Abstract
Despite growing popularity of endovascular techniques, certain subsets of patients with cerebrovascular compromise may benefit from bypass surgery. We present four cases in which pending ischemic lesion was prevented by (1) A3 resection and reanastomosis following falx meningioma removal, (2) rescue superficial temporal artery–middle cerebral artery (STA-MCA) bypass after pituitary adenoma surgery, (3) STA-MCA bypass for chronic internal carotid artery occlusion, and (4) external carotid artery-MCA bypass using radial artery grafting. Following the procedure, there were no further clinical or radiological deteriorations and long-term patency was confirmed in all four cases.
Keywords: Bypass surgery, cerebrovascular occlusion, giant aneurysm, intracranial tumor
Background
Extracranial–intracranial (EC-IC) bypass is used to treat chronic stenooclusive cerebrovascular diseases (flow augmentation) and as a part of the treatment of complex aneurysms and skull base tumors (flow replacement).[1] Despite five decades of clinical use, there is still a lack of consensus regarding indications and techniques of EC-IC bypass surgery.
Today, the procedure has an invaluable role in selected patients with cerebrovascular stenooclusive disease, moyamoya disease, skull base tumors, and complex intracranial aneurysms.[2] For internal carotid artery (ICA) lesions following transsphenoidal resection of pituitary tumors, the EC-IC bypass is a life-saving treatment option.[3] In aneurysm management, bypass surgery has its role in challenging and failed endovascular treatment cases.[2] Moreover, it is a rescue treatment for symptomatic flow diverter thrombosis.[4]
We report our experience with bypass surgery in four cases with distinct underlying pathology. Approval was granted by the Institutional Review Board of the University Hospital Center Zagreb for the publication of this case series.
Case Reports
Case 1
Falx meningioma removal with compromised A3 branch resection and reanastomosis
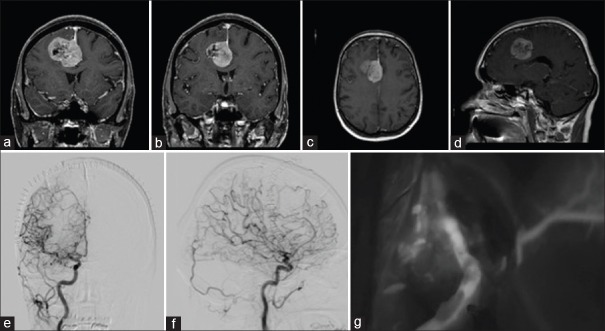
A 56-year-old woman presented with decreased visual acuity (VA). Five years earlier, she had been diagnosed with a falx meningioma, and at that time, she refused surgery. Urgent magnetic resonance imaging showed growth of the meningioma with encasement of the pericallosal-callosomarginal bifurcation [Figure 1a and b]. The tumor was nearly completely calcified and had a calcified groove, in which the callosal and callosomarginal branches were embedded [Figure 1c and d]. During tumor resection, the A3 was damaged and thereafter sutured; however, intraoperative indocyanine green fluorescent angiography (ICGA) showed the absence of distant filling. The compromised vessel was resected and the distal segment reanastomosed with the preserved segment. Adequate blood flow was confirmed intraoperatively using ICGA and 24 h after surgery using digital subtraction angiography (DSA) [Figure 1e–g]. The patient was discharged on the 7th postoperative day, neurologically intact.
Figure 1.
(a and b) Coronal T1 postcontrast images showing a right-sided falx meningioma with enhancement of pericallosal artery branches. (c) Flow void indicating arterial encasement (T1 magnetic resonance imaging horizontal view). (d) Flow void indicating arterial encasement (T1 magnetic resonance imaging sagittal view). (e and f) Digital subtraction angiography showing perfusion after reanastomosis of the pericallosal artery. (g) Intraoperative indocyanine green angiography showing anastomosis patency
Case 2
Rescue superficial temporal–middle cerebral artery bypass after pituitary adenoma surgery
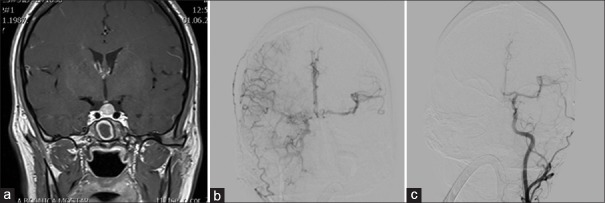
A 30-year-old woman presented with dizziness, headache, and transitory left arm weakness. Neuroradiological imaging showed a large (11 mm × 9 mm) pituitary mass, confirmed by endocrinological assessment to be a nonsecreting adenoma [Figure 2a]. The patient underwent an endoscopic transsphenoidal tumor removal, during which the left ICA was damaged. The bleeding was controlled using hemostatic material and nasal tamponade. An urgent DSA showed occlusion of the intracranial segment of the left ICA with slow filling of the ipsilateral medial cerebral artery (MCA) and anterior cerebral artery through the anterior communicating artery (ACoA) from the hypoplastic right A1 segment and delayed venous filling [Figure 2b]. Furthermore, both P1 segments were hypoplastic. Because of these angiographic findings, a rescue end-to-side STA-MCA anastomosis was performed. ICGA and micro-Doppler sonography (mDS) showed bypass patency, and the patient had no postoperative neurological sequelae. Control DSA at 10 days after surgery showed recanalization of the left ICA with satisfactory bypass flow. In addition, a pseudoaneurysmal wall of the C4 segment was noted and the patient was scheduled for endovascular treatment with stent placement. After administration of dual antiplatelet therapy, a silk flow-diverter stent (4 mm × 20 mm) was inserted with no angiographically verified complications [Figure 2c]. Twenty days after the first operation, the patient was discharged complication free.
Figure 2.
(a) Magnetic resonance imaging T1 postcontrast image showing pituitary adenoma. (b) Internal carotid artery was compressed, and there was weak collateral flow through the anterior communicating artery. (c) After the superficial temporal–middle cerebral artery bypass, there was collateral flow through the bypass
Case 3
Double-barrel superficial temporal–middle cerebral artery bypass for internal carotid artery occlusion and contralateral stenosis
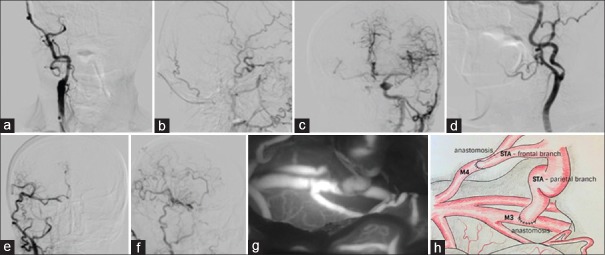
A 67-year-old male with a history of multiple transient ischemic attacks (TIAs) presented with a right MCA stroke. DSA showed complete occlusion of the right ICA in the neck, moderate (50%) contralateral ICA stenosis, and collateral flow limited only to the ophthalmic artery and poorly to the ACoA [Figure 3a–d]. Carotid endarterectomy was unsuccessful. Due to a large STA, the surgical plan was to perform a double-barrel STA-MCA bypass; in case of failure, a high-flow bypass was the alternative [Figure 3h]. After preparation of the STA branches and a wide Sylvian fissure opening, both were anastomosed terminolateral to both M3 segments. A satisfactory blood flow was confirmed intraoperatively using ICGA and mDS and at the 1st postoperative day using DSA [Figure 3e–g]. At 6 months follow-up, both anastomosed STA segments had a diameter comparable to the normal ICA, good flow, and excellent global (hemispheric) perfusion. The patient fully recovered from the stroke and experienced no further TIAs.
Figure 3.
(a) Digital subtraction angiography showing occlusion of the internal carotid artery neck. (b) Collateral flow through the ophthalmic artery. (c) Weak collateral flow through the anterior communicating artery. (d) Contralateral internal carotid artery 50% stenosis. (e) Double-barrel superficial temporal–middle cerebral artery bypass – complete revascularization of the middle cerebral artery and anterior cerebral artery territory through the graft (lateral view). (f) Double-barrel superficial temporal–middle cerebral artery bypass – complete revascularization of the middle cerebral artery and anterior cerebral artery territory through the graft (anterior view). (g) Intraoperative indocyanine green showing anastomosis patency. (h) Schematic view of the double-barrel superficial temporal–middle cerebral artery bypass procedure
Case 4
External carotid artery -RA-M3 bypass for a large supraclinoid internal carotid artery aneurysm
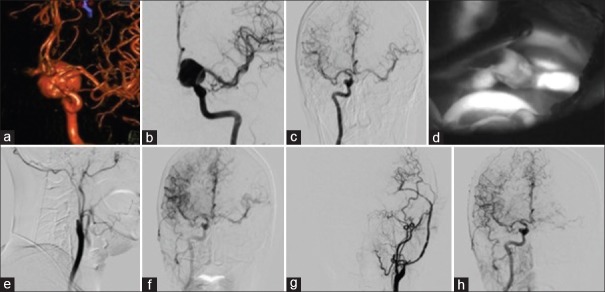
A 58-year-old woman presented with blurry vision on the left eye. Neuroradiological imaging showed a giant aneurysm of the left supraclinoid ICA and a small saccular aneurysm of the right C4 segment [Figure 4a and b]. An uneventful 30-min left ICA angiographic balloon test occlusion showed good collateral circulation through the ACoA [Figure 4c]. The surgery plan was to secure the distal flow to the MCA using a radial artery (RA) graft in order to prevent a late stroke after ICA occlusion. The left RA was harvested without consequences. A left frontotemporal osteoplastic craniotomy and Sylvian fissure dissection were performed. After exposing the left common carotid artery bifurcation, a high-flow external carotid artery-RA-M3 bypass was performed in order to ensure perfusion of the left hemisphere and reduces the pressure load on the right ICA. Next, the left C1 segment was occluded; then the A1 and M1 segments temporary were clipped, and the aneurysm and the prebifurcation ICA segment completely was occluded using three clips. ICGA and mDS showed good bypass patency and complete occlusion of the aneurysm [Figure 4d]. Postoperatively, there was improvement of VA on the left eye and no new neurological deficits. DSA performed on the 1st postoperative day showed that there was no flow through the RA graft; however, arterial pulsations were present, and there was good perfusion of the left hemisphere through the ACoA [Figure 4e and f]. Graft thrombosis was suspected and low-molecular-weight heparin therapy was started. Follow-up DSA was performed after 10 days, showing good bypass flow [Figure 4g]. Surprisingly, flow from the opposite side over the ACoA was absent [Figure 4h]. The patient was discharged 11 days postoperatively, neurologically intact.
Figure 4.
(a) Three-dimensional MSCT angiography showing a large left supraclinoid internal carotid artery aneurysm. (b) Digital subtraction angiography shows a large left supraclinoid internal carotid artery aneurysm (anterior view). (c) Balloon occlusion test showing collateral flow. (d) Intraoperative indocyanine green shows patency of the anastomosis. (e) Early postoperative digital subtraction angiography shows no flow through the radial artery graft. (f) Collateral flow persisting through the right internal carotid artery during radial artery graft vasospasm. (g) At 10 days postoperatively, digital subtraction angiography shows a normal flow through the graft with signs of vasospasm. (h) Flow through opposite side was reduced after the radial artery graft spasm recovered
Discussion
Total skull base tumor removal sometimes requires sacrificing the encased large vessels. In such cases, high-flow RA or saphenous vein (SV) grafts are mandatory.[5] Likewise, treatment of smaller skull base or interhemispheric meningiomas might require laterolateral M3 or PICA anastomoses or vascularization using the STA or occipital artery.
ICA bleeding and formation of fistulas or aneurysms are rare, but potentially fatal complications of transsphenoidal surgery that requires immediate hemostasis or stenting.[2] Early stent placement is a viable option; however, it presupposes that the vessel lumen is preserved and the patient is started on antiaggregation therapy, both of which increase the risk of rebleeding.[6] If sellar packing causes ICA occlusion or ICA occlusion is inevitable, bypass surgery is the only option to prevent ischemic complications. In the second case, an STA-MCA bypass was performed, followed by stent placement. Thus, the MCA area was supplied from both the natural vessel and artificial one, the STA bypass.
Bypass surgery is the last resort for patients with ICA occlusion in whom endovascular treatment is contraindicated.[7] Apart from the case presented herein, recently two other patients with ICA occlusion and preoperative hemiparesis underwent an STA-MCA bypass procedure at our center. All of these patients had favorable preoperative DSA findings which dictated the treatment modality and in case of failure, a high-flow bypass was considered as an alternate procedure.[8] When possible, a double-barrel STA-MCA bypass is the preferred procedure.
Despite refined endovascular techniques, complex aneurysms are very often treated surgically.[9] One possible donor vessel in large aneurysms cases with ICA occlusion is the RA, which has advantages (larger diameter) and drawbacks (vasospasm) over the SV graft. Perioperative antiplatelet therapy and eptifibatide administration reduce the risk of graft thrombosis.[10] In our experience, ICGA and mDS have proven to be essential modalities in the intraoperative armamentarium in the assessment of graft patency and distal brain perfusion.[11]
Conclusion
EC-IC bypass might offer the best options of treatment for selected cases; therefore, the indications have to be carefully studied.
Informed consent
All patients have consented to the submission of the case series to the journal.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Gazyakan E, Lee CY, Wu CT, Tsao CK, Craft R, Henry SL, et al. Indications and outcomes of prophylactic and therapeutic extracranial-to-intracranial arterial bypass for cerebral revascularization. Plast Reconstr Surg Glob Open. 2015;3:e372. doi: 10.1097/GOX.0000000000000339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vilela MD, Newell DW. Superficial temporal artery to middle cerebral artery bypass: Past, present, and future. Neurosurg Focus. 2008;24:E2. doi: 10.3171/FOC/2008/24/2/E2. [DOI] [PubMed] [Google Scholar]
- 3.Tantogtip D, Fratianni A, Jenkner J, Arnold S, Spetzger U. Surgical treatment of inadvertent internal carotid artery lesion by the extracranial high-flow bypass. A case report and review of the literature. J Neurol Surg Rep. 2015;76:100–4. doi: 10.1055/s-0035-1551670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lanterna LA, Lunghi A, Brembilla C, Gritti P, Bernucci C. Extraintracranial bypass as a rescue therapy for symptomatic flow diverter thrombosis. Case Rep Neurol Med 2015. 2015:204387. doi: 10.1155/2015/204387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalavakonda C, Sekhar LN. Cerebral revascularization in cranial base tumors. Neurosurg Clin N Am. 2001;12:557–74. viii-ix. [PubMed] [Google Scholar]
- 6.Kocer N, Kizilkilic O, Albayram S, Adaletli I, Kantarci F, Islak C, et al. Treatment of iatrogenic internal carotid artery laceration and carotid cavernous fistula with endovascular stent-graft placement. AJNR Am J Neuroradiol. 2002;23:442–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Ciric I, Ragin A, Baumgartner C, Pierce D. Complications of transsphenoidal surgery: Results of a national survey, review of the literature, and personal experience. Neurosurgery. 1997;40:225–36. doi: 10.1097/00006123-199702000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Lawton MT, Hamilton MG, Morcos JJ, Spetzler RF. Revascularisation and aneurysm surgery: Current techniques, indications and outcome. Neurosurgery. 1996;38:83–94. doi: 10.1097/00006123-199601000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Abla AA, Zaidi HA, Crowley RW, Britz GW, McDougall CG, Albuquerque FC, et al. Optic chiasm compression from mass effect and thrombus formation following unsuccessful treatment of a giant supraclinoid ICA aneurysm with the Pipeline device: Open surgical bailout with STA-MCA bypass and parent vessel occlusion. J Neurosurg Pediatr. 2014;14:31–7. doi: 10.3171/2014.4.PEDS13213. [DOI] [PubMed] [Google Scholar]
- 10.Stambolija V, Mrak G, Lozic M, Ljevak J, Miklic ublic M, Scap M, et al. Intraoperative eptifibatide administration during urgent arterial bypass in neurosurgery. World Neurosurg. 2017;103:952.e5–952.e9. doi: 10.1016/j.wneu.2017.04.083. [DOI] [PubMed] [Google Scholar]
- 11.Woitzik J, Horn P, Vajkoczy P, Schmiedek P. Intraoperative control of extracranial-intracranial bypass patency by near-infrared indocyanine green videoangiography. J Neurosurg. 2005;102:692–8. doi: 10.3171/jns.2005.102.4.0692. [DOI] [PubMed] [Google Scholar]