Abstract
Introduction:
The purpose of this study was to compare the stress distributions in the teeth treated through minimally invasive access (MIA) designs to those of the teeth treated through traditional straight-line access and their relationship to the final restoration using three-dimensional finite element analysis (FEA).
Materials and Methods:
Four FEA models of an extracted mandibular first molar were constructed. An intact model served as the control, whereas the other three were prepared with either an MIA or traditional straight-line access. Simulated composite access fillings with or without a simulated gold crown were applied to the models, followed by application of an occlusal load of 100 N. Von Mises stresses in the teeth were then calculated and analyzed.
Results:
Stress values within the dentin for baseline, MIA with composite filling, MIA with composite filling and crown, and traditional access with composite filling and crown were 10.14 MPa, 6.98 MPa, 11.79 MPa, and 16.81 MPa, respectively. Higher stress values indicate that the tooth is more prone to fracture.
Conclusions:
A traditional endodontic access cavity may render a tooth more susceptible to fracture compared with an MIA design.
Keywords: Finite element analysis, fracture, minimally invasive
INTRODUCTION
Minimally invasive, or ultraconservative, endodontic access preparations are utilized in an effort to preserve a greater amount of healthy occlusal tooth structure[1] and are gaining popularity among members of the endodontic community. With greatly improved visibility through the use of the dental microscope, and continual advances in instrument design, metallurgy, flexibility, and integrity, traditional straight-line access design could be replaced using a smaller, more conservative (minimally invasive access [MIA]) with the idea that conservation of tooth structure will limit or reduce the stresses of endodontically treated teeth and improve their overall integrity through the reduced removal of tooth structure. Therefore, MIA can be described as a cavity design which allows access to and instrumentation of every canal while preserving as much of the hard tooth structure as possible.[1]
The choice of the final restoration for endodontically treated teeth is multifactorial. As Reeh and Messer have demonstrated, endodontic access alone only contributes to a 5% reduction in tooth stiffness, with the loss of marginal ridge integrity being the major contributor.[2] Aquilino and Caplan also showed that endodontically treated teeth not crowned after obturation were lost at six times greater rate than teeth crowned after obturation, concluding that there is a strong association between crown placement and the survival of endodontically treated teeth.[3]
However, with the trend toward smaller and more conservative access designs, come questions concerning the need for cuspal coverage of endodontically treated molars having otherwise intact and unrestored crowns. Furthermore, up for debate, is whether these MIAs offer any potential benefits to the teeth treatment planned for full coronal coverage restorations. Till date, these ideas of conservative access designs being utilized to improve tooth strength and integrity while limiting fracture susceptibility following root canal treatment (RCT) has not been investigated.
Three-dimensional (3D) finite element analysis (FEA) is used to determine the distribution of stress when a structure is subjected to force using computer-generated models utilizing data from micro-computed tomography (CT) scans.[4,5] With this technology, previous studies[6,7,8] have investigated the stress distributions in the canals of endodontically treated teeth, but have yet to consider the impact of such stresses based on the size of the access, and how these forces contribute to the tooth's crown strength or final restoration. Therefore, the purpose of this study is to compare the stress distributions in the teeth treated through MIA designs to those of the teeth treated through traditional straight-line access and their relationship to the final restoration using 3D FEA.
MATERIALS AND METHODS
Preparation of tooth
An intact, extracted human mandibular first molar with fully formed roots and patent canals was used. The tooth received preoperative radiographs in both the buccal-lingual and proximal dimensions as well as a preoperative microCT scan. MIA was performed using a #2 Endo-Access bur (Dentsply Maillefer, North America) mounted in a high-speed handpiece with water cooling. The access cavity was located in the central fossa, allowing localization and entry to all three canal orifices from different visual angulations while maintaining part of the chamber roof, excluding pulp horns. Root canals were negotiated with size 10 K-type files (Flexofile; Dentsply Maillefer, Ballaigues, Switzerland) until the tip of the file was visualized exiting the apical foramen. Working length was determined by subtracting 1 mm from the length of the visualized file. Each canal was instrumented to the established working length using LightSpeed LSX rotary files (Kerr Endodontics, United States) to a master apical file size 35 in each mesial canal and size 45 in the distal canal using 17% ethylenediaminetetraacetic acid irrigation between each instrument. Postinstrumentation radiographs in the same dimensions and a micro-CT scan were performed before obturation and again after obturation. Canals were then dried with paper points and obturated with gutta-percha and EndoSequence BC sealer (Brasseler USA, Savannah, Georgia) using the synchronized hydraulic compaction technique.
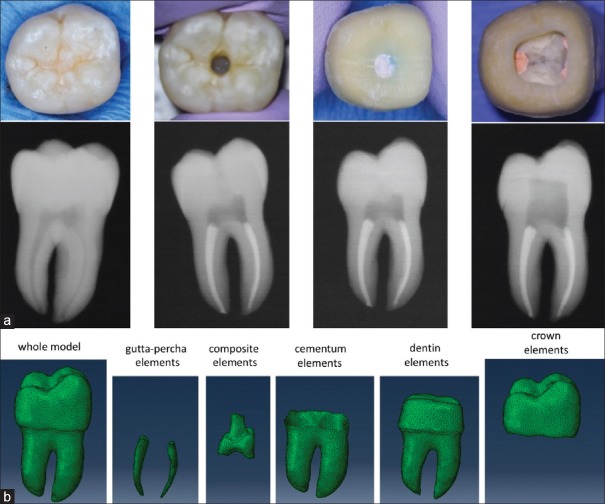
Following obturation, the access cavity was temporized with a cotton pellet and Cavit temporary filling. An impression of the tooth was made using Regisil PB (DENTSPLY Caulk, Milford, DE) for use as a template. The tooth was prepared for a full gold crown, and a provisional was fabricated using injectable Integrity Temporary Crown and Bridge Material (DENTSPLY Caulk, Milford, DE). Radiographs and a micro-CT scan were repeated with the temporary crown on the tooth for simulation of a final full coverage restoration. The temporary crown was removed, and the MIA was enlarged to represent an ideal straight-line endodontic access design. Radiographs and the micro-CT scan were repeated as before [Figure 1a].
Figure 1.
Clinical and radiographic overview of access modification, obturation, and crown preparation (a). Generation of three-dimensional finite element analysis models following segmentation into constituent parts and meshing (b)
Finite element analysis processes
The micro-CT scans obtained at baseline (unmodified), after MIA, MIA with a crown, and traditional access with a crown were utilized in the FEA process. Composite was not generally present in the restored micro-CT scans as the sequentially more invasive designs were imaged to see the enlarged access. The locations where composite would be used (enlarged access cavities and pulp chambers) in a completed restoration were identified, and material properties for a bulk-fill composite (X-tra fil; VOCO GmbH, Cuxhaven, Germany) were assigned in the models. In addition, the scanned temporary crown was assigned material properties of a full gold crown. Therefore, four 3D geometric models were reconstructed: (1) baseline (intact molar), (2) MIA molar with composite restoration, (3) MIA molar with composite restoration and full gold crown, and (4) conventionally, accessed molar with composite restoration and full gold crown.
Development of finite element analysis models
Models were created from micro-CT by use of Mimics (v19, Materialise, Belgium). Masks were created from thresholding, region grow, and morphology operations. The draw tool was used manually at times to identify the boundary between dentin and cementum, as imaging artifacts and quality prevented automatic detection. Due to issues with remeshing of disconnected bodies in 3-matic (v11, Materialise, Belgium), the canals within the root were masked separately. The Boolean tool was used to ensure the masks did not overlap and had no gaps between the components – which included pulp zone, dentin, cementum, roots, enamel, and/or crown. The masks were linked together in an inside-out order before conversion to a 3D model so that 3-matic could properly create an assembly.
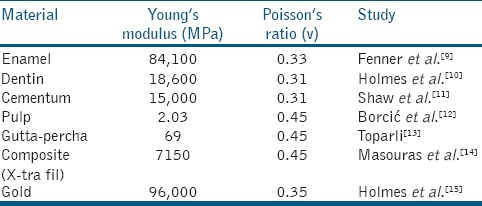
In the 3-matic software (v11, Materialise, Belgium), the Uniform Remesh was used on each of the parts, with parameters of 0.3 triangle edge length, auto fix enabled, and two iterations [Figure 1b]. The result of the triangles was checked by turning on filled with triangle edges view. Then, a non-manifold assembly was created with the cementum as the main entity and the rest as the intersecting entity. Following that, the Volume Mesh tool was used to fill the surface meshes. The parts were selected individually, with the parameters as Tet4, control edge length (check), maximum edge length 0.5, shape measure of R-in/R-out (N), shape quality threshold of 100, and growth rate of 60%. The parts were then copied and pasted into the same Mimics file the meshes were exported from, and each part was then assigned material values [Table 1].
Table 1.
Material values applied based on previously reported studies
To check if everything was remeshed properly, the volume meshes were exported to Abaqus from 3-matic. First, a section of the tooth was selected, then the Remove tool was used to check the inside quality of the meshes. The meshes were edited accordingly when not up to satisfaction. Figure 2 diagrams how the models were then exposed to distributed loading (100 N) over the occlusal surface simulating forces of mastication.[16,17]
Figure 2.
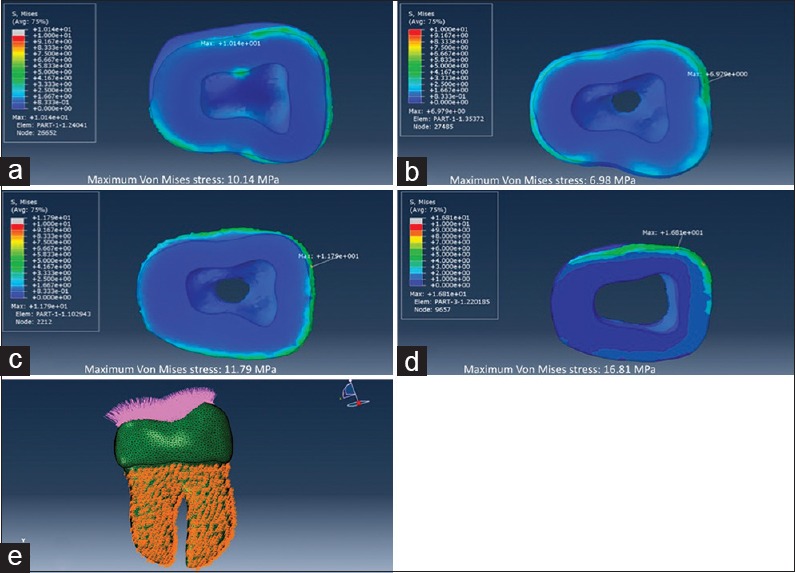
Maximum von Mises stress values (MPa) within the dentin under 100 N of total force applied to the occlusal surface for baseline (a), minimally invasive access with composite filling (b), minimally invasive access with composite filling and crown (c), and traditional access with composite filling and crown (d). Distributed loading (100 N) over the occlusal surface simulating forces of mastication with fixation in all directions of the cementum surface (boundary condition) (e)
RESULTS
Stresses at loads of 100 N are far from those needed to cause fracture in all models. Under 100 N total force applied to the occlusal surface, maximum von Mises stress values within the dentin for baseline, MIA with composite filling, MIA with composite filling and crown, and traditional access with composite filling and crown were 10.14 MPa, 6.98 MPa, 11.79 MPa, and 16.81 MPa, respectively [Figure 2]. Higher stress values indicate that the tooth is more prone to fracture.
DISCUSSION
Loss of tooth structure is one of the most important causes of fractures in endodontically treated teeth. MIA cavities have been recently proposed to reduce the risk of fracture in root-filled teeth.[18,19,20] Therefore, a more conservative access design aimed at conserving tooth structure may improve the overall prognosis of these teeth.[21] On the contrary, there is a debate as to whether an efficient endodontic treatment is feasible through a small access cavity design. A study showed that MIA resulted in increased resistance to fracture, but it compromised the cleaning and shaping of some of the canals.[20] However, the authors concluded that the benefits of MIA for premolars and molars may outweigh the risks. Another recent study found that, when using a microscope alone without ultrasonic troughing, fewer canals were located with MIA compared to traditional access. In addition, it was found that canal transportation was significantly higher for the MIA group.[22] In general, conflicting findings have been reported regarding the effect of MIA on overall endodontic treatment. However, it is imperative to understand that the present study did not assess the efficacy of endodontic treatment through MIA, only the fracture resistance was evaluated. In this study, the stress distributions in teeth treated through MIA design were compared to those of teeth treated through traditional straight-line access and their relationship to the final restoration using 3D FEA. Until now, no similar study in the literature has addressed this through the use of computer-generated models focusing solely on access size.
For this investigation, a mandibular first molar was studied because not only is it commonly indicated for endodontic treatment but also the majority of these teeth are also restored with full-coverage crowns following RCT. Root canal instrumentation was completed with LSX instruments with the intention of preparing the apical portion of the canals to an acceptable size while avoiding exaggerated removal of cervical dentin. In addition, FEA was incorporated into the design of this study to limit the variables and provide controlled analysis conditions. Moreover, it allows the investigators an infinite opportunity to apply stresses to the same tooth without actually causing fracture of the specimen. It also provides 3D analysis of where the stresses are concentrated throughout the various dental materials, both natural and synthetic. In this study, the roots and root canal condition remained the same for all samples. The only variables that changed were the size of endodontic access and coronal restoration.
The results of this investigation showed higher stress values in the tooth prepared with a traditional access cavity, compared to the tooth with an MIA, both with and without coronal coverage. These findings are in agreement with another recently published study by Plotino, et al. In their study, evaluating fracture strength of endodontically treated teeth with various access cavity designs, 160 teeth were loaded to fracture in a mechanical material testing machine. They found that the teeth with traditional access cavity designs showed lower fracture strength than those prepared with minimally invasive designs.[23] The present study also showed higher stresses in the precervical region, which is a zone critical for transferring load from the occlusal table to the root. This finding confirms the anecdotal claims that preserving precervical dentin may increase the tooth's resistance to coronal fracture.[18]
The FEA models employed in the present study are simplifications, and presume perfectly filled and bonded interiors with uniform properties within constituents. Therefore, the results of FEA cannot reflect a perfect interpretation for clinical situations. As an example, dentin has been observed by others to fail at 297 MPa of stress.[24] If loads increased to by about ×50, we could more easily see the stress patterns within the dentin and the differences between access preparations. Another interesting finding in this study was that the baseline tooth showed a higher stress value (10.14 MPa) compared to the MIA with composite filling tooth (6.98 MPa), indicating that the latter is less prone to fracture. One explanation for this is the fact that when using FEA, the simulated composite restoration is assumed to be solid and completely bonded 3D to the tooth. This, therefore, results in a stronger model than the baseline tooth with an empty pulp chamber, lacking the added benefits of a bonded restoration. While this may prove to have some validity, it is unlikely that this represents a true clinical situation in which the restoration is completely free of voids and perfectly bonded to every surface of the access cavity. In addition, a single tooth and tooth type were used without the presence of periodontal ligament or bone simulated. Further studies with improved models and additional teeth are required to more accurately predict the biomechanical responses of endodontically treated teeth through MIA cavity designs.
CONCLUSIONS
Within the limitations of this study, it can be concluded that a traditional endodontic access cavity may render a tooth more susceptible to fracture compared with an MIA design. Removal of additional tooth structure for crown fabrication yielded higher stress patterns in all cases, regardless of the access size.
Acknowledgement
“Dr. Allen and Dr. Meyer contributed equally to this study”.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yuan K, Niu C, Xie Q, Jiang W, Gao L, Huang Z, et al. Comparative evaluation of the impact of minimally invasive preparation vs. Conventional straight-line preparation on tooth biomechanics: A finite element analysis. Eur J Oral Sci. 2016;124:591–6. doi: 10.1111/eos.12303. [DOI] [PubMed] [Google Scholar]
- 2.Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod. 1989;15:512–6. doi: 10.1016/S0099-2399(89)80191-8. [DOI] [PubMed] [Google Scholar]
- 3.Aquilino SA, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent. 2002;87:256–63. doi: 10.1067/mpr.2002.122014. [DOI] [PubMed] [Google Scholar]
- 4.Gao Y, Peters OA, Wu H, Zhou X. An application framework of three-dimensional reconstruction and measurement for endodontic research. J Endod. 2009;35:269–74. doi: 10.1016/j.joen.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 5.Trivedi S. Finite element analysis: A boon to dentistry. J Oral Biol Craniofac Res. 2014;4:200–3. doi: 10.1016/j.jobcr.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng R, Zhou XD, Liu Z, Hu T. Development of a finite element analysis model with curved canal and stress analysis. J Endod. 2007;33:727–31. doi: 10.1016/j.joen.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 7.Sathorn C, Palamara JE, Palamara D, Messer HH. Effect of root canal size and external root surface morphology on fracture susceptibility and pattern: A finite element analysis. J Endod. 2005;31:288–92. doi: 10.1097/01.don.0000140579.17573.f7. [DOI] [PubMed] [Google Scholar]
- 8.Santos AF, Tanaka CB, Lima RG, Espósito CO, Ballester RY, Braga RR, et al. Vertical root fracture in upper premolars with endodontic posts: Finite element analysis. J Endod. 2009;35:117–20. doi: 10.1016/j.joen.2008.09.021. [DOI] [PubMed] [Google Scholar]
- 9.Fenner DN, Robinson PB, Cheung PM. Three-dimensional finite element analysis of thermal shock in a premolar with a composite resin MOD restoration. Med Eng Phys. 1998;20:269–75. doi: 10.1016/s1350-4533(98)00011-3. [DOI] [PubMed] [Google Scholar]
- 10.Holmes DC, Diaz-Arnold AM, Leary JM. Influence of post dimension on stress distribution in dentin. J Prosthet Dent. 1996;75:140–7. doi: 10.1016/s0022-3913(96)90090-6. [DOI] [PubMed] [Google Scholar]
- 11.Shaw AM, Sameshima GT, Vu HV. Mechanical stress generated by orthodontic forces on apical root cementum: A finite element model. Orthod Craniofac Res. 2004;7:98–107. doi: 10.1111/j.1601-6343.2004.00285.x. [DOI] [PubMed] [Google Scholar]
- 12.Borcić J, Antonić R, Urek MM, Petricević N, Nola-Fuchs P, Catić A, et al. 3-D stress analysis in first maxillary premolar. Coll Antropol. 2007;31:1025–9. [PubMed] [Google Scholar]
- 13.Toparli M. Stress analysis in a post-restored tooth utilizing the finite element method. J Oral Rehabil. 2003;30:470–6. doi: 10.1046/j.1365-2842.2003.01090.x. [DOI] [PubMed] [Google Scholar]
- 14.Masouras K, Silikas N, Watts DC. Correlation of filler content and elastic properties of resin-composites. Dent Mater. 2008;24:932–9. doi: 10.1016/j.dental.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 15.Holmes DC, Haganman CR, Aquilino SA, Diaz-Arnold AM, Stanford CM. Finite element stress analysis of IMZ abutment designs: development of a model. J Prosthodont. 1997;6:31–6. doi: 10.1111/j.1532-849x.1997.tb00062.x. [DOI] [PubMed] [Google Scholar]
- 16.Rodrigues FP, Li J, Silikas N, Ballester RY, Watts DC. Sequential software processing of micro-XCT dental-images for 3D-FE analysis. Dent Mater. 2009;25:e47–55. doi: 10.1016/j.dental.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 17.Santos-Filho PC, Veríssimo C, Raposo LH, Noritomi MecEng PY, Marcondes Martins LR. Influence of ferrule, post system, and length on stress distribution of weakened root-filled teeth. J Endod. 2014;40:1874–8. doi: 10.1016/j.joen.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 18.Clark D, Khademi J. Modern molar endodontic access and directed dentin conservation. Dent Clin North Am. 2010;54:249–73. doi: 10.1016/j.cden.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Clark D, Khademi JA. Case studies in modern molar endodontic access and directed dentin conservation. Dent Clin North Am. 2010;54:275–89. doi: 10.1016/j.cden.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Krishan R, Paqué F, Ossareh A, Kishen A, Dao T, Friedman S, et al. Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars. J Endod. 2014;40:1160–6. doi: 10.1016/j.joen.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 21.Ikram OH, Patel S, Sauro S, Mannocci F. Micro-computed tomography of tooth tissue volume changes following endodontic procedures and post space preparation. Int Endod J. 2009;42:1071–6. doi: 10.1111/j.1365-2591.2009.01632.x. [DOI] [PubMed] [Google Scholar]
- 22.Rover G, Belladonna FG, Bortoluzzi EA, De-Deus G, Silva EJ, Teixeira CS, et al. Influence of access cavity design on root canal detection, instrumentation efficacy, and fracture resistance assessed in maxillary molars. J Endod. 2017;43:1657–62. doi: 10.1016/j.joen.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 23.Plotino G, Grande NM, Isufi A, Ioppolo P, Pedullà E, Bedini R, et al. Fracture strength of endodontically treated teeth with different access cavity designs. J Endod. 2017;43:995–1000. doi: 10.1016/j.joen.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 24.Rodrigues MP, Soares PBF, Valdivia AD, Pessoa RS, Veríssimo C, Versluis A, et al. Patient-specific finite element analysis of fiber post and ferrule design. J Endod. 2017;43:1539–44. doi: 10.1016/j.joen.2017.04.024. [DOI] [PubMed] [Google Scholar]