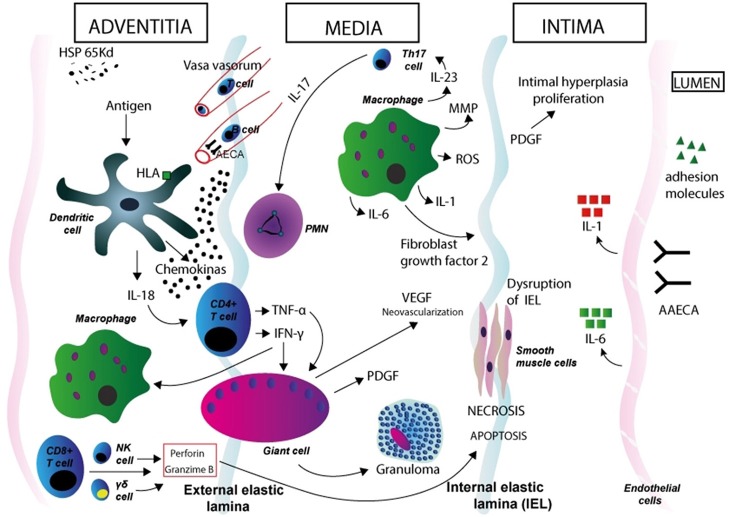
Figure 1.
Immunopathogenesis of Takayasu arteritis. Schematic figure showing possible mechanisms in the aortic wall. Dendritic cells in the adventitia expressing specific HLA molecules are activated by a stimulus so far unrecognized. Expression of the 65 kDa HSP in the aortic tissue might play a role in dendritic cell activation. These cells synthesize and release proinflammatory cytokines (such as IL-18) and homing chemokines that recruit T cells to the vessel wall and initiate an aberrant T cell response. After interaction with dendritic cells, CD4-positive T cells with a Th1 phenotype release cytokines such as interferon (IFN)-γ and tumor necrosis factor (TNF)-α, which induce differentiation and increased function of macrophages, and also induce the coalescence of multinucleated giant cells, thus promoting the formation of granuloma. T cells with an induced Th17 phenotype release IL-17, which attracts and activates neutrophils in the vessel wall. Macrophages release IL-1 and IL-6, MMP, and ROS (which induce oxidative injury and degradation of media and intima layers, and disruption of the elastic laminae), VEGF (leading to neoangiogenesis), FGF, and PDGF, which results in exuberant intimal proliferation. These phenomena contribute to the structural damage in the aortic wall. IFN-γ, TNF-α, IL-6, IL-8, IL-17A, and IL-18 likely play a role in vessel wall damage (through the recruitment of mononuclear cells in the vessel wall) and systemic features of TA. CD8-positive T cells, γδ T-cells, and natural killer (NK) cells release of perforin and granzyme-B, which contribute to apoptosis and necrosis of smooth muscle cells and damage in the intimate layer. AAECA may also have a role in pathogenesis through the activation of endothelial cells and induction of complement- and cell-mediated cytotoxicity. Degenerative changes in the media and adventitia, as well as intimal fibrocellular hyperplasia, eventually lead to muscular layer weakening, aneurismal formation, vascular stenosis and thrombus formation. HSP, heat shock protein; HLA, human leukocyte antigen; PMN, polymorphonuclear neutrophil; NK, natural killer cell; MMP, matrix metalloproteinase; ROS, reactive oxygen species; PDGF, platelet-derived growth factor; VEGF, vascular endothelial growth factor; FGF, fibroblast growth factor; AAECA, anti-aortic endothelial cell antibodies.