasli-Esfahani E, Farzadfar F, Kouhnavard M, Ghodssi-Ghassemabadi R, Khajavi A, Peimani M, et al. Iran diabetes research roadmap (IDRR) study: a preliminary study on diabetes research in the world and Iran. J Diabetes Metab Disord. 2017;16(9) 10.1186/s40200-017-0291-9. https://www.ncbi.nlm.nih.gov/pubmed/?term=28239599. [DOI] [PMC free article] [PubMed]
- 3.Cuthbertson DJ, Bell JA, Ng SY, Kemp GJ, Kivimaki M, Hamer M. Dynapenic obesity and the risk of incident type 2 diabetes: the English longitudinal study of ageing. Diabet Med. 2016;33(8):1052–1059. doi: 10.1111/dme.12991. [DOI] [PubMed] [Google Scholar]
- 4.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290(14):1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 5.Carnethon MR, Rasmussen-Torvik LJ, Palaniappan L. The obesity paradox in diabetes. Curr Cardiol Rep. 2014;16(2):446. doi: 10.1007/s11886-013-0446-3. [DOI] [PubMed] [Google Scholar]
- 6.Gao F, Wang ZJ, Shen H, Yang SW, Nie B, Zhou YJ. Impact of obesity on mortality in patients with diabetes: meta-analysis of 20 studies including 250,016 patients. J Diabetes Investig 2017; 10.1111/jdi.12677. [Epub ahead of print] https://www.ncbi.nlm.nih.gov/pubmed/28593750. [DOI] [PMC free article] [PubMed]
- 7.Hajian-Tilaki KO, Heidari B. Prevalence of obesity, central obesity and the associated factors in urban population aged 20-70 years, in the north of Iran: a population-based study and regression approach. Obes Rev. 2007;8(1):3–10. doi: 10.1111/j.1467-789X.2006.00235.x. [DOI] [PubMed] [Google Scholar]
- 8.Noroozian M. The elderly population in Iran: an ever growing concern in the health system. Iran J Psychiatry Behav Sci. 2012;6(2):1–6. [PMC free article] [PubMed] [Google Scholar]
- 9.Hosseini SR, Cumming RG, Kheirkhah F, Nooreddini H, Baiani M, Mikaniki E, Taghipour-darzi M, Akhavan Niaki H, Rasolinejad SA, Mostafazadeh A, Parsian H, Bijani A. Cohort profile: the Amirkola health and ageing project (AHAP) Int J Epidemiol. 2014;43(5):1393–1400. doi: 10.1093/ije/dyt089. [DOI] [PubMed] [Google Scholar]
- 10.Bijani A, Ghadimi R, Mikaniki E, Kheirkhah F, Mozaffarpur SA, Motallebnejad M, Esmaili H, Majidi F, Cumming RG, Hosseini SR. Cohort profile update: the Amirkola health and ageing project (AHAP) Caspian J Intern Med. 2017;8(3):205–212. doi: 10.22088/cjim.8.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 2013; 36 (Suppl 1): S67-S74. 10.2337/dc13-S067, Diagnosis and Classification of Diabetes Mellitus. [DOI] [PMC free article] [PubMed]
- 12.Hosseini SR, Cumming RG, Sajjadi P, Bijani A. Chronic diseases among older people in Amirkola, northern Islamic Republic of Iran. East Mediterr Health J. 2011;17(11):843–849. doi: 10.26719/2011.17.11.843. [DOI] [PubMed] [Google Scholar]
- 13.Zghebi SS, Steinke DT, Carr MJ, Rutter MK, Emsley RA, Ashcroft DM. Examining trends in type 2 diabetes incidence, prevalence and mortality in the UK between 2004 and 2014. Diabetes Obes Metab. 2017;19:1537–1545. doi: 10.1111/dom.12964. [DOI] [PubMed] [Google Scholar]
- 14.Onat A, Hergenç G, Uyarel H, Can G, Ozhan H. Prevalence, incidence, predictors and outcome of type 2 diabetes in Turkey. Anadolu Kardiyol Derg. 2006;6(4):314–321. [PubMed] [Google Scholar]
- 15.Wong E, Backholer K, Gearon E, Harding J, Freak-Poli R, Stevenson C, Peeters A. Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013;1(2):106–114. doi: 10.1016/S2213-8587(13)70046-9. [DOI] [PubMed] [Google Scholar]
- 16.Dhana K, Kavousi M, Ikram MA, Tiemeier HW, Hofman A1, Franco OH. Body shape index in comparison with other anthropometric measures in prediction of total and cause-specific mortality. J Epidemiol Community Health 2016; 70(1):90–96. https://www.ncbi.nlm.nih.gov/pubmed/26160362. [DOI] [PubMed]
- 17.Newman AB, Lee JS, Visser M, Goodpaster BH, Kritchevsky SB, Tylavsky FA, Nevitt M, Harris TB. Weight change and the conservation of lean mass in old age: the health, aging and body composition study. Am J Clin Nutr. 2005;82:872–878. doi: 10.1093/ajcn/82.4.872. [DOI] [PubMed] [Google Scholar]
- 18.Hughes VA, Frontera WR, Roubenoff R, Evans WJ, Singh MA. Longitudinal changes in body composition in older men and women: role of body weight change and physical activity. Am J Clin Nutr. 2002;76:473–481. doi: 10.1093/ajcn/76.2.473. [DOI] [PubMed] [Google Scholar]
- 19.Jang HC. Sarcopenia, frailty, and diabetes in older adults. Diabetes Metab J. 2016;40(3):182–189. doi: 10.4093/dmj.2016.40.3.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bouchard DR, Janssen I. Dynapenic-obesity and Physical function in older adults. J Gerontol A Biol Sci Med Sci 2010; 65(1):71–77. https://www.ncbi.nlm.nih.gov/pubmed/19887536. [DOI] [PubMed]
- 21.Brown JC, Harhay MO, Harhay MN. Sarcopenia and Mortality among a population-based sample of community-dwelling older adults. J Cachexia Sarcopenia Muscle. 2016;7(3):290–298. doi: 10.1002/jcsm.12073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim JH, Lim S, Choi SH, Kim KM, Yoon JW, Kim KW, Lim JY, Park KS, Jang HC, Kritchevsky S. Sarcopenia: an independent predictor of mortality in community-dwelling older Korean men. J Gerontol A Biol Sci Med Sci. 2014;69(10):1244–1252. doi: 10.1093/gerona/glu050. [DOI] [PubMed] [Google Scholar]
- 23.Murphy RA, Reinders I, Garcia ME, Eiriksdottir G, Launer LJ, Benediktsson R, Gudnason V, Jonsson PV, Harris TB, Age, Gene/Environment Susceptibility-Reykjavik Study (AGES-Reykjavik). Age, gene/environment susceptibility-Reykjavik study (AGES-Reykjavik). Adipose tissue, muscle, and function: potential mediators of associations between body weight and mortality in older adults with type 2 diabetes. Diabetes Care 2014; 37(12): 3213–3219.https://www.ncbi.nlm.nih.gov/pubmed/?term=25315206. [DOI] [PMC free article] [PubMed]
- 24.Srikanthan P, Karlamangla AS. Relative muscle mass is inversely associated with insulin resistance and prediabetes. Findings from the third National Health and nutrition examination survey. Format: Abstract J Clin Endocrinol Metab. 2011;96(9):2898–2903. doi: 10.1210/jc.2011-0435. [DOI] [PubMed] [Google Scholar]
- 25.Carnethon MR, De Chavez PJ, Biggs ML, Lewis CE, Pankow JS, Bertoni AG, et al. Association of weight status with mortality in adults with incident diabetes. JAMA. 2012;308(6):581–590. doi: 10.1001/jama.2012.9282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cho MR, Park JK, Choi WJ, Cho AR, Lee YJ. Serum ferritin level is positively associated with insulin resistance and metabolic syndrome in postmenopausal women: a nationwide population-based study. Maturitas. 2017;103:3–7. doi: 10.1016/j.maturitas.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Morimoto A, Tatsumi Y, Deura K, Mizuno S, Ohno Y, Watanabe S. Impact of cigarette smoking on impaired insulin secretion and insulin resistance in Japanese men: the Saku study. Journal of Diabetes Investigation. 2013;4(3):274–280. doi: 10.1111/jdi.12019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 2010; 375(9733): 2215–2222 https://www.ncbi.nlm.nih.gov/pubmed/?term=20609967. [DOI] [PMC free article] [PubMed]
- 29.Lieber BA, Taylor B, Appelboom G, Prasad K, Bruce S, Yang A, Bruce E, Christophe B, Connolly ES., Jr Meta-analysis of telemonitoring to improve HbA1c levels: promise for stroke survivors. J Clin Neurosci. 2015;22(5):807–811. doi: 10.1016/j.jocn.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 30.Bijani A, Esmaili H, Ghadimi R, Babazadeh A, Rezaei R, Cumming RG, et al. Development and validation of a semi-quantitative food frequency questionnaire among older people in north of Iran. Caspian J Intern Med. 2018;9(1):78–86. doi: 10.22088/cjim.9.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Please contact corresponding author for data requests.


