Abstract
This study examined the interplay of depression and different types of e-health interventions on breast cancer patients’ perceived healthcare competence, emotional processing, and social well-being over time. The three e-health interventions - Internet Only as a control condition, CHESS (Comprehensive Health Enhancement Support System) Only, and CHESS with a Human Mentor, a cancer information specialist - provided varying degrees of interactivity and presence. A total of 328 women with breast cancer participated in one of the three interventions for a 6-month period. Women were further split into two groups based on reported levels of depression. For perceived healthcare competence and social well-being, results revealed significant interaction effects for intervention type by depression over time, such that breast cancer patients with higher levels of depression benefited most from the CHESS with Mentor intervention over the 6-month study period. For emotional processing, depressed cancer patients benefited more from the CHESS with Mentor than the other two interventions, regardless of time. These findings have (a) theoretical implications on how mental health factors can intersect with interactivity and presence to influence psychosocial outcomes, (b) conceptual implications for the role of human interaction within e-health systems, and (c) practical implications for the development of e-health interventions for cancer patients with depression.
Keywords: Interactivity, Presence, e-Health, Comprehensive Health Enhancement Support System (CHESS), Human cancer mentor, Healthcare competence, Psychosocial well-being
Breast cancer is the most commonly diagnosed cancer, except skin cancer, and the second leading cause of cancer death in women in the United States (American Cancer Society, May 2017). Dealing with a breast cancer diagnosis and treatments is associated with heightened social concerns and psychological challenges such as loneliness (Anderson, 1992), distress, depression, and anxiety (Satin, Linden, & Phillips, 2009). One common way that cancer patients cope with their illness is by exploring the Internet for health information, education and support.
A national survey found that 68% of Internet users living with chronic illnesses have looked online for information about a specific disease or a medical problem such as cancer (Fox & Purcell, 2010). Also, 28% of those with chronic conditions reported they have searched online for mental health related information, including topics such as depression, anxiety, or emotional and social distress. Patients indicated that their online information seeking activities contributed to improved treatment decisions, doctor-patient communications, and abilities to cope with health challenges. For breast cancer patients, the Internet is a primary source of information after their healthcare providers (Shaw, Han, & Hawkins et al., 2007). Research has found that women with breast cancer more actively sought out cancer-related information online when they had a low level of support from their social networks combined with a high level of emotional stability. This suggests that those lacking information support from within their existing networks compensate for that void through online information seeking if they have the resources associated with emotional well-being (Kim, Shah, Namkoong, McTavish, & Gustafson, 2013).
Using e-health interventions such as Interactive Cancer Communication Systems (ICCSs) can contribute to better health outcomes among chronic illness patients (Gustafson et al., 2001, 2005, 2008). While the use of ICCSs has been found to confer benefits in both clinical trials and population studies, research suggests that the picture is more nuanced. Different combinations of e-health service use (e.g., Lu, Shaw, & Gustafson, 2011; Shaw, Han, Hawkins et al., 2007), longitudinal use patterns (Han et al., 2009), and distinctive activity type within specific services (Shaw, Han, Hawkins, McTavish, & Gustafson, 2008) – individually or in combination – contribute to outcomes of interest in different ways. This study explores these issues in greater depth, examining three different e-health interventions that vary in interactivity and presence and considering how their over time effects might be moderated by cancer patients’ mental health.
Depression among Cancer Patients
Based on a recent meta-analysis (Satin et al., 2009), depression has been recognized as the most common mental health problem cancer patients face, a frequently experienced comorbidity (Longman, Braden, & Mishel, 1999). Previous research has also found that symptoms of depression are a predictor for and negatively associated with psychosocial and physical functioning (Holzberg, Robinson, Geisser, & Gremillion, 1996), increase anxiety and pain levels (McDonald Passik, Dugan, Rosenfeld, Theobald, & Edgerton, 1999), and contribute to insomnia and difficulty in concentrating (Dow, Ferrell, Leigh, Ly, & Gulasekaram, 1996). Also, depression tends to be persistent throughout the illness trajectory and is consistently associated with biological cancer progression and mortality rates (Saul et al., 2005). Other research confirmed that depression is one of the key predictors for diminished quality of life (Fredrickson, 2001; Visser & Smets, 1998), poorer medical treatment adherence, and longer stays in hospitals (Badger, Braden, Mishel, & Longman, 2004; Spiegel, 1997) among women with breast cancer. Research also confirms that cancer patients’ relevant information seeking could be discouraged by unexpected or unintended psychological fluctuations such as emotional trauma or mood disturbance caused by disease-related experiences (Harris, 1998).
Despite the considerable evidence that depression is common among breast cancer patients and diminishes their quality of life at an already difficult time in their lives, often times the symptoms of depression are unrecognized and therefore it remains untreated (Badger et al., 2004; Newport & Nemeroff, 1998). Moreover, despite substantial evidence supporting the positive effects of psychosocial interventions, including e-health interventions, in improving cancer patients’ psychological adjustment and quality of life, these interventions have not been readily available and targeted to cancer patients with different levels of depression. In other words, potential conditional effects of depression on different health outcomes have not been systematically examined related to the development and implementation of e-health interventions. Most of what we do know comes form face-to-face, community-based interventions (Badger et al., 2004; Spiegel & Giese-Davis, 2003), which depressed breast cancer patients may not have the inclination or energy to engage. To date, these community-based studies have offered descriptive findings and only used cross-sectional data to explore such intervention effects at one point in time (Badger et al., 2004).
This study responds to this dearth by exploring how breast cancer patients with and without depression benefit from different types of e-health interventions over a 6-month period. Determining what types of health support services are necessary to confer positive patient outcomes has practical implications, particularly for depressed patients who not only may be having a harder time coping with their illness but who are also heavier users of clinical services, placing higher demands on the healthcare system. Because e-health interventions require considerable time and money to design, develop, and maintain, determining what type of intervention is most effective to support depressed patient populations can help developers make cost-effective decisions for patient support. This study also provides insights about how patients with depression may improve over time by using an e-health intervention.
Interactivity, Presence, and Cancer Management in e-Health Intervention
Generally speaking, e-health interventions can offer potential benefits to patients. Such systems, however, can offer different configurations of services, with health outcomes varying depending on the features available to users. One way to think about the quality and quantity of services provided to patients is through the concepts of ‘presence’ and ‘interactivity.’
Interactivity has been a core concept when explaining features of online communication technologies, with a particular focus on its ability to tailor content to individual users (Walther, Pingree, Hawkins, & Buller, 2005). Since a primary goal of an e-health intervention system is to promote and encourage desired health outcomes among targeted patients, this study supports an approach of defining interactivity as “an attribute of communication exchanges, in this case between the system and its users” (Hawkins, Han, Pingree et al., 2010, p. 2). Previous studies have found beneficial effects of using interactive technologies on various cognitive outcomes, including learning, involvement, continuous adherence to subsequent communication exchanges, as well as the persuasiveness of the intervention resources (Hawkins, Han, Pingree et al., 2010).
Social presence, when applied to e-healthcare settings, is defined as the patient (the user) experiencing interpersonal ‘person-like’ qualities from either within the e-health systems or the people behind those systems. With high levels of social presence, a patient can be encouraged to seek out instructional help, establish a sense of mutual trust and emotional support, decrease disease-related concerns, and effectively handle social relationship challenges (Hawkins, Han, Pingree et al., 2010). Lee (2004) suggests that in a computer-mediated environment, the feeling of presence is closely related to the feeling of interactivity.
Thus, when developing an e-health system that provides more tailored services, both interactivity and social presence should be taken into consideration to maximize patient health benefits. These features of e-health intervention systems also enable users to develop autonomy and self-confidence to cope more effectively with their illnesses. Higher levels of perceived interactivity and presence can lead to reducing emotional distress, cancer-related concerns, and improve quality of life (Hawkins, Pingree, Shaw et al., 2010; Ryan & Deci, 2000; Sheldon, Williams, & Joiner, 2003). E-health intervention systems such as CHESS (Comprehensive Health Enhancement Support System) provide high degrees of interactivity and presence by emphasizing user control and social interaction. Use of well-designed e-health interventions can, under these situations, lead to significant improvement of different patient health outcomes.
For example, Gustafson and colleagues (2001) explored potential beneficial effects of the CHESS intervention with newly diagnosed breast cancer patients. After two months, patients reported enhanced competence in healthcare participation and in interactions with doctors, and greater information-seeking intentions. At the five-month follow-up, patients also experienced greatly enhanced social support and information competence. In another study, they found significant, positive effects of using CHESS on perceived social support among cancer patients. These benefits remained even after the CHESS intervention had ended. Conversely, simple access to Internet resources was found to be of little or no benefit to patient care, despite containing links to a series of quality health sites (Gustafson, Hawkins, McTavish et al., 2008).
Work by Hawkins et al. (2011) examined potential benefits of integrating a human cancer mentor with the CHESS intervention for breast cancer patients. Results suggested that compared to the only Internet access, the CHESS and mentor-combined intervention enhanced information competence and emotional processing strategies of breast cancer patients at six weeks and three months compared to baseline. Another study reporting on the same experimental design confirmed that the CHESS and mentor-combined condition has the highest levels of perceived interactivity and presence among breast cancer patients when followed by CHESS alone and cancer mentor alone, and then the Internet-only conditions (Hawkins, Han et al., 2010). These results have substantial implications for how to improve current e-health interventions.
Although some online sites provide credible cancer information along with communication or interactive services, these sites tend to offer less than CHESS in terms of service integration and systematic support. Breast cancer patients also face information redundancy, information overload, and information omission, along with questionable medical claims for profit when exploring online themselves (Hawkins, Han et al., 2010). As such, it is not surprising that perceptions of interactivity and presence are maximized under the CHESS with Mentor condition given the interactivity and tailoring built into the system when combined with human presence provided by the cancer mentor, who was available to provide timely and individualized services to patients. The three conditions examined in this study, Internet Only, CHESS Only, and CHESS with Mentor, were provided with the goal of increasing presence and interactivity — the Internet Only providing minimal interactivity and presence, CHESS Only giving a moderate level of both, and CHESS with Mentor offering the most interactivity and presence. The benefits of the CHESS with Mentor intervention were expected to be greatest due to the potential synergetic effects from simultaneous use of both computer-mediated CHESS and interpersonal Mentor health services (Hawkins et al., 2011).
Hypotheses and Research Questions
Based on the above discussion, the following hypotheses and research question were proposed. Our first ancillary hypothesis was that 1) depression would be associated with worse health outcomes at baseline and over time as found in previous research. Our primary hypothesis was that 2) women with breast cancer who are depressed would obtain greater health benefits from the e-health intervention that provides higher levels of interactivity and presence, primarily because they have greater needs to begin with and thus have a greater gap to close as compared to patients who are not depressed. The final exploratory research question was 3) whether psychosocial health benefits breast cancer patients with depression would obtain from the e-health intervention with higher levels of interactivity and presence would be greater over time, compared to those who are not depressed.
Method
Recruitment Procedure
Study participant recruitment was conducted at three different cancer centers across the U.S. (in Wisconsin, Connecticut, and Texas). Among a total of 1,034 women who were initially approached for study participation, this study focuses on 328 who were randomly assigned to one of three intervention conditions (Internet Only, CHESS Only, and CHESS with Mentor). Random assignment of study participants was implemented through a computer-generated list concealing upcoming assignments managed by site research managers (Baker et al., 2011).
Brochures were distributed to recruit study participants at relevant locations and clinical staff training meetings. Researchers asked eligible individuals if they would be interested in participating in the study. If agreed, researchers explained the informed consent, HIPAA information, and the intervention details, and answered questions from patients. Researchers then collected written consent, contact information and distributed the baseline survey for completion. Only participants over 17 years old, literate in English, and within two months of a primary breast cancer diagnosis or recurrence were included in the study (Baker et al., 2011).
Survey data were collected at pretest (baseline) as well as three (T1) and six months (T2) after receiving the intervention. Patients completed the pretest and follow-up surveys and mailed them back after completion. The longitudinal nature of the data provided the opportunity to parse out whether, when, to what degree, intervention effects occurred (Baker et al., 2011).
Intervention Assignment
Once the consent form and baseline survey were received, participants were randomized to conditions (Internet Only, CHESS Only, or CHESS with Mentor) and asked about their technological needs. A computer and/or Internet access were provided to patients who needed them. Internet service provider costs were paid in full for participants for the entire 6-month study period. Study participants in the CHESS Only or CHESS with Mentor were offered training on how to use the CHESS system and received a user guide to supplement training. Patients who were assigned to the Internet Only condition received training on how to use search engines like Google. The average training time was around 30 minutes (Baker et al., 2011).
Intervention Type
Internet Only.
This control condition represented the norm for patients with Internet access without other intervention access. Thus, this design did not test whether e-health intervention access per se was effective, but rather whether various high-quality, integrated e-health interventions would be effective relative to unguided, open Internet access. Patients were provided a list of respected cancer-related websites that included information that was low in interactivity and presence (e.g., Baker et al., 2011; Hawkins, Pingree et al., 2010).
CHESS Only.
The CHESS Only intervention included a series of complementary services to assist patients in accessing information about breast cancer and navigating the medical system. These included information services such as Questions & Answers, Instant Library, and Resource Guide. This condition also offered communication services, which enhanced both interactivity and presence of the system, such as Discussion Group and Ask an Expert. Other services provided interactive coaching, which further increased both presence and interactivity of the CHESS intervention, such as Action Plan, Health Charts, and Decision Aid. The regular reporting of patient worries, concerns, and challenges in cancer treatment was also encouraged by the CHESS system (Hawkins, Kreuter, Resnicow, Fishbein, & Dijkstra, 2008).
CHESS with Mentor.
In addition to the CHESS system, this intervention included a human Cancer Mentor. The Mentor was a National Cancer Institute cancer information specialist, who previously consulted patients through the 1–800-4CANCER Cancer Information Service. The mentor was trained to use the CHESS system so that concrete suggestions about the most effective system use could be made to patients based on their individual needs. Phone conversations with the mentor occurred 10 times with each patient during the six-month study period and lasted anywhere from five minutes to an hour (the average being around 15 minutes) (Baker et al., 2011). During conversations, the mentor answered questions, guided the selection of trustworthy information, and recommended further search strategies. The regularity and archived records of the dialogues helped the mentor to build upon past discussions so that more tailored advice could be offered to individual patients (Hawkins, Pingree et al., 2010).
Key Measures
This study examined the interplay of different e-health intervention use and depression levels on perceived healthcare competence, emotional processing, and social well-being over the 6-month intervention period. The reliability and validity of these measures have been tested in prior research (Brady et al., 1997; Cella et al., 1993; Gustafson et al., 2005; Baker et al., 2011).
Depression.
Feelings of depression, as a key independent variable of the study, were assessed on a four-point scale (0 = rarely or none, 3 = most or all the time) by using eight items of the well-established Center for Epidemiologic Studies Depression Rating Scale (CES-D) (Radloff, 1977)1. These items were combined to measure patients’ depression (pretest M = .83, SD = .62, Cronbach’s α = .86), with higher scores indicating greater depression. Then, the depression scale was divided into two levels (low and high) by using a median-split technique (Median = .63)2.
Perceived healthcare competence.
This measure assesses an individual’s level of comfort interacting with health professionals and managing different healthcare situations (see Gustafson et al., 1999, 2001, 2005). Participants were asked to indicate their level of agreement on a five-point scale (0 = strongly disagree, 4 = strongly agree) with the following statements: (1) “I went to the right healthcare provider at the right time,” (2) “I understood what was going on,” (3) “I thought about what was going to happen ahead of time,” (4) “I knew the right question to ask,” and (5) “I felt comfortable with how actively I participated in my care.” The five items were combined to create a perceived healthcare competence scale (pretest: M = 2.93, SD = .73, Cronbach’s α = .85; 3 month: M = 3.03, SD = .73, Cronbach’s α = .87; 6 month: M = 3.13, SD = .69, Cronbach’s α = .87).
Emotional processing.
For emotional processing, respondents indicated their level of agreement on a five-point scale (0=strongly disagree, 4=strongly agree) with the following statements: Since I learned I had cancer, I have (1) “Learned to see my emotions in a new way” (2) “Become less afraid of my emotions” (3) “Accepted my emotions” (4) “Seen some worth in even unpleasant emotions” (5) “Learned why my negative emotions occur” (6) “Gained some control over my negative emotions” (7) “Understood how my thoughts affect my emotions” (8) “Learned specific things to do to change my emotions” and (9) “Learned not to dwell on negative thoughts.” Items were combined (M = 2.46, SD = .57, Cronbach’s α = .85; 3 month; M = 2.56, SD = .59, Cronbach’s α = .86; 6 month: M = 2.65, SD = .65, Cronbach’s α = .92).
Social well-being.
Social well-being, as one dimension of the multi-dimensional World Health Organization Quality of Life (WHOQOL) assessment instrument, examined patients’ interpersonal relations and social interactions, including interpersonal functioning, social activities, support from significant others, family members, and friends (see Den Oudsten, Van Heck, Van der Steeg, Roukema, & De Vries, 2009; Padilla, Ferrell, Grant, & Rhiner, 1990). Using a five-point scale (0 = very dissatisfied, 4 = very satisfied), participants were asked to respond to the listed statements: (1) “How satisfied are you with yourself?” (2) “How satisfied are you with your personal relationships?” and (3) “How satisfied are you with the support you get from your friends?” These items were combined (pretest: M = 3.26, SD = .64, Cronbach’s α = .74; 3 month; M = 3.08, SD = .62, Cronbach’s α = .70; 6 month: M = 3.14, SD = .61, Cronbach’s α = .70).
Control variables.
Baseline (pretest) scores of each dependent variable (perceived healthcare competence, emotional processing, and social well-being), along with other demographic and clinical variables, were included as covariates in the subsequent analyses (e.g., Namkoong et al., 2010; Shaw, Hawkins, McTavish, Pingree, & Gustafson, 2006).
Analytical Framework
Mixed ANCOVA (Analysis of Covariance) was performed to test the proposed hypotheses and research question (Moulton, 2010). It was a 3 (intervention type: Internet Only vs. CHESS Only vs. CHESS with Mentor) x 2 (depression level: high vs. low) x 2 (use time: 3-month vs. 6-month) design and the intervention use time was a within-subject factor. Only breast cancer patients who participated at all times were included in the subsequent analyses.
Results
Patient Characteristics
As key patient demographic and clinical characteristics, age, education, minority status (yes/no), insurance (yes/no), cancer stage, surgery (yes/no), and days between diagnosis and intervention were included in the analyses. These seven demographic and clinical characteristics of breast cancer patients across three difference intervention conditions were compared at baseline; there were no significant differences. This supports that the random assignment to the conditions worked well in the experiment. See Table 1 for detailed information.
Table 1.
Demographic and clinical characteristics of intervention groups (pretest)
| Internet Only (n =112) |
CHESS Only (n =111) |
CHESS with Mentor (n =105) |
|
|---|---|---|---|
| Age | |||
| Mean (SD) | 52.25 (10.23) | 50.90 (9.00) | 52.66 (9.28) |
| Minority | |||
| Yes | 12 (10.7 %) | 11 (10 %) | 12 (11.8 %) |
| No | 100 (89.3 %) | 99 (90 %) | 90 (88.2 %) |
| Education | |||
| High school degree | 14 (12.5 %) | 17 (15.3 %) | 15 (14.3 %) |
| College degree or higher | 98 (87.5 %) | 94 (84.7 %) | 90 (85.7 %) |
| Insurance | |||
| Yes | 112 (100 %) | 110 (100 %) | 100 (99 %) |
| No | 0 (0 %) | 0 (0 %) | 1 (1 %) |
| Breast Cancer Stage | |||
| Early stage (stage 0,1,2) | 65 (59.1 %) | 65 (59.1 %) | 63 (61.8 %) |
| Late stage (3,4, or inflammatory) |
11 (10 %) | 8 (7.3 %) | 7 (6.9 %) |
| Other | 34 (30.9 %) | 37 (33.6 %) | 32 (31.4 %) |
| Surgery or Treatment | |||
| Yes | 67 (62.6 %) | 59 (54.6 %) | 55 (56.7 %) |
| No | 40 (37.4 %) | 49 (45.4 %) | 42 (43.3 %) |
|
Days btw Diagnosis and Intervention |
|||
| Mean (SD) | 68.42 (28.05) | 67.08 (24.29) | 68.72 (30.38) |
Note. There were no statistically significant differences among these variables across different intervention groups.
Effects of Intervention Type, Depression, and Time on Perceived Healthcare Competence
To investigate difference in perceived healthcare competence, ANCOVA analysis was conducted, with main effects, two-way, and three-way interactions examined. We observed main effects of depression, F(1, 253) = 10.397, p = .001, η² = .039 and intervention type, F(2, 253) = 3.063, p = .048, η² = .024. Also, there was a significant two-way interaction for intervention type by depression, F(2, 253) = 3.673, p = .027, η² = .028 and a three-way interaction for intervention type by depression by time, F(2, 253) = 3.654, p = .027, η² = .028. Table 2 shows the mixed ANCOVA models for healthcare competence by intervention type, depression, and time.
Table 2.
Mixed ANCOVA analysis results predicting healthcare competence
| Within-Subject Effect |
Mean Square |
df | F | p | η² |
|---|---|---|---|---|---|
| Time | .003 | 1 | .010 | .920 | .00 |
| Time * Healthcare competence (pretest) | .038 | 1 | .131 | .717 | .001 |
| Time * Intervention type | .011 | 2 | .039 | .962 | .00 |
| Time * Depression | .101 | 1 | .350 | .555 | .001 |
| Time * Intervention type * Depression | 1.055 | 2 | 3.654 | .027 | .028 |
| Error (time) | .289 | 253 | |||
| Between-Subject Effect |
Mean Square |
df | F | p | η² |
| Intercept | 108.916 | 1 | 221.006 | .000 | .466 |
| Healthcare competence (pretest) | 48.404 | 1 | 98.218 | .000 | .280 |
| Intervention type | 1.510 | 2 | 3.063 | .048 | .024 |
| Depression | 5.124 | 1 | 10.397 | .001 | .039 |
| Intervention type * Depression | 1.810 | 2 | 3.673 | .027 | .028 |
| Error | .493 | 253 | |||
The data revealed that patients with high depression had lower levels of perceived healthcare competence than patients with low depression, regardless of intervention assignment and time. Also, the post hoc mean and standard error comparisons showed that overall, patients who used the CHESS with Mentor intervention (M = 3.15, SE = .05) had higher levels of perceived healthcare competence than those who used the Internet Only (M = 2.97, SE = .05, p = .02) condition. Moreover, patients with high depression benefited significantly more from both CHESS Only (M = 3.00, SE = .07, p = .032) and CHESS with Mentor (M = 3.15, SE = .07, p = .001) interventions compared to the Internet Only (M = 2.77, SE = .08) control condition. Interestingly, in contrast to the Internet Only (M = 2.72, SE = .097) group, more depressed breast cancer patients demonstrated the most enhanced healthcare competence in the CHESS with Mentor intervention (M = 3.25, SE = .087, p = .000) at the 6-month intervention period. Patients with high depression also had better healthcare competence in the CHESS Only intervention (M = 3.12, SE = .087, p = .003) than the control (M = 2.72, SE = .097) at 6 months, but the benefits were not as pronounced as for the CHESS with Mentor condition. Within the CHESS Only intervention, however, more depressed patients improved their perceived healthcare competence from 3 months (M = 2.89, SE = .097) to 6 months (M = 3.12, SE = .087) and the magnitude of the improvement was statistically significant at p = .044. Figure 1 provides a visual representation of these findings.
Figure 1.
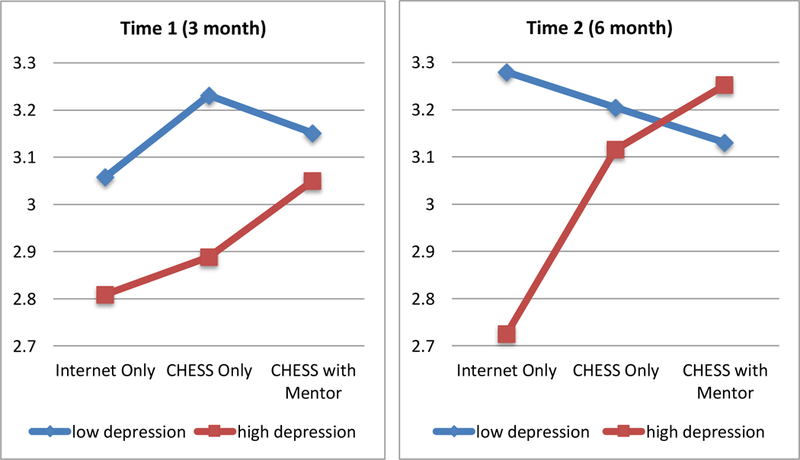
Interaction effects of intervention type, depression, and time on healthcare competence
Effects of Intervention Type, Depression, and Time on Emotional Processing
For emotional processing, there were significant main effects of depression, F(1, 249) = 6.3, p = .013, η2 = .025 and intervention type, F(2, 249) = 3.186, p = .043, η2 = .025. Also, there were significant two-way interaction effects for intervention type by depression, F(2, 249) = 3.237, p = .041, η2 = .025. Table 3 presents results from the mixed ANCOVA models for emotional processing by intervention type, depression, and time.
Table 3.
Mixed ANCOVA analysis results predicting emotional processing
| Within-Subject Effect |
Mean Square |
df | F | p | η² |
|---|---|---|---|---|---|
| Time | .015 | 1 | .074 | .786 | .00 |
| Time * Emotional processing (pretest) | .015 | 1 | .071 | .789 | .00 |
| Time * Intervention type | .047 | 2 | .232 | .793 | .002 |
| Time * Depression | .223 | 1 | 1.096 | .296 | .004 |
| Time * Intervention type * Depression | .084 | 2 | .412 | .663 | .003 |
| Error (time) | .204 | 249 | |||
| Between-Subject Effect |
Mean Square |
df | F | p | η² |
| Intercept | 39.826 | 1 | 107.921 | .000 | .302 |
| Emotional processing (pretest) | 43.819 | 1 | 118.741 | .000 | .323 |
| Intervention type | 1.176 | 2 | 3.186 | .043 | .025 |
| Depression | 2.325 | 1 | 6.300 | .013 | .025 |
| Intervention type * Depression | 1.194 | 2 | 3.237 | .041 | .025 |
| Error | .369 | 249 | |||
In general, patients with higher scores on the measure of depression (M = 2.68, SE = .039) tended to have higher emotional processing than patients with lower scores on the depression measure (M = 2.55, SE = .038) at p = .013, regardless of intervention assignment and time. As for the intervention type, patients who were randomly assigned to the CHESS with Mentor intervention (M = 2.69, SE = .047) had better emotional processing than those who used the Internet Only (M = 2.53, SE = .047, p = .013) condition. More depressed cancer patients reported better emotional processing in the CHESS with Mentor condition as opposed to the Internet Only control, and this pattern was consistent across two different time points. See Figure 2 for details.
Figure 2.
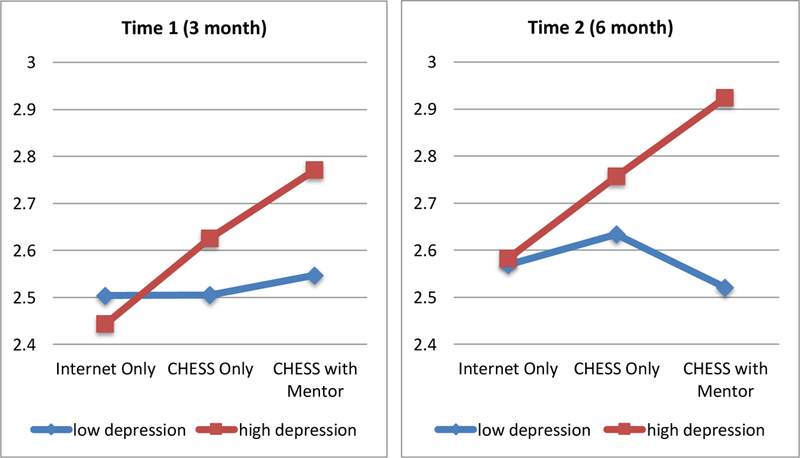
Interaction effects of intervention type and depression on emotional processing
Effects of Intervention Type, Depression, and Time on Social Well-Being
For social well-being, there were neither significant main effects of any of the predictors nor two-way interaction effects. Instead, there were significant three-way interactions for intervention type by depression by time, F(2, 251) = 3.617, p = .028, η² = .028. In other words, at 6 months, more depressed breast cancer patients showed greatly improved social well-being in the CHESS with Mentor intervention (M = 3.18, SE = .080, p = .018) and also in the CHESS Only condition (M = 3.15, SE = .08, p = .041) in contrast with the Internet Only control condition (M = 2.90, SE = .092). Additionally, in the Internet Only condition, breast cancer patients with lower levels of depression showed enhanced social well-being from 3 month (M = 3.04, SE = .076) to 6 month (M = 3.23, SE = .077) at p = .026 surveys. Table 4 presents the mixed ANCOVA models of social well-being by intervention type, depression, and time. These differences are plotted in Figure 3.
Table 4.
Mixed ANCOVA analysis results predicting social well-being
| Within-Subject Effect |
Mean Square |
df | F | p | η² |
|---|---|---|---|---|---|
| Time | .346 | 1 | 1.926 | .166 | .008 |
| Time * Social well-being (pretest) | .230 | 1 | 1.277 | .260 | .005 |
| Time * Intervention type | .037 | 2 | .208 | .812 | .002 |
| Time * Depression | .084 | 1 | .469 | .494 | .002 |
| Time * Intervention type * Depression | .650 | 2 | 3.617 | .028 | .028 |
| Error (time) | .180 | 251 | |||
| Between-Subject Effect |
Mean Square |
df | F | p | η² |
| Intercept | 46.798 | 1 | 121.450 | .000 | .326 |
| Social well-being (pretest) | 37.251 | 1 | 96.673 | .000 | .278 |
| Intervention type | .456 | 2 | 1.183 | .308 | .009 |
| Depression | 1.045 | 1 | 2.711 | .101 | .011 |
| Intervention type * Depression | .141 | 2 | .366 | .694 | .003 |
| Error | .385 | 251 | |||
Figure 3.
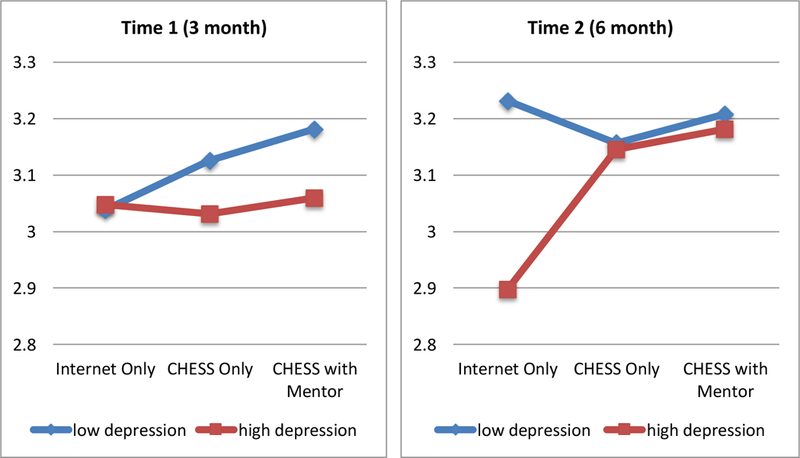
Interaction effects of intervention type, depression, and time on social well-being
Discussion
The primary purpose of this study was to investigate how levels of depression interacted with different types of e-health intervention used to improve breast cancer patients’ psychosocial health. As for patient health outcomes, perceived healthcare competence, emotional processing and social well-being were examined to understand cognitive, emotional, and social dimensions of patient health conditions. Specifically, CHESS Only and CHESS with Mentor interventions were compared to the Internet Only control. The longitudinal nature of the data allowed us to investigate shorter- and longer-term intervention effects on cancer patients over a 6-month period. This was done to provide a better understanding of the e-health intervention effects in the course of cancer patients’ treatment process. That is, the study attempted to find out when and with what type of e-health intervention, psychosocial health benefits of breast cancer patients could be maximized with a focus on understanding the moderating role of depression.
Consistent with previous research (Spiegel, 1997; Visser & Smets, 1998), the study found main effects of depression on perceived healthcare competence and emotional processing of breast cancer patients. Specifically, more depressed breast cancer patients reported lower levels of perceived healthcare competence than those with low levels of depression, no matter what e-health intervention they were exposed to. Since cancer patients with pre-existing feelings of depression are more vulnerable than cancer patients who are less depressed, these findings make sense: depression level of cancer patients is negatively associated with their abilities to manage healthcare and communicate with healthcare providers about symptoms and treatment options. As for emotional processing, the opposite pattern was observed, such that more depressed cancer patients seemed to have deeper levels of emotional processing than those who were less depressed. This was the opposite of what was hypothesized. Further investigation is need to understand other factors that could account for this relationship.
Regarding the main effects of intervention type, the CHESS with Mentor intervention was the most effective e-health intervention for both perceived healthcare competence and emotional processing of breast cancer patients, regardless of depression levels. Confirming previous study findings, the synergistic effects produced by the combination of computer-mediated and live interpersonal support was most effective for helping patients gain confidence in their healthcare and emotional distress management (Hawkins, Han et al., 2010; Hawkins et al., 2011).
Moreover, the two-way interactions between intervention type and depression showed that overall, more depressed cancer patients benefited most from the CHESS with Mentor intervention compared to other interventions. This pattern was consistent regardless of time points and was true for both perceived healthcare competence and emotional processing. In addition, the positive CHESS with Mentor system effects were larger than the positive effects of the CHESS Only intervention, suggesting that higher levels of presence and interactivity were associated with improved health outcomes as hypothesized. These findings were consistent with previous study results that the CHESS with Mentor intervention improved multiple psychosocial health outcomes (e.g., cancer information competence, emotional processing, and social support) than did the Internet Only control (Baker et al., 2011; Hawkins, Han et al., 2010). There were, however, no significant two-way interactions found for social well-being of the patients.
The most interesting findings of the study were three-way interactions among intervention type, depression, and time on perceived healthcare competence and social well-being of breast cancer patients. For both health outcomes, more depressed breast cancer patients showed the most improvement when they used the CHESS with Mentor intervention from baseline through six months. Combining an interactive e-health services with interpersonal support from the cancer Mentor gave more depressed patients the confidence to actively engaging in their healthcare and discussing cancer progression with doctors. Moreover, the same intervention boosted the patients’ satisfaction with social support they received from their family and friends as compared to other e-health intervention (Hawkins, Han et al., 2010; Lee, 2004; Walther et al., 2005). The depressed patients’ level of satisfaction from interpersonal support was greater from baseline to 3-months and to 6-months intervention. These findings were consistent with previous research that the CHESS with Mentor intervention, compared to CHESS Only, produced better cancer information competence at six weeks, higher functional well-being at both six weeks and three months, and reduced breast cancer-related concerns at three months of the e-health intervention period (Baker et al., 2011). This study speaks to the sustainability and continuity of the benefits these sorts of e-health systems can offer to patients with breast cancer.
Although this study produced meaningful findings, it is not without limitations. First, the study did not investigate which specific services within CHESS Only or CHESS with Mentor intervention were most influential for breast cancer patients to improve their psychosocial outcomes: as mentioned in the methods section, the CHESS system includes Information Services, Support Services, and Coaching Services. The focus of the study, however, was not to understand which sub-services of the CHESS Only or CHESS with Mentor intervention were more influential than others but to understand how CHESS as an ICCS as a whole when coupled with a human Mentor worked to help cancer patients with improved coping and well-being.
Second, although the interactive relationship between depression and the e-health intervention use explains a substantial amount of variance in the examined health outcomes of breast cancer patients during at the six-month follow-up survey, there could be other factors that may have an influence on those psychosocial outcomes such as physical fatigue (Visser & Smets, 1998). Nonetheless, by finding patterns of interactive relationships of intervention type, depression, and time, with a sample of breast cancer patients, this experimental study adds valuable insights to the current health communication literature.
Consequently, this study offers several important implications for e-health intervention designers, healthcare professionals, and scholars in the area of health communication. It seems that the CHESS with Mentor intervention has the greatest potential for assisting emotionally and mentally vulnerable cancer patients for a longer period of time. This study consistently found strong beneficial effects of this intervention on cognitive, emotional, and social dimensions of depressed patients’ health outcomes. Depression is prevalent among cancer patients. The study findings, therefore, can provide insights on how to develop or improve an e-health intervention for cancer patients with higher depression levels. Incorporating interpersonal Mentor support to the e-health intervention produced desirable synergistic effects and could be key for the well-being and confidence of breast cancer patients dealing with depression. Although NCI’s Cancer Information Service has offered similar services, it rarely provides follow-up on previous calls and also does not offer information or support that builds upon or complements resources from a more comprehensive and integrated ICCS such as CHESS. In contrast, the CHESS with Mentor intervention was facilitated by the Mentor’s familiarity of the CHESS services (Baker et al., 2011).
Some previous findings also support these results, arguing that interpersonal contributors are essential to manage depression (Joiner, 2000) and can buffer depressive feelings (Badger et al., 1999; Segrin, 2001). Since not much research to date has examined the effects of different e-health interventions with varying degrees of interactivity and presence, this investigation also contributes to these areas of inquiry. Future research could compare beneficial effects of interpersonal therapy for depressed cancer patients to the effects of a system like CHESS with Mentor for health outcomes. If an e-health system like CHESS with Mentor could provide similar effects as a psychologist for a significantly lower cost, it might influence how healthcare professionals approach offering services to their patients. These results also speak to the importance of human interaction within the context of e-health support systems.
By systematically investigating interactive relationships of intervention type, depression levels, and time, for the 6-month intervention period, this study contributes to narrowing down when, and to what degree, such intervention effects started, accumulated, and become sizable enough to enhance cognitive, emotional, and social outcomes of breast cancer patients. Since effects of the intervention use became more beneficial to depressed cancer patients at later points in time, we argue that it would be a good strategy to provide health services through online and through interpersonal Mentor support for longer than three months to effectively assist more depressed breast cancer patients. Future research and clinical practice should consider this intervention strategy. These findings, then, have theoretical implications on how mental health factors can intersect with interactivity and presence to influence psychosocial outcomes, conceptual implications for the role of human interaction within e-health systems, and practical implications for the development of e-health interventions for cancer patients.
Acknowledgements
We would like to thank the women who agreed to participate in the study. This study was funded by grants from the National Cancer Institute (P50 CA095817–05).
Footnotes
Detailed information about measures is available from the corresponding author.
Anything above a low value was considered experiencing ‘some depression’ from patients. Considering potential social desirability biases, we were mainly interested in comparing low and high depression cancer patients – not with absolute values.
Contributor Information
Sojung Claire Kim, Department of Communication George Mason University
Bret Shaw, Department of Life Sciences Communication University of Wisconsin-Madison
Dhavan V. Shah, School of Journalism and Mass Communication Center for Health Enhancement Systems Studies University of Wisconsin-Madison
Robert P. Hawkins, School of Journalism and Mass Communication Center for Health Enhancement Systems Studies University of Wisconsin-Madison
Suzanne Pingree, Department of Life Sciences Communication University of Wisconsin-Madison
Fiona M. McTavish, Center for Health Enhancement Systems Studies University of Wisconsin-Madison
David H. Gustafson, Department of Industrial and Systems Engineering Center for Health Enhancement Systems Studies University of Wisconsin-Madison
References
- American Cancer Society (May 2017). What are the key statistics about breast cancer? Retrieved July 20, 2017, from http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-key-statistics
- Anderson BL (1992). Psychological interventions for cancer patients to enhance quality of life. Journal of Consulting and Clinical Psychology, 60, 552–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badger TA, Braden CJ, Longman AJ, & Mishel MH (1999). Depression burden, self-help interventions, and social support among women receiving treatment for breast cancer. Journal of Psychosocial Oncology, 17, 17–35. [Google Scholar]
- Badger TA, Braden CJ, Mishel MH, & Longman A (2004). Depression burden, psychological adjustment, and quality of life in women with breast cancer: Patterns over time. Research in Nursing & Health, 27, 19–28. [DOI] [PubMed] [Google Scholar]
- Baker TB, Hawkins R, Pingree S, Roberts LJ, McDowell HE, Shaw BR, … & Stewart JA. (2011). Optimizing ehealth breast cancer interventions: Which types of ehealth services are effective? Translational Behavioral Medicine, 1, 134–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, & Shiomoto G. (1997). Reliability and validity of the functional assessment of cancer therapy-breast quality-of-life instrument. Journal of Clinical Oncology, 15, 974–986. [DOI] [PubMed] [Google Scholar]
- Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, & Brannon J. (1993). The functional assessment of cancer therapy scale: Development and validation of the general measure. Journal of Clinical Oncology, 11, 570–579. [DOI] [PubMed] [Google Scholar]
- Den Oudsten BL, Van Heck GL, Van der Steeg AF, Roukema JA, & De Vries J (2009). The WHOQOL-100 has good psychometric properties in breast cancer patients. Journal of Clinical Epidemiology, 62, 195–205. [DOI] [PubMed] [Google Scholar]
- Dow KH, Ferrell BR, Leigh S, Ly J, & Gulasekaram P (1996). An evaluation of the quality of life among long-term survivors of breast cancer. Breast Cancer Research & Treatment, 39, 261–273. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56, 218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox S, & Purcell K (March, 2010). Health information Retrieved February 24, 2017, from http://www.pewinternet.org/2010/03/24/health-information/
- Gustafson DH, Hawkins R, Boberg E, Pingree S, Serlin RE, Graziano F, & Chan CL (1999). Impact of a patient-centered, computer-based health information support system. American Journal of Preventive Medicine, 16, 1–9. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, Hawkins R, McTavish F, Pingree S, Chen WC, Volrathongchai K, & Serlin RC. (2008). Internet-based interactive support for cancer patients: Are integrated systems better? Journal of Communication, 58, 238–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, Hawkins R, Pingree S, McTavish F, Arora NK, Mendenhall J, & Salner A. (2001). Effects of computer support on younger women with breast cancer. Journal of General Internal Medicine, 16, 435–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Stengle W, Ballard D, Hawkins R, Shaw BR, & Volrathongchai K. (2005). Use and impact of e-health System by low-income women with breast cancer. Journal of Health Communication, 10, 195–218. [DOI] [PubMed] [Google Scholar]
- Han JY, Hawkins RP, Shaw B, Pingree S, McTavish F, & Gustafson DH (2009). Unraveling uses and effects of an Interactive Health Communication System. Journal of Broadcasting and Electronic Media, 53, 112–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KA (1998). The informational needs of patients with cancer and their families. Cancer Practice, 6, 39–46. [DOI] [PubMed] [Google Scholar]
- Hawkins RP, Han JY, Pingree S, Shaw B, Baker TB, & Roberts LJ (2010). Interactivity and presence of three e-health interventions. Computers in Human Behavior, 26, 1081–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins RP, Kreuter M, Resnicow K, Fishbein M, & Dijkstra A (2008). Understanding tailoring in communicating about health. Health Education Research, 23, 454–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins RP, Pingree S, Baker TB, Roberts LJ, Shaw BR, McDowell H, & Stewart JA. (2011). Integrating eHealth with human services for breast cancer patients. Translational Behavioral Medicine, 1, 146–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins RP, Pingree S, Shaw B, Serlin RC, Swoboda C, Han JY, & Salner A. (2010). Mediating process of two communication interventions for breast cancer patients. Patient Education and Counseling, 81S, 48–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzberg AD, Robinson ME, Geisser ME, & Gremillion HA (1996). The effects of depression and chronic pain on psychosocial and physical functioning. Clinical Journal of Pain, 12, 118–125. [DOI] [PubMed] [Google Scholar]
- Joiner TE (2000). Depression’s vicious scree: Self‐propagating and erosive processes in depression chronicity. Clinical Psychology: Science and Practice, 7, 203–218. [Google Scholar]
- Kim SC, Shah DV, Namkoong K, McTavish FM, & Gustafson DH (2013). Predictors of online health information seeking among women with breast cancer: The role of social support perception and emotional well-being. Journal of Computer-mediated Communication, 18, 98–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KM (2004). Presence, explicated. Communication Theory, 14, 27–50. [Google Scholar]
- Longman AJ, Braden CJ, & Mishel MM (1999). Side-effects burden, psychological adjustment and life quality in women with breast cancer: Patterns of association over time. Oncology Nursing Forum, 26, 909–915. [PubMed] [Google Scholar]
- Lu HY, Shaw BR, & Gustafson DH (2011). Online health consultation: Examining uses of an interactive cancer communication tool by low-income women with breast cancer. International Journal of Medical Informatics, 80, 518–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald MV, Passik SD, Dugan W, Rosenfeld B, Theobald DE, & Edgerton S. (1999). Nurses’ recognition of depression in their patients with cancer. Oncology Nursing Forum, 26, 593–599. [PubMed] [Google Scholar]
- Moulton ST (2010). Analysis of Covariance (ANCOVA) Retrieved April 24, 2017, from http://isites.harvard.edu/fs/docs/icb.topic820610.files/printer-hostile%20format/Lecture22_ANCOVA.pdf
- Namkoong K, Shah DV, Han JY, Kim SC, Yoo W, Fan D, & Gustafson DH. (2010). Expression and reception of treatment information in breast cancer support groups: How health self-efficacy moderates effects on emotional well-being. Patient Education and Counseling, 8, S41–S47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newport DJ, & Nemeroff CB (1998). Assessment and treatment of depression in the cancer patient. Journal of Psychosomatic Research, 45, 215–237. [DOI] [PubMed] [Google Scholar]
- Padilla GV, Ferrell B, Grant MM, & Rhiner M (1990). Defining the content domain of quality of life for cancer patients with pain. Cancer Nursing, 13, 108–115. [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychology Measurement, 1, 385–401. [Google Scholar]
- Ryan RM, & Deci EL (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American psychologist, 55, 68–78. doi.org/10.1037/0003-066X.55.1.68 [DOI] [PubMed] [Google Scholar]
- Satin JR, Linden W, & Phillips MJ (2009). Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer, 115, 5349–61. [DOI] [PubMed] [Google Scholar]
- Saul AN, Oberyszyn TM, Daugherty C, Kusewitt D, Jones S, Jewell S, & Dhabhar FS. (2005). Chronic stress and susceptibility to skin cancer. Journal of National Cancer Institute, 97, 1760–1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segrin C (2001). Interpersonal processes in psychological problems New York: Guildford. [Google Scholar]
- Shaw B, Han JY, Hawkins RP, McTavish F, & Gustafson DH (2008). Communicating about self and others within an online support group for women with breast cancer and subsequent outcomes. Journal of Health Psychology, 13, 930–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw B, Han JY, Hawkins RP, Stewart J, McTavish F, & Gustafson D (2007). Doctor-patient relationship as motivation and outcome: Examining uses of an interactive cancer communication system. International Journal of Medical Informatics, 76, 274–282. [DOI] [PubMed] [Google Scholar]
- Shaw B, Hawkins RP, McTavish F, Pingree S, & Gustafson DH (2006). Effects of insightful disclosure within computer mediated support groups on women with breast cancer. Health Communication, 19, 133–142. [DOI] [PubMed] [Google Scholar]
- Sheldon K, Williams G, & Joiner T (2003). Self-determination theory in the clinic: Motivating physical and mental health New Haven, CT: Yale University Press. [Google Scholar]
- Spiegel D (1997). Psychosocial aspects of breast cancer treatment. Seminars in Oncology, 24, 36–47. [PubMed] [Google Scholar]
- Spiegel D, & Giese-Davis J (2003). Depression and cancer: mechanisms and disease progression. Biological Psychiatry, 54, 269–282. [DOI] [PubMed] [Google Scholar]
- Visser MRM, & Smets EMA (1998). Fatigue, depression and quality of life in cancer patients: How are they related? Supportive Care in Cancer, 6, 101–108. [DOI] [PubMed] [Google Scholar]
- Walther JB, Pingree S, Hawkins RP, & Buller DB (2005). Attributes of online interactive online health information systems. Journal of Medical Internet Research, 7(3), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]


