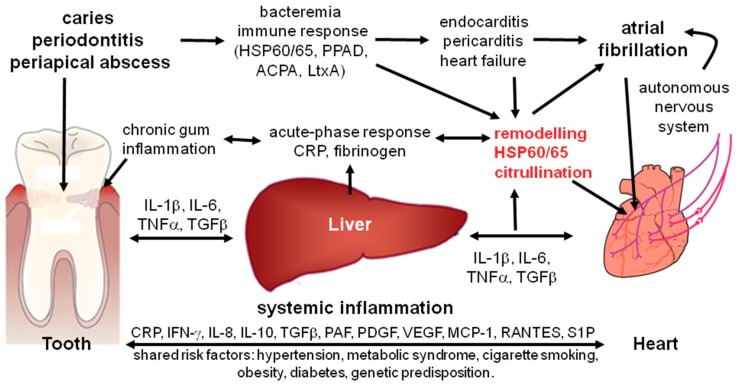
Figure 3.
Potential role of the oral inflammation in the pathogenesis of atrial fibrillation. Chronic oral inflammation induced by bacterial biofilm (gingivitis, periodontitis, and apical endodontic lesions) cause a localized inflammation, which affects cardiac structural and electrophysiological remodeling linked to atrial fibrillation by: (i) low level bacteremia by which oral bacteria enter the blood stream at inflamed sites of the oral cavity and invade the heart; (ii) systemic inflammation induced by inflammatory mediators which are released from the sites of oral inflammation into the blood stream, affecting ventricular remodeling; (iii) autoimmunity against molecular structures expressed in the heart, such as HSP60/65 and citrullinated cardiac proteins, caused by the host immune response to specific components of oral pathogens; (iv) arrhythmogenic effects mediated by activation of the autonomic nervous system during inflammation; (v) effects resulting from specific bacterial proteins and toxins, such Porphyromonas gingivalis PAP and leukotoxin A (LtxA) that are produced by oral pathogenic bacteria and induce the formation of anticitrullinated protein antibodies (ACPA). Abbreviations: CRP: C-reactive protein; IL: interleukin; IFN: interferon; MCP: monocyte chemoattractant protein; PAF: platelet activating factor; PDGF: platelet-derived growth factor; RANTES: regulated on activation, normal T cell expressed and secreted; S1P: sphingosine-1-phosphate; TNF: tumor necrosis factor; VEGF: vascular endothelial growth factor.