Abstract
Context:
Recent studies indicated that significant proportion of facial fractures attributed to road traffic mishaps in the middle- and low-income countries are caused by motorcycle (MC) crashes. However, there is limited information on crash characteristics of such injuries. This study was designed to examine the crash characteristics, pattern of fracture, and sociodemographics of patients with facial bone fractures due to MC crashes in our institution.
Subjects and Methods:
Data on patients’ sociodemographics, pattern of presentation, type(s) of fracture, patient status, crash characteristics, level of consciousness, and treatment offered were collected and analyzed.
Results:
A total of 151 patients, aged 7–59 years were reviewed during the study period. A male preponderance was observed (M:F = 4:1) and the patients were predominantly motorcyclists (64.8%, n = 98). The most common mechanism of crash was collision with another MC (51.6%, n = 78). A total of 194 fractures were reviewed and the mandible (58.8%, n = 114) was more commonly affected than the midface (41.2%, n = 80). The predominant site on the mandible was the body (31.6%) while zygoma (32.5%) was the most affected part of the midface. Patient status was found to have a statistically significant relationship with loss of consciousness (P = 0.02). Eighty-two fracture sites (42.3%) were managed with open reduction and internal fixation.
Conclusions:
Facial bone fractures occur in a significant proportion of MC crashes and riders are predominantly affected. In addition, a larger proportion of commuters rarely wear crash helmet which could have offered protection. Continual advocacy on preventive measures and enforcement of road safety regulations is hereby advised.
KEYWORDS: Facial bone, fractures, motorcycle
INTRODUCTION
It has been documented that injuries will likely become the fourth leading cause of mortality and disability worldwide by 2030.[1] Low- and middle-income countries are said to be disproportionately affected, accounting for a significant proportion of the overall injury-related mortality.[1,2,3,4] Most of these deaths are attributable to road traffic crashes (RTC) involving the vulnerable road users.[5,6,7,8] Facial bone fracture constitutes a substantial proportion of trauma globally, and it often results in serious morbidity and sometimes fatal consequence.[3,9,10] These injuries pose a huge economic burden due to treatment costs, rehabilitation, disabilities, and man-hour loss occasioned by hospital stay.[3,7]
In developing countries, maxillofacial injuries due to RTC continue to rise alarmingly and motorcycle (MC) crash victims form a high proportion of those killed or injured in road mishaps.[11,12,13,14,15,16] The high incidence of oral and maxillofacial injuries has been attributed to the heavy reliance on MC as a mode of transportation in the low- and middle-income countries.[2,7,11,14,15,17]
There is dearth of information on crash characteristics, epidemiology, and sociodemographics of victims of MC-related facial fractures in Nigeria and other countries in Sub-Saharan Africa. Thus, the present study was designed to examine the relationship between crash characteristics, pattern of fractures, and sociodemographics of patients with facial bone fracture due to MC crashes in our institution.
SUBJECTS AND METHODS
The data of patients who sustained facial bone fractures due to MC crash between January 2010 and December 2014 were collected on individual proforma. The patients presented either through the accident and emergency ward or maxillofacial surgery clinic of our institution.
The information gathered included patient's sociodemographics (age, sex, and occupation), crash characteristics (type and nature of crash), pattern of fracture, radiologic diagnosis and treatment offered. Patient's status (rider, pillion passenger, pedestrian) and the number of persons on the MC at the time of crash were also documented. Level of consciousness was determined using Glasgow Coma Scale.
Diagnosis of maxillofacial fractures was achieved through clinical and radiologic evaluation. All patients had plain radiographs for radiologic evaluation. In addition, computerized tomography scan was done for those who could afford it.
Ethical approval for the study was obtained from our institution's ethical review board.
Data obtained were summarized in figures and frequency tables. Analysis was done using SPSS (Statistical Package for Social Sciences, Chicago, Illinois) version 20. Descriptive statistics and Chi-square test were carried out and the level of significance was set as P < 0.05.
RESULTS
One hundred and fifty-one patients with MC-related facial fractures presented during the study period. There was a male preponderance of 120 to 31 (M: F 4:1). The mean age of the patients was 23.52 ± 9.61, while the peak age range was 20–29 years [Figure 1]. A greater proportion of injured patients were MC riders (64.8%, n = 98). Furthermore, most of the victims (56.3%, n = 85) in this series were unemployed youths [Figure 2].
Figure 1.
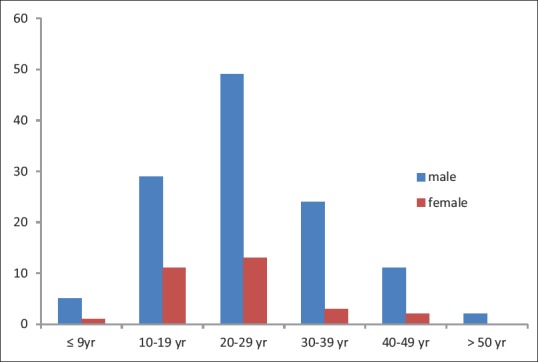
Patients’ age and sex distribution. The figure showed the age and sex distribution of the patients. There were more males than females (male n = 120, 79.5% female n = 31, 20.5%). The predominant age group were those between 20 and 29 years in both sex categories (male 40.8%, female 41.9%). The least represented age group were those above 50 years (male 0.02%, female 0%)
Figure 2.
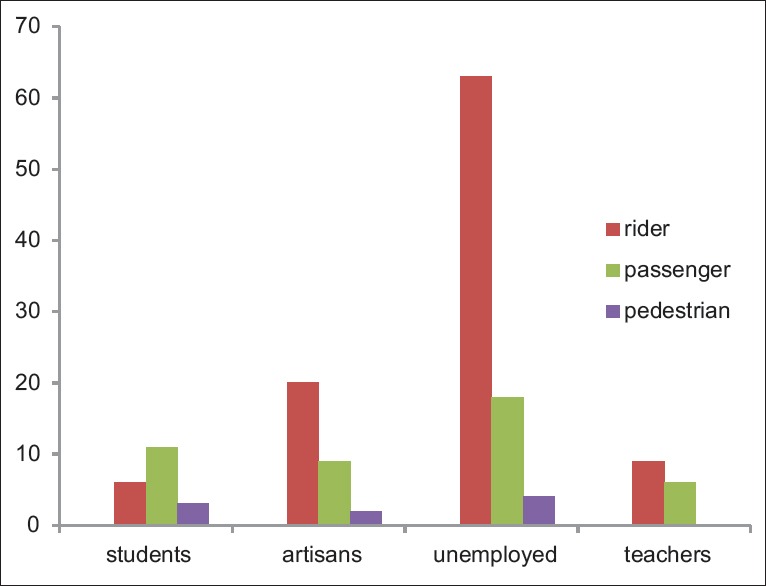
Status and occupation of crash victims. The charts showed that majority (n = 85, 56.29%) of the patients were unemployed. Artisans (n = 31) and students (n = 20) made up 20.5% and 13.3% of the patients, respectively. Furthermore, majority of those affected are motorcycle riders (n = 98, 64.9%) followed by pillion passengers (n = 44, 29.1%)
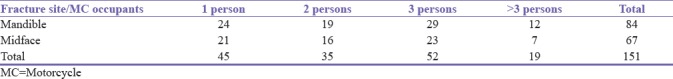
The most common mechanism of injury was collision with another MC (51.6% n = 78). Collision with motor vehicle and other objects accounted for 17.8% and 24.5%, respectively [Table 1]. Pedestrian injury accounted for just 6.0% (n = 9) of the study population. Only 17.2% (n = 26) of the victims claimed to have crash helmet on their head at the time of crash. Further examination of the crash characteristics revealed that nearly half (47.0%, n = 71) of the patients claimed that the MC was carrying 3 or more persons at the time of crash [Table 2]. However, the number of persons on the MC does not have a statistically significant relationship with fracture pattern (χ2 = 0.24, P = 0.8).
Table 1.
Mechanism of collision and status of injured patients
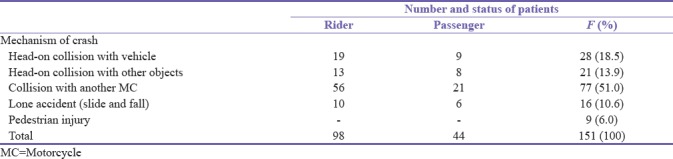
Table 2.
Number of persons on motorcycle at time of crash and site of fracture
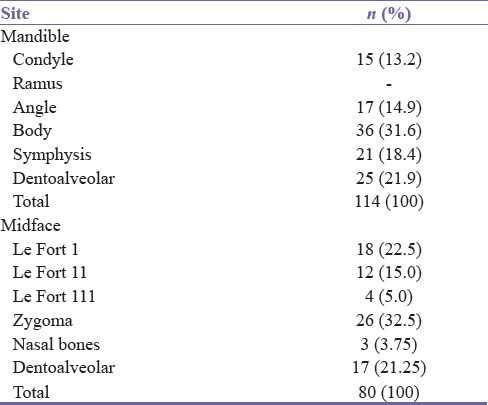
One hundred and ninety-four fracture sites were reviewed giving an average of 1.3 fractures per patient. The most commonly encountered sites of fracture were in the mandible (58.8%, n = 114) compared to the midface (41.2%, n = 80). Table 3 showed that the predominant site on the mandible was the body (31.6%) followed by the dentoalveolar region (21.9%) while zygoma (32.5%) was the most affected part of the midface followed by Le Fort 1 fractures (22.5%).
Table 3.
Pattern of maxillofacial fractures
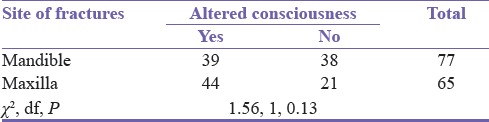
A total of 83 patients (54.9%) suffered altered state of consciousness and majority (77.1% n = 64) regained full consciousness within 24 h of admission. Further analysis revealed that patient's status (either rider or pillion passenger) was found to have a statistically significant relationship with loss of consciousness (χ2 = 12.8, P = 0.02) [Table 4]. On the contrary, fracture site, either mandible or midface did not have any significant relationship on altered consciousness (χ2 = 1.56, P = 0.13) [Table 5].
Table 4.
Relationship between altered state of consciousness and status of injured patients
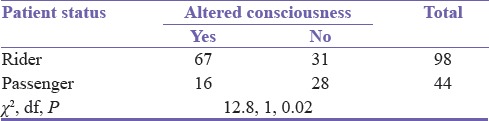
Table 5.
Relationship between altered state of consciousness and site of fracture
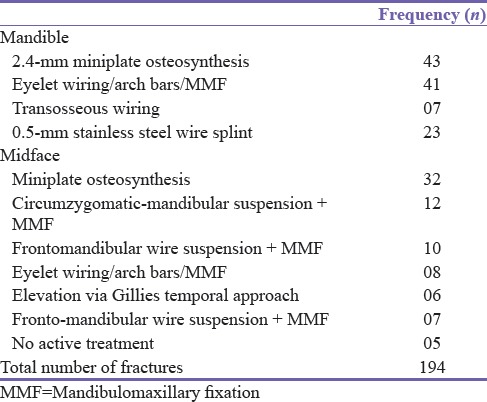
A higher proportion of the patients (57.7%, n = 112) were treated conservatively with either mandibulomaxillary fixation (MMF), a combination of MMF with internal wire suspension or 0.5-mm stainless steel wire splint without MMF [Table 6]. Eighty-two patients (42.3%) had open reduction and internal fixation which was achieved predominantly with miniplate osteosynthesis (n = 75).
Table 6.
Treatment offered to victims of motorcycle-related crash
DISCUSSION
The poor state of roads, harsh economic condition, lack of efficient public transport system, and rising spate of youth unemployment have popularized the use of MC for road transport in Sub-Saharan Africa.[2,3,7,18] Although previous studies from Nigeria have reported the pattern of facial injuries sustained by MC crash victims,[4,15,16,18] none has been able to relate the crash characteristics to the pattern of injuries and status of patients involved in such crashes. Thus, a holistic appraisal and characterization of MC-related injuries is necessary to develop strategy on prevention and enforce adherence to road traffic safety regulations.
In agreement with similar studies, we found a high male preponderance and the victims were predominantly below 30 years of age.[4,7,11,16,19,20,21] It has been argued that the male gender tends to be more adventurous and likely to indulge in injury prone adventures such as dangerous driving and use of automobile for commercial purposes. Furthermore, majority of the patients in this research were mostly unemployed youths. This view was also shared by some Nigerian authors[3,4,14,16] and other countries in Sub-Saharan Africa.[2,7] Rising youth unemployment, rural/urban migration, and attendant economic hardship have spurred many youths into riding MCs for commercial purpose in Nigeria.[3,14,22] These MCs are often procured with ease through hired purchase or differed payment system.
In this study, we found that majority of the crashes were due to collision with another MC (51.0%) followed by collision with motor vehicles (18.5%). This is comparable with the findings of Chichom-Mefire et al.[2] and Oginni et al.[4] who reported that collision with other automobiles represented 60% and 58% of all crashes, respectively. The high rate of collision involving MC and motor vehicles in this study corroborates the vulnerability of MC to other motorized road users. Moreover, MC riders are always impatient and often do not obey traffic signs and regulations. Furthermore, most Nigerian roads are designed for motor vehicle use without designated bands for MC, thus the MC shares the available portion with vehicles, thereby predisposing the road users to crash. The classical skid and fall of lone MC crashes were however low in this study.
Although there was a low utilization rate of helmet (17.2%) in this study, it is, however, higher than previous studies which reported poor adherence to protective measures in Sub-Saharan Africa.[2,4,16,18] This differs considerably from the high-income nations where helmet use is strict and mandatory for all MC riders and pillion passengers.[11,23,24] Studies have shown that MC helmets reduce the risk of head injury and mortality following crash, although these effects may be modified by other crash factors such as speed.[11,17,23,24,25] While the health benefits of crash helmets have been widely reported by various researchers,[11,21,23,24,25,26,27] its use has not been embraced in Nigeria despite preexisting legislation.
The effect of the number of pillion passengers on crash characteristics has not been examined sufficiently by previous reports because it is often assumed that MCs do not carry more than one passenger. Majority of the MCs involved in this series had more than one pillion passenger at the time of crash. This is similar to reports by Chichom-Mefire et al.[2] but contrary to the finding of Oginni et al.[16] Multiple pillion passengers increase the weight carried by the MC beyond its capacity, rendering it less stable and prone to accidents. Although it can be argued that excess passengers reduce the motility of the automobile and hence impact of collision, thereby limiting the severity of injuries sustained in such circumstances.
The pattern of facial bone injuries revealed a higher preponderance of mandibular fractures compared to the midface. Several authors have attributed the higher prevalence of mandibular fractures to the mobility and prominence of the bone.[2,3,4,6,7,10,14] In agreement with similar reports,[3,14,16] the body of the mandible was the most commonly fractured part of the bone. Furthermore, we found that zygomatic bone was the most commonly fractured bone in the midface. This corroborated the findings of previous facial trauma surveys on the prevalence of zygomatic bone fracture.[3,6,10] The prevalence of zygomatic bone fractures may be due to the prominence of the bone in the midface and hence its proneness to fracture.
In general, the prevalence of head injuries is rarely reported in most maxillofacial surveys. Few studies have reported concomitant loss of consciousness in patients with facial bone fractures due to automobile crash.[13,28,29] The proportion of those who suffered loss of consciousness in this study is comparable to similar reports.[28,29] Furthermore, we found that a statistically significant proportion of those who had loss of consciousness were riders. MC riders are often the first person in the line of crash and they are at risk of suffering more fatalities during collision. The incidence of head injury has also been linked to the impact of collision, especially in nonhelmeted individuals.[13]
Seventy-five fractures (38.7%) were treated definitively with miniplate osteosynthesis; this showed that the use of bone plates for maxillofacial fractures in Nigeria has gained ground considerably compared with previous reports[6,14] where MMF was the mainstay of facial bone fracture management.
CONCLUSIONS
Facial bone fractures occur in a significant proportion of MC-related crashes and motorcyclists were predominantly affected. In addition, a larger proportion of commuters rarely wear crash helmet which could have offered protection. Continual advocacy on preventive measures and enforcement of road safety regulations is hereby advised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge the residents at the oral and maxillofacial surgery department and the emergency room doctors for helping in data collection.
REFERENCES
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chichom-Mefire A, Atashili J, Tsiagadigui JG, Fon-Awah C, Ngowe-Ngowe M. A prospective pilot cohort analysis of crash characteristics and pattern of injuries in riders and pillion passengers involved in motorcycle crashes in an urban area in Cameroon: Lessons for prevention. BMC Public Health. 2015;15:915. doi: 10.1186/s12889-015-2290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Obimakinde OS, Ogundipe KO, Rabiu TB, Okoje VN. Maxillofacial fractures in a budding teaching hospital: A study of pattern of presentation and care. Pan Afr Med J. 2017;26:218. doi: 10.11604/pamj.2017.26.218.11621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oginni FO, Ajike SO, Obuekwe ON, Fasola O. A prospective multicenter study of injury profile, severity and risk factors in 221 motorcycle-injured Nigerian maxillofacial patients. Traffic Inj Prev. 2009;10:70–5. doi: 10.1080/15389580802496968. [DOI] [PubMed] [Google Scholar]
- 5.Toroyan T, Peden M. How safe are the world's roads? Bull World Health Organ. 2009;87:736. doi: 10.2471/BLT.09.071829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adeyemo WL, Ladeinde AL, Ogunlewe MO, James O. Trends and characteristics of oral and maxillofacial injuries in Nigeria: A review of the literature. Head Face Med. 2005;1:7. doi: 10.1186/1746-160X-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agbor AM, Azodo CC, Ebot EB, Naidoo S. Dentofacial injuries in commercial motorcycle accidents in Cameroon: Pattern and cost implication of care. Afr Health Sci. 2014;14:77–82. doi: 10.4314/ahs.v14i1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohammad S, Firas A, Sukaina R, Ameen K. Trends in the pattern of facial fractures in different countries of the world. Int J Morphol. 2012;30:745–56. [Google Scholar]
- 9.Lee K. Global trends in maxillofacial fractures. Craniomaxillofac Trauma Reconstr. 2012;5:213–22. doi: 10.1055/s-0032-1322535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fasola AO, Lawoyin JO, Obiechina AE, Arotiba JT. Inner city maxillofacial fractures due to road traffic accidents. Dent Traumatol. 2003;19:2–5. doi: 10.1034/j.1600-9657.2003.00073.x. [DOI] [PubMed] [Google Scholar]
- 11.Usha M, Ravindran V, Soumithran CS, Ravindran Nair KS. The impact of mandatory helmet law on the outcome of maxillo facial trauma: A comparative study in Kerala. J Maxillofac Oral Surg. 2014;13:176–83. doi: 10.1007/s12663-013-0496-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Solagberu BA, Ofoegbu CK, Nasir AA, Ogundipe OK, Adekanye AO, Abdur-Rahman LO, et al. Motorcycle injuries in a developing country and the vulnerability of riders, passengers, and pedestrians. Inj Prev. 2006;12:266–8. doi: 10.1136/ip.2005.011221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramli R, Oxley J, Noor FM, Abdullah NK, Mahmood MS, Tajuddin AK, et al. Fatal injuries among motorcyclists in Klang Valley, Malaysia. J Forensic Leg Med. 2014;26:39–45. doi: 10.1016/j.jflm.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 14.Oginni FO, Oladejo T, Alake DP, Oguntoba JO, Adebayo OF. Facial bone fractures in Ile-Ife, Nigeria: An update on pattern of presentation and care. J Maxillofac Oral Surg. 2016;15:184–90. doi: 10.1007/s12663-015-0826-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fasola AO. Nigeria: 2011 Faculty Lecture, Faculty of Dentistry, College of Medicine, University of Ibadan; 2011. “Okada” and Facial Injuries: That All May Live. [Google Scholar]
- 16.Oginni FO, Ugboko VI, Ogundipe O, Adegbehingbe BO. Motorcycle-related maxillofacial injuries among Nigerian intracity road users. J Oral Maxillofac Surg. 2006;64:56–62. doi: 10.1016/j.joms.2005.09.027. [DOI] [PubMed] [Google Scholar]
- 17.Cavalcante JR, Oka SC, de Santana Santos T, Dourado E, de Oliveira E, Silva ED, Gomes AC, et al. Influence of helmet use in facial trauma and moderate traumatic brain injury victims of motorcycle accidents. J Craniofac Surg. 2012;23:982–5. doi: 10.1097/SCS.0b013e31824e5b04. [DOI] [PubMed] [Google Scholar]
- 18.Oginni FO, Ugboko VI, Adewole RA. Knowledge, attitude, and practice of Nigerian commercial motorcyclists in the use of crash helmet and other safety measures. Traffic Inj Prev. 2007;8:137–41. doi: 10.1080/15389580601058472. [DOI] [PubMed] [Google Scholar]
- 19.Júnior SM, Santos SE, Kluppel LE, Asprino L, Moreira RW, de Moraes M, et al. A comparison of motorcycle and bicycle accidents in oral and maxillofacial trauma. J Oral Maxillofac Surg. 2012;70:577–83. doi: 10.1016/j.joms.2011.03.035. [DOI] [PubMed] [Google Scholar]
- 20.Ramli R, Abdul Rahman R, Abdul Rahman N, Abdul Karim F, Krsna Rajandram R, Mohamad MS, et al. Pattern of maxillofacial injuries in motorcyclists in Malaysia. J Craniofac Surg. 2008;19:316–21. doi: 10.1097/SCS.0b013e318163f94d. [DOI] [PubMed] [Google Scholar]
- 21.Christian JM, Thomas RF, Scarbecz M. The incidence and pattern of maxillofacial injuries in helmeted versus non-helmeted motorcycle accident patients. J Oral Maxillofac Surg. 2014;72:2503–6. doi: 10.1016/j.joms.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 22.Okafor EE. Youth unemployment and implication for stability of democracy in Nigeria. J Sustain Dev Afr. 2011;13:258–73. [Google Scholar]
- 23.Kraus JF, Peek C, Williams A. Compliance with the California motorcycle helmet use law. Am J Public Health. 1995;85:96–9. doi: 10.2105/ajph.85.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Servadei F, Begliomini C, Gardini E, Giustini M, Taggi F, Kraus J, et al. Effect of Italy's motorcycle helmet law on traumatic brain injuries. Inj Prev. 2003;9:257–60. doi: 10.1136/ip.9.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu B, Ivers R, Norton R, Blows S, Lo SK. Helmets for preventing injury in motorcycle riders. Cochrane Database Syst Rev. 2004;(2):CD004333. doi: 10.1002/14651858.CD004333.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Brandt MM, Ahrns KS, Corpron CA, Franklin GA, Wahl WL. Hospital cost is reduced by motorcycle helmet use. J Trauma. 2002;53:469–71. doi: 10.1097/00005373-200209000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Geneva: World Health Organization; WHO Global Status Report on Road Safety: Time for Action. Available from: http://www.who.int/violence_injury_prevention/road_safety_status/2013/en . [Google Scholar]
- 28.Zhou HH, Liu Q, Yang RT, Li Z, Li ZB. Traumatic head injuries in patients with maxillofacial fractures: A retrospective case-control study. Dent Traumatol. 2015;31:209–14. doi: 10.1111/edt.12165. [DOI] [PubMed] [Google Scholar]
- 29.Zandi M, Seyed Hoseini SR. The relationship between head injury and facial trauma: A case-control study. Oral Maxillofac Surg. 2013;17:201–7. doi: 10.1007/s10006-012-0368-z. [DOI] [PubMed] [Google Scholar]


