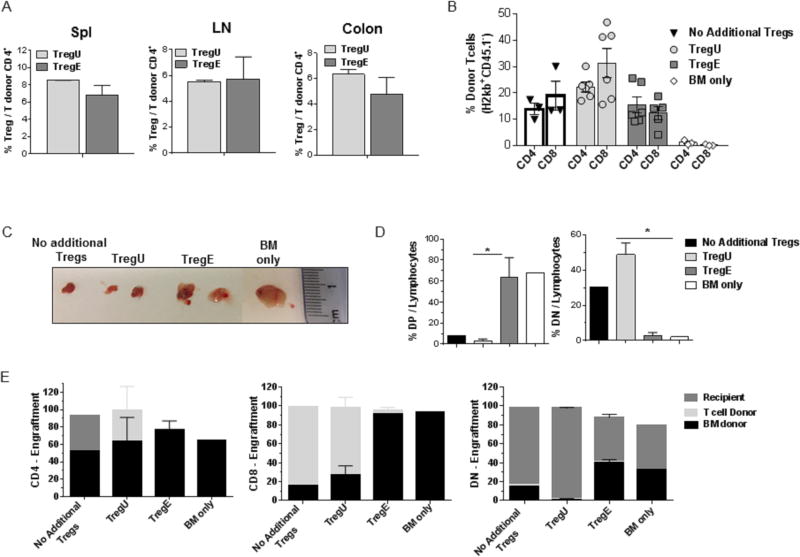
Figure 3. Recipients of TL1A-Ig+IL-2 expanded Tregs develop a normal pattern of thymic differentiation and accompanied by donor stem cell derived long term engraftment after MHC-mismatched aHSCT.
A complete MHC-mismatched aHSCT was performed (as in Fig 2) transplanting sorted CD4+FoxP3+ unexpanded and expanded Tregs (175,000-200,000) together with B6-wt 1×106 splenic T cells and 5.5×106 TCD B6-CD45.1 BM cells. Recipient mice were bled / sacrificed at different time points post-aHSCT. (A) Similar Treg levels were found in TregU and TregE recipient spleen (Spl), lymph nodes (LN) and colon 1 week after transplantation. Data are representative of 3 independent experiments. (B) Frequency of CD4+ and CD8+ cells present in the blood of recipients of the indicated groups one month post-aHSCT. Results demonstrated only TregE recipients did not contain an inverted CD4/CD8 ratio (C-E). Five weeks after transplant, the thymus was evaluated. (C) Representative photographs of thymi indicate larger thymic size in the TregE vs TregU recipients. (D) Frequency of CD4+CD8+ double-positive (DP) and CD4−CD8− (DN) thymocytes cells out of total lymphocytes. TregE thymi showed virtually normal levels of DP and DN subsets comparable to recipient to of BM only. Data were analyzed by a two-tailed unpaired t test. *p<0.05. (E) Determination of origin of thymocyte populations, i.e. BM donor, T cell donor or recipient. TregE but not TregU recipients contained levels of BM derived thymocytes comparable to recipients of donor BM only. Data are expressed as means ± SEM.