Abstract
Female sex workers are particularly susceptible to HIV infection in Russia. However, a dearth of information exists on their utilization of HIV services. A mixed-methods, cross-sectional study was conducted to examine motivators and barriers to HIV testing among street-based sex workers in St. Petersburg, Russia. The Health Belief Model was the theoretical framework for the study. Twenty-nine sex workers participated in in-depth interviews, and 139 sex workers completed interviewer-administered surveys between February and September 2009. Barriers to getting an HIV test were fear of learning the results, worrying that other people would think they were sick, and the distance needed to travel to obtain services. Motivators for getting tested were protecting others from infection, wanting to know one’s status and getting treatment if diagnosed. Logistic regression analysis demonstrated that knowing people living with HIV [aOR=6.75, 95% CI (1.11, 41.10)] and length of time since start of injection drug use [aOR=0.30, 95% CI (0.09, 0.97)] are significantly associated with recently getting tested. These results are important to consider when developing public health interventions to help female sex workers in Russia learn their HIV status and get linked to care and treatment services if needed.
Keywords: HIV testing, sex workers, Russia
Introduction
St. Petersburg, the second largest city in Russia, has consistently been among the cities contributing the largest number of HIV cases (57,009 registered cases in 2014), in a country with an expanding epidemic (Federal AIDS Center, 2014). The epidemic is largely concentrated among people who inject drugs (PWID), though sexual transmission accounts for a growing proportion of new HIV cases in the country. In 2014, 57.3% of newly diagnosed HIV cases were attributable to injection drug use transmission and 40.3% were attributable to heterosexual transmission (Federal AIDS Center, 2014). An estimated 40% of PWIDs are female (Benotsch et al., 2004), and approximately one-third of female PWID are involved in sex work (Benotsch et al., 2004, Kozlov et al., 2006). A large gap in information exists for Russia on the epidemiology of HIV among female sex workers, although the available data indicate an HIV epidemic among women involved in both sex work and injection drug use (Shannon et al., 2015). The most recent study in St. Petersburg showed that 48% of street-based female sex workers tested positive for HIV (WHO, 2004).
While HIV testing and treatment services are available in Russia, it has been shown that these services are not reaching the populations most vulnerable and in need. HIV testing remains sub-optimal among PWIDs in Russia (Grau et al., 2011). Less than half of people living with HIV (PLHIV) in Russia have been diagnosed with HIV and 23% of those diagnosed are not linked to care (Pokrovskaya et al., 2014). The UNAIDS Gap Report (2014) noted that late diagnosis of HIV-infections is a problem in Eastern Europe, and recognized sex workers to be among the groups disproportionately affected by the growing epidemic in the region. A study in three Russian cities showed that 86.5% of female sex workers had previously received an HIV test, and showed a 3.9% prevalence of HIV among female sex workers (Decker et al., 2013); however, as the authors mentioned, this study did not include St. Petersburg. Fear of stigma and discrimination have been shown to be institutional barriers to accessing HIV services for female sex workers in Russia (King et al., 2013). Overall, there remains a dearth of information about accessing HIV testing services and about the motivators and barriers to getting tested for HIV among female sex workers, including the particularly vulnerable subpopulation of female sex workers who are also injecting drugs. The objective of this study was to gain a more thorough understanding of the motivators and barriers for the utilization of HIV testing services among street-based female sex workers in St. Petersburg.
Methods
Study design
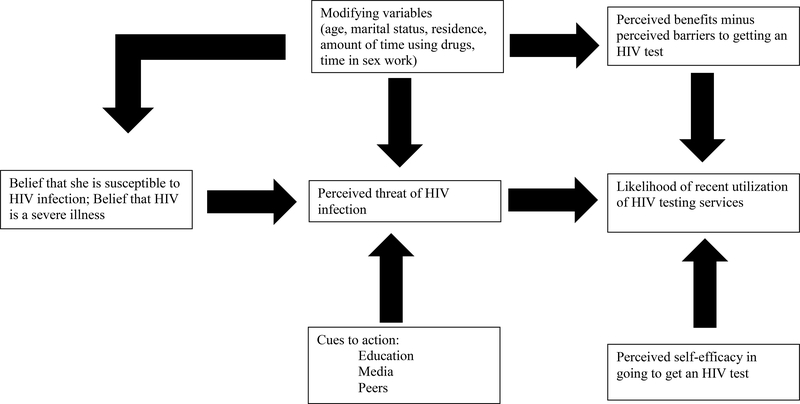
This mixed-methods study was designed using a transformative strategy, meaning that the quantitative and qualitative methods complement each other and are guided by a theoretical perspective (Creswell, 2003). While data collection was done in phases, final analysis was conducted concurrently. The Health Belief Model (HBM) guided this study (Figure 1). Developed by Rosenstock (1966), the HBM is often used to explain the relationship between health behaviors and service utilization (Shahrabani & Benzion, 2012). Triangulation of the data occurred during data collection and analysis. The first author/principal investigator (PI), a US researcher, who had previously studied and worked in Russia for several years, spent ten months as a visiting scholar in the Faculty of Sociology at St. Petersburg State University to do fieldwork for this study. The qualitative component was the first phase. Doing the qualitative interviews first helped to build trust with the community and plan for the logistics of implementing the survey data collection. Also, the preliminary qualitative findings were used to finalize the quantitative questionnaire. Additional qualitative work was done later for further exploration and explanation of the preliminary trends in the data. Participants were eligible to complete either or both the qualitative or quantitative interviews, and participation in one component was not contingent upon participation in the other. It is likely that there was overlap between the qualitative and quantitative participants, but there was no documentation made given that participation was anonymous in both components in order to adhere to research ethics. Data collection occurred between February and September 2009. The Ethics Review Committee at St. Petersburg State University and the Institutional Review Board at the University of North Carolina at Chapel Hill approved all research protocols. Verbal informed consent was obtained from each participant and anonymity of participation was guaranteed.
Figure 1.
Health belief model constructs and recent utilization of HIV testing services
Qualitative component
A purposive sampling strategy was used to recruit women for in-depth interviews. The inclusion criteria for participation was self-report of currently being engaged in street-based sex work in St. Petersburg and at least 18 years of age. Participants were recruited through a nongovernmental organization that provides mobile outreach services to female sex workers around the city. The outreach services typically included the provision of condoms and needles, the referral for testing for HIV and other sexually transmitted infections, and other sexual health education activities. HIV testing was not part of the routine services offered at the time of the study. Topics of the in-depth interviews included: awareness and knowledge of HIV, risk perceptions, sources of information about HIV, perceived barriers and benefits to getting tested for HIV, experiences testing for HIV, and experiences receiving follow-up care if tested positive. We also asked sex workers to reflect on experiences in clinical HIV testing sites and did not ask questions directly related to any HIV testing they might have received as part of the outreach services.
The PI conducted 25 interviews in Russian until data saturation was achieved, meaning that she noticed overlap in the information that participants were sharing about the topics of interest for this study. The PI later conducted interviews with an additional 4 sex workers who had tested positive for HIV and were enrolled in care and support services for PLHIV. The objective of these interviews was to assess how these women overcame barriers to accessing HIV services or incorporated facilitators in order to access services, including HIV testing.
All interviews were conducted in a private space with only the PI and participant present. The PI, a foreign visiting scholar at St. Petersburg State University, had no affiliation with the nongovernmental organization where participants were recruited. Also, participants were ensured during the informed consent process that participation in the study had no implications on the services received through the organizations. Interviews were transcribed and the texts were imported into Atlas.ti for coding. Deductive coding was done based on the theoretical constructs from the HBM. Inductive coding was used to identify emerging themes from the data that had not been pre-identified from the deductive coding.
Quantitative component
A community-based sample of participants was recruited through two organizations that independently operate mobile outreach van services to street-based female sex workers. Participants were recruited until no new potential recruits appeared at either organization. The interviewer-administered questionnaire took approximately 15–20 minutes to complete.
Data analysis was conducted using the SAS 9.1 statistical software program. Logistic regression was used to determine which factors were significantly associated with HIV testing. The outcome variable was dichotomized as recent HIV test (received in the previous six months) versus no recent HIV test, given that some health care providers recommend that individuals engaging in high risk behaviors get tested for HIV every three to six months (HHS, 2014). Observations were excluded in the logistic regression analysis if a participant reported an HIV-positive status and had tested more than six months ago, assuming that someone would not seek an HIV test after diagnosis. The independent variables were based on the constructs from the HBM. The items representing each construct were used in previous studies on HIV testing. Perceived susceptibility was measured by ‘I think that I can get HIV’ (Lux & Petosa, 1995). Perceived severity was measured by ‘If I were to get HIV, it would be bad for my health’ (Lux & Petosa, 1995). Perceived self-efficacy was measured by ‘I could easily arrange to have an HIV test if I wanted one’ (Vermeer et al, 2008). Potential perceived barriers and benefits were taken from a previous study on HIV testing and listed in Tables II and III (Genberg et al, 2009). Based on the qualitative findings, the measure for “knowing a PLHIV” was included in the model. Demographic variables were also included in the regression model: residency, marital status, time spent in sex work and time using drugs. Age was not included in the multivariate analyses given that the test for co-linearity showed age to be highly correlated with the amount of time using drugs. The variables that showed an odd ratio that was significant at the p=.05 level in the logistic regression model were considered to be significantly associated with a recent HIV test among the sample of women who were HIV-negative, unaware of their status, or received an HIV diagnosis in the previous six months.
Table II.
Barriers to getting an HIV test (N=139)
| Reasons not to get tested | n(%) agreed |
|---|---|
| Nervous to get results | 76 (54.7%) |
| Worried about partner’s reaction | 67 (48.2%) |
| Worried people will think I am sick | 61 (43.9%) |
| Too far from home | 56 (40.3%) |
| It is not important to me | 34 (24.4%) |
| Doubt confidentiality | 33 (23.7%) |
| Can’t leave work | 21 (15.1%) |
| I am not at risk | 20 (14.4%) |
| Results take too long | 15 (10.8%) |
| Too expensive | 11 (7.9%) |
| Don’t know where to test | 10 (7.2%) |
| Never thought of testing | 6 (4.3%) |
| Afraid of needles | 3 (2.2%) |
Table III.
Benefits to getting an HIV test (N=139)
| Reasons to get tested | n (%) agreed |
|---|---|
| Could protect others if tested positive | 134 (96.4%) |
| Want to know status | 132 (95.0%) |
| Could get treatment if tested positive | 123 (88.5%) |
| Want to stop worrying | 120 (86.3%) |
| Important for job | 116 (83.5%) |
Results
Description of sample
Twenty-nine women participated in in-depth interviews. The women ranged in age between 21 and 38 years old. Twenty-three of the participants were unmarried; and about half (n=15) had children. Time spent in sex work ranged from 1.5 years to 11 years. All of the participants were either currently using or had previously used injection drugs. All women reported that they had been tested for HIV at least once. Eleven of the 29 women disclosed during the interviews that they had HIV.
One hundred thirty-nine women participated in the interviewer-administered questionnaire. The women ranged in age between 19 and 41 years old (mean= 29 years, median=28 years). The majority of the women were unmarried (62%); and, about half (52%) had children. Time spent in sex work ranged from 2 weeks to 20 years (mean time = 5.26 years, median=4 years). Almost all participants reported current injection drug use (99%). Length of time using drugs ranged from 8 months to 25 years (mean time=8.86 years, median=8 years). Nearly all survey participants had tested for HIV (97%, n=136). Having been tested for HIV six months earlier was the median and mode answer to the question on the time of the most previous HIV test. Over one-third of the sex workers had been diagnosed with HIV (34%, n=47).
Factors influencing the utilization of HIV testing services
Table I provides a summary of key findings. The left-hand column indicates the findings from the quantitative component; and, the right-hand column provides a summary of the findings from the qualitative data.
Table I.
Health beliefs regarding the need for HIV testing and treatment services among female sex workers in St. Petersburg, Russia (quantitative N=139; qualitative N=29)
| Construct | Quantitative Findings | Qualitative Findings |
|---|---|---|
| Perceived Susceptibility | 40 (43%) of HIV-negative women greatly perceived themselves to be at risk for HIV 83 (60%) said it depended on fate |
--Nearly all participants were cognizant of risk, but many said that they are protecting themselves and therefore risk perception is lower --Participants noted that whether or not they acquire HIV is determined by chance or fate |
| Perceived Severity | 137 (99%) of the women perceived HIV to be a threat to their health | --Some were very afraid, but others cited knowing PLHIV that did not have symptoms --HIV-positive participants also had mixed perceptions about how severe the virus was |
| Perceived Self-efficacy | 48 (35%) had high perceived self-efficacy for going for an HIV test | -- Many participants recognized personal motivation as a factor in accessing services --Drug use inhibited one’s ability to get services |
| Perceived Barriers | 76 (55%) too nervous to get results 67 (49%) worried about partner’s reaction 61 (44%) worried that people will think they are sick 56 (40%) said testing sites were too far away |
--Distance needed to travel was a commonly cited barrier --Time away from work/doing everything they can just to survive were barriers to going to get an HIV test --Fear of learning results, but also fear of having it documented inhibited participants from getting tested for HIV |
| Perceived Benefits | 134 (96%) cited being able to protect others was a benefit of getting tested 132 (95%) said they would want to know their status |
--Wanting to protect others (partners, children) were cited as reasons for getting tested --Concern about one’s health motivated participants to get tested --Reassurance was a common reason for getting tested -- Many participants talked about getting tested for HIV because it was necessary for obtaining documents |
| Cues to Action | 131 (94%) talked with someone about HIV 129 (93%) knew PLHIV 121 (87%) received educational materials |
--HIV was talked about among people who inject drugs, but less discussed with other sex workers --Participants did not always talk in-depth about HIV with peers -- The majority of participants felt they were informed about HIV |
Perceived susceptibility
In the quantitative component, 43% of HIV-negative participants completely agreed that they could become infected with HIV, and 60% agreed that if it is their fate to get HIV, then they would become infected. The qualitative data highlighted the mixed feelings that sex workers held about their perceived risk for getting HIV. Participants recognized that they were involved in a profession that made them vulnerable to contracting HIV. ‘I say, “Yes, I am involved in prostitution, are you prepared?” I say, “I cannot be responsible”… we are all dependent on God, and sooner or later it could happen that I get sick.’ They also recognized that drug use could put them at risk for HIV, especially if they did not always follow all the steps of safer injection drug use.
It was common for sex workers to minimize their perception of susceptibility to HIV infection because of the precautions they take. For example, as one sex worker described in the in-depth interview:
If I only have sex with condoms, then I probably won’t get HIV. Although, of course, no one is insured, but I think that I won’t get it. I keep a close eye on everything, and I even take all the precautions when using drugs. I don’t use other people’s things.
While everyone talked about trying to protect themselves from HIV with clean needles and condoms, some sex workers, nonetheless, perceived themselves to be at risk and reported times when ‘I am feeling bad and really need something and there is nothing on hand. Then it is possible that you take whatever is lying around.’
Participants talked about reasons why they tested and this included perceived susceptibility to HIV infection and spreading the disease.
Just to know. So that I can be confident that I don’t have it. So that I can be calm. Because I work with people and, God forbid, I could transmit it to someone. Working in this profession you have to think not only about yourself, but about those around you.
When sex workers did not perceive themselves to be at risk for getting HIV, then there was not a reason to get an HIV test. As one participant replied to the question of whether or not she gets tested for HIV: ‘If I use condoms, if they don’t break, and if they are okay, then, why would I go get tested?’ Another participant talked about not getting tested for HIV because she did not feel that she was at risk for getting the virus.
So why would I get tested? Maybe I needed to. I don’t know…I cannot even understand why it is necessary. If I had the test, I know that it would be negative, and that I cannot become infected. There is no point. I will get tested if I needed to for going to the hospital. I do not believe that there is any point to just go and get tested.
Perceived severity
Perceived severity of HIV infection was high among the female sex workers in this study. Among the surveyed women, 99% agreed that if she were to contract HIV, it would be bad for her health. Many participants in the qualitative component also believed HIV to be severe. When asked what she knew about HIV, one participant replied ‘I know that it is a scary illness and that one can die. There is nothing good about it.’ In fact, most the women talked about HIV as being the illness they fear most. ‘I have hepatitis, but HIV?! I really don’t want to get infected.’ Despite the widespread fear of HIV, there were some women who talked about knowing people who had HIV and were not showing symptoms. As one woman discussed: ‘Well, as far as I know from the conversations I’ve had, people don’t really feel HIV. They don’t feel it.’
When female sex workers did not perceive HIV to be a very severe illness, then they were not as concerned with getting an HIV test. Additionally, the women who have HIV and did not perceive it to be a threat to their health were not utilizing HIV treatment and care services. The trend in the data indicated that the sex workers have an abstract understanding that HIV is a severe illness, but it is not necessarily the case that they apply this knowledge to themselves. Moreover, the absence of concrete symptoms is a barrier for utilizing treatment services.
Perceived self-efficacy
In the quantitative component, 35% of participants were completely confident that they could arrange to get an HIV test. In the qualitative component, many of the sex workers talked about personal motivation as a factor in whether or not one regularly gets an HIV test. Most of these women discussed it in the context of saying that they simply could not do it and did not provide much explanation, most often switching to external factors such as time, money or distance. Others blamed the injection drug use for affecting one’s motivation for doing anything related to caring about one’s health.
Of course, no one is going to demand these certificates [of clean health] on the street. So, it depends on the girl, on how she takes care of herself. If she is interested in her health, then of course, she will go to be tested. Otherwise, she will not.
This perceived self-efficacy to access care services was also an issue for women living with HIV. Aside from not feeling sick and therefore not thinking they needed services, women talked about ‘simply not being able to go’ to the AIDS Center. One woman said that what she needed was for someone to take her hand and lead her there, that she would not do it on her own.
Yes, I need to plan to go. And so that somehow, with someone, so that someone would support me in this, in this trip. I will probably never go alone. If someone, somehow, desirably on transport…umm, like in my condition, using drugs, to travel in those buses, somewhere, in the subway, for me this is totally horrible. Let’s say that if someone could help me with this trip, then I would go without further ado.
There were instances where sex workers said that they knew preventing HIV and getting an HIV test depended on their own motivation and supported the idea that ‘it is all possible. If you, yourself, want it.’ However, this was more often the case with HIV preventive behaviors rather getting tested. One participant highlighted the lack of inner-strength to go for an HIV test.
No, there are not any reasons. You know, I somehow have a calm attitude towards all of this. I am so quiet. I don’t go anywhere, just home and work. But, to go somewhere—for that after all, requires a lot of strength. Some kind of great breakthrough is needed for that.
While not all women felt that they could access HIV testing services, there were some women who perceived that they had a choice in getting the test and that the strength to do so was a personal motivator.
Perceived barriers to testing
In the quantitative component (Table II), the most commonly cited reasons for not getting an HIV test included: being too nervous to learn the results, being worried about the reaction of one’s sexual partner, being worried that people would think she was sick, and the distance needed to travel to the testing site.
The qualitative results also highlighted some of the aforementioned barriers and provided a more in-depth understanding as to how sex workers perceived barriers to getting tested for HIV. Time, distance, and money were major factors in these women’s lives. As one participant explained:
I repeat that it doesn’t happen that we have extra time. For example, since we are here [working the street] until late, and then we sleep, and then already back here again. Well, I am just being lazy not to go there [AIDS Center]. If it were just across the road, then of course it would have all been done long ago. But since it is so far to travel—well this is probably the problem. There is simply no money, and when there is, then some other kinds of issues come up.
Another woman described the situation as follows:
I would need to go to the doctor for those tests. If they learn that you are, for example, HIV-infected or something then they send you away. Can you imagine that I would have to go from here to the city center to give blood? To, who the hell knows where… to hell and beyond. And, such is the situation that you cannot be tested here in our district, not to mention here in our clinic. Such is the situation that we cannot test in our clinic. We cannot test in our district. They send you somewhere to the center of the city. Excuse me, but, I would have to waste two hours just to get there.
Barriers to going for an HIV test that were associated with injection drug use also came up in the in-depth interviews.
In order for me to go somewhere, well…First, my residence permit is not for this district, so I would have to specially go to the other end of the city. When you use drugs, you are not up to doing this. If the occasion presents, like the van came and there was an opportunity, then, I immediately tested for everything. I immediately checked for everything. But, it is rare to go somewhere specifically to get tested. It is nonsense to think that someone would specially go somewhere to get tested.
Like this woman discussed, other female sex workers talked about using the outreach van as an opportunity to get tested since traveling somewhere else for an HIV test was not realistic given other constraints in their lives. HIV testing was not routinely offered on the outreach vans, though there could be instances when oral, rapid HIV testing campaigns or research studies did happen; however, if someone were to test positive, she would need to be sent for confirmatory testing at a clinic. The time needed to travel as a barrier to getting services was especially true for women who lived in the suburbs and worked in the city.
A person could get tested at a private clinic closer to their home. However, not having the money to pay for an HIV test at a facility that is closer to home was also mentioned as a barrier to testing among participants.
You know, I simply haven’t tested in a really long time. It has not been possible. I paid for the test and that was a lot of money. Umm, I tested, I’ll tell you when. I tested three years ago.
Fear was also cited as a barrier to HIV testing. Many of the women talked about the fear of learning that they had HIV as a deterrent to getting tested. One participant described: ‘All the same it is scary. No matter how many times you get these tests, it is nonetheless scary.’ It was not only the fear of getting a positive test result, but what happens once you have that result on your record that was perceived as a barrier to getting tested. In response to the question of whether she had gone to the AIDS Center to be tested, one sex worker replied ‘No, I am afraid to go, to be registered.’ If a person tests positive, then she is officially registered at the AIDS Center and this information is included in her medical records.
There was confusion around the issue of treatment for HIV and feeling like one would not receive treatment or care was reported to be a barrier to testing. Moreover, feeling like nothing would change from knowing one’s HIV serostatus was cited as a reason not to get tested. One participant, who had not tested for HIV in over a year said:
If I have it [HIV], it is not going to go away. So why should I know about it? It is not like I give anyone my needle. I use condoms. I try not to infect anyone. Why get upset all over again? I don’t know- it doesn’t matter. You aren’t going to get rid of it.
Women, like the participant quoted above, who did not foresee being able to do anything about the HIV-infection, were not motivated to get tested.
Perceived benefits of testing
In the quantitative component, the most common reasons identified for getting tested for HIV were the desire to know one’s status and the ability to protect others (Table III).
The qualitative data supported these same reasons and also provided additional reasons that female sex workers felt it was important to get tested for HIV. Some of the participants talked about wanting to know for their own health. They talked about wanting to reassure themselves because they knew that they were at risk for HIV. As one participant described:
I get tested for myself first and foremost, since I am involved in this non-sense. I do this just for myself, actually, in order to know. Anything can just happen. I simply hear that girls are sick, and of course, I start worrying. It is better that I go get tested for everything.
One woman described how she thought learning her status earlier would result in a better outcome:
Why? Because I am a drug user, a prostitute…syphilis can be treated, but HIV, excuse me…It seems to me that the earlier I will know about it, the greater chance I have to live longer because I will know. I can, well for myself, well, how to say it exactly? I can control the process, take some kind of medicines.
Some participants talked about needing to know their status for other people in their lives, namely their children, but also their male partners. One participant explained why she tested for HIV: ‘I give blood [for analysis] every month because my child is young. Of course, I must know what is what and why it is so.’ Another participant described wanting to know her status to protect her husband if she were diagnosed with HIV. ‘I was also using, when he and I lived together. So I decided to get tested for myself and for him. And when I was working, then I tested for my own health.’
Many of the sex workers in the study reported not being motivated by a specific reason to test for HIV, but they recognized the value in getting the test and seized the opportunity when it was presented to them:
No, there were not any concrete reasons. I tested simply because. And even more so this type of work is so risky, so why not get tested. Moreover, it was convenient and free. I tested and went on my way.
Cues to action
Among surveyed participants, 93% said that they knew someone who had HIV. Nearly all of the women (94%) reported talking to someone about HIV. HIV was most commonly discussed with friends and peers, followed by discussions with doctors and social workers. Just over half of the sex workers had ever discussed HIV with their husbands or sexual partners. Participants were least likely to discuss HIV with their clients (44%). Eighty-seven percent (87%) of participants said that had received written materials about HIV. Most (94%) had heard of the City AIDS Center. Three-quarters of participants said that other PWID told them about visiting the AIDS Center, while just over half (58%) said that other sex workers had talked to them about receiving services at the AIDS Center.
The qualitative data also revealed that the sex workers were exposed to various types of information about HIV and HIV services—primarily printed brochures, but also referral slips from outreach workers. All of the women said that they felt they were exposed to information about HIV.
Yes, in my opinion, nowadays a person can go anywhere for a test. You can go where you pay for the test and it is anonymous… Moreover, there are advertisements everywhere. They show ads on television. That is, there are no secrets.
Participants also read booklets and used the Internet to get information about HIV.
The sex workers talked about knowing PLHIV, including relatives, friends, other sex workers, and other drug users. Some women said that they openly discussed the issue of HIV with other sex workers. ‘The girls even talk about it amongst themselves. We are here talking about it. Why hide something here? After all, we are not medical workers; it is not necessary to hide something from one another.’ However, not all participants were comfortable talking about HIV with other sex workers, and for the most part, they discussed HIV more among their peers in drug use than among their peers in sex work.
Women talked about deciding to get an HIV test because they found out someone they knew had HIV. For example, one sex worker told that, ‘My friend told me that she had HIV. When she first learned and then told me, I was, like, kind of in shock. I decided to get tested.’ Participants discussed their preference to get information about HIV from their peers them rather than from professionals. One participant talked about receiving information from other patients in the hospital.
Well, they [doctors] didn’t really discuss HIV. That is everything we learned was from booklets and from other patients in the hospital bed next to you who are ill. Probably you will learn more information from them than from doctors. Doctors don’t have time. Well that is, I learned more in the hospital from other patients.
Not all women talked about feeling comfortable talking about HIV--either their own status or the illness itself--with other sex workers, and in some cases with their family and friends.
Associations between health beliefs and recent HIV testing
Multivariable logistic regression was used to determine which factors were associated with having a recent HIV test. HIV-positive sex workers who were tested more than six months prior were not included in the analysis, resulting in a sample of 105. Among these female sex workers, 59% (n=62) reported being tested for HIV within the past six months. The multivariable logistic regression model is shown in Table IV.
Table IV.
Associations between individual-level factors and recent HIV testing (N=105)
| Factor | Unadjusted OR |
95% CI | p-value | Adjusted OR |
95% CI | p-value |
|---|---|---|---|---|---|---|
| Perceived susceptibility | 1.80 | (0.78, 4.13) | p=0.17 | 1.61 | (0.60, 4.35) | p=.35 |
| Perceived severity | 1.59 | (0.62, 4.10) | p=0.33 | 1.10 | (0.33, 3.60) | p=.88 |
| Perceived self-efficacy | 1.79 | (0.63, 5.08) | p=0.28 | 1.32 | (0.41, 4.24) | p=.63 |
| Perceived barrier: don’t feel at risk | 0.56 | (0.19, 1.67) | p=0.30 | 0.50 | (0.14, 1.83) | p=.29 |
| Perceived barrier: people will think I am sick | 0.54 | (0.24, 1.19) | p=0.13 | 0.48 | (0.19, 1.23) | p=.13 |
| Cue to action: know people with HIV | 5.83 | (1.15, 29.62) | p=0.03 | 6.75 | (1.11, 41.10) | p=.04 |
| Marital status | 0.90 | (0.41, 2.00) | p=0.80 | 1.16 | (0.45, 3.03) | p=0.76 |
| Place of residence | 1.54 | (0.53, 4.49) | p=0.43 | 1.59 | (0.42, 6.00) | p=0.50 |
| Amount of time using drugs | 0.39 | (0.15, 0.98) | p=.04 | 0.30 | (0.09, 0.97) | p=.01 |
| Amount of time involved in sex work | 0.38 | (0.16, 0.81) | p=.014 | 0.46 | (0.17, 1.20) | p=0.11 |
If a female sex worker reported knowing someone who has HIV then she was more likely to have had a recent HIV test [aOR=6.75, 95% CI (1.11, 41.10)]. The length of time using drugs was also significant, and the only demographic variable to be significant in the model. Female sex workers were 70% less likely to have had a recent HIV test if they had been using drugs for more than four years compared to those who had been using drugs for less than four years [aOR= 0.30, 95% CI (0.09, 0.97)]. The remaining theoretical constructs in the model were associated with HIV testing in the anticipated direction, but due to the wide confidence intervals these results were inconclusive.
Discussion
This study illustrated the application of a mixed-methods design to a theory-driven examination of factors influencing the uptake of HIV testing among a vulnerable population in Russia. The HBM was an important framework for beginning to understand motivators and barriers to HIV testing among street-based female sex workers. However, the constructs, measured as they have been in the past, may overlook important details and nuances in this population’s understanding of perceived severity, susceptibility, barriers, benefits, and self-efficacy and exposure to cues to action. The mixed-methods approach helped to further the understanding of how each of these constructs contributes to female sex workers’ health beliefs around HIV and influences getting an HIV test. In the future, it would be interesting to examine the motivators and barriers for HIV testing among other sex workers in Russia, including female sex workers in indoor settings, male sex workers, and sex workers in other locations in Russia, such as more provincial towns that are further from a larger metropolitan city where there are potentially less resources available for reaching sex workers with outreach services.
Our findings on the individual-level, health beliefs add to what other factors have been shown to influence HIV testing and linkage to HIV services for vulnerable populations in Russia. The history of ever having been tested for HIV was higher in the current sample than in a previous study among PWID in Russia (Niccolai et al., 2010). However, approximately half of the sex workers in our study had a recent HIV test, which according to these other studies would also be considered sub-optimal. HIV-related stigma is a documented problem in Russia (Balabanova et al., 2006). There are structural barriers within the healthcare system and society that marginalizes female sex workers from receiving care (King and Maman, 2013). Stigma and discrimination negatively affect HIV service utilization among female sex workers in Russia (King et al., 2013). Systemic barriers, including bureaucracy, lack of integration of HIV, tuberculosis and drug treatment services, and the provision of HIV treatment services conditional upon treated drug use, inhibit the utilization of HIV treatment services among PWID in Russia (Sarang, Rhodes, & Sheon, 2013). Among PLHIV in Russia, fear that others would learn about one’s HIV-positive serostatus was found to be a major barrier for engaging in care (Kelly et al., 2014). The findings from our study provide information focused on health beliefs, which may help in tailoring and improving upon public health programs to promote HIV testing for vulnerable populations.
The results of our study could be used to strengthen the design and implementation of public health programs to increase HIV testing among street-based female sex workers and to help address the critical gap in the number of diagnosed cases among the estimated number of PLHIV in Russia. The information on health beliefs could help frame the health promotion aspects of public health campaigns to increase HIV testing, such as discussions around susceptibility to HIV and repeat testing, focusing on self-efficacy for seeking a test, building off the perceived benefits of getting an HIV test, and addressing the barriers of fear of getting a positive HIV test result through education on the opportunities for treatment and care. However, it is important to note that addressing the barriers of time, distance and money would require an intervention beyond the individual-level health education activities. Participants talked about needing to travel to the clinics where HIV testing was offered, such as the St. Petersburg City AIDS Center, S. P. Botkin City Infectious Disease Hospital, or sexually transmitted disease clinic. The City AIDS Center and Botkin Hospital are centrally located in a large, cosmopolitan city of over five million inhabitants. A fee-based (anonymous) test at the City AIDS Center is 14 rubles (at the time of data collection, $0.60), which is the cost of the testing kit; and, an additional 190 rubles for a written certificate of the test results (City AIDS Center, 2009).
One recommendation is to expand anonymous voluntary counseling and testing opportunities, including furthering opportunities to integrate HIV testing into outreach activities. Decker et al. (2014) argue for the continuation and expansion of targeted programs for female sex workers based on their evaluation that these targeted outreach and clinical services were effective at improving uptake of HIV testing in Kazan, Krasnoyarsk and Tomsk, Russia. Our findings add further support for this argument, as outreach services were an important means to help break down some of the barriers to HIV testing for street-based female sex workers. The importance of mobile, outreach services for uptake of HIV testing has also recently been shown to be effective with sex workers in other settings, such as in Canada (Deering et al, 2015). Our study findings suggest the importance of peers in both getting information about HIV and getting tested for HIV, highlighting an opportunity for intervention design. Previous studies have focused on this approach. For example, research in east and southern Africa also indicated the need for sex worker-led peer outreach work as an important way to reach sex workers with HIV prevention activities and improve access to services (Scorgie et al., 2013).
Our research should be considered in light of its limitations. First, the cross-sectional study results did not allow casual inferences to be made. Our study was limited by the sample size for exploring alternative considerations of the relationships between the HBM constructs, such as the idea that the influence of cues to action on the uptake of HIV testing may be mediated by perceived threat. Future research studies could expand upon our initial descriptive study. Second, this study did not include sex workers who are not connected to outreach services. Sex workers who are not receiving outreach research services may be different than sex workers who are receiving these services. Nonetheless, the fact that the research was community-based rather than clinic-based allowed for the inclusion of women who were not getting HIV services at clinics. Third, the self-reported data were subject to social desirability bias. Ensuring anonymity in responses may have helped to reduce this bias; and also the qualitative data helped to elucidate the results from the questionnaires. Despite these limitations, our study was a significant undertaking in reaching street-based female sex workers that may or may not have accessed HIV testing services in a clinic. The researchers were not part of any HIV testing or outreach services. Given that the PI was conducting interviews as a visiting foreign scholar, she distinguished herself as separate from a service provider or representative of any clinical setting, but rather positioned as an outside researcher trying to better understand barriers and motivators for HIV testing among street-based sex workers in St. Petersburg.
These results highlighted how quantitative and qualitative findings, and especially the ‘integration of qualitative and quantitative research’ (Bryman, 2007) contributed to a more nuanced understanding of health beliefs. The confirmation and discrepancies between the qualitative and quantitative findings improved the interpretation of the results for each of the constructs of the HBM. For the specific area of interest of this study, the information learned about risk perceptions, perceived barriers and benefits, self-efficacy, and cues to action should be considered in developing interventions to improve the uptake of HIV testing among street-based female sex workers in Russia.
Acknowledgments
Funding
This work was supported by a Fulbright-Hays Doctoral Dissertation Research Abroad Award; a Travel Award from The Gillings School of Global Public Health at the University of North Carolina at Chapel Hill; a Royster’s Society of Fellows Doctoral Dissertation Completion Fellowship at the University of North Carolina at Chapel Hill; and a Postdoctoral Training Grant at Yale University’s Center for Interdisciplinary Research on AIDS from the National Institute of Mental Health [grant number T32MH020031]. The content of the manuscript is solely the responsibility of the authors and does not necessarily represent the views of the funding agencies.
References
- Balabanova Y, Coker R, Atun RA, & Drobniewski F (2006). Stigma and HIV infection in Russia. AIDS Care, 18(7), 846–852. [DOI] [PubMed] [Google Scholar]
- Beattie TS, Bhattacharjee P, Suresh M, Isac S, Ramesh BM, & Moses S (2012). Personal, interpersonal and structural challenges to accessing HIV testing, treatment and care services among female sex workers, men who have sex with men and transgenders in Karnataka state, South India. J Epidemiology Community Health, 66(Suppl.2), ii42–48. doi: 10.1136/jech-2011-200475 [DOI] [PubMed] [Google Scholar]
- Benotsch EG, Somlai AM, Pinkerton SD, Kelly JA, Ostrovski D, Gore-Felton C, & Kozlov AP (2004). Drug use and sexual risk behaviours among female Russian IDU who exchange sex for drugs and money. International Journal of STD & AIDS, 15(5), 343–347. [DOI] [PubMed] [Google Scholar]
- Brown EJ, & Van Hook M (2006). Risk behavior, perceptions of HIV risk, and risk-reduction behavior among a small group of rural African American women who use drugs. Journal of the Association of Nurses in AIDS Care, 17(5), 42–50. [DOI] [PubMed] [Google Scholar]
- Bryman A (2007). Barriers to integrating quantitative and qualitative research. Journal of Mixed Methods Research, 1(1), 8–22. [Google Scholar]
- City AIDS Center (St. Petersburg Center for the Prevention of and Fight Against AIDS and Infection Diseases). (2009). Information for those who want to get tested for HIV, hepatitis A, B, C, or syphilis. Retrieved from http://stop-spid.ru/spid.html.
- Creswell J (2003). Research design: Qualitative, quantitative, and mixed methods approaches (2nd ed.). Thousand Oaks, CA: Sage Publication. [Google Scholar]
- de Paoli MM, Manongi R, & Klepp KI (2004). Factors influencing acceptability of voluntary counselling and HIV-testing among pregnant women in northern Tanzania. AIDS Care, 16(4), 411–425. [DOI] [PubMed] [Google Scholar]
- Decker MR, Wirtz A, Moguilnyi V, Peryshkina A, Ostrovskaya M, Nikita M, … Beyrer C (2014). Female sex workers in three cities in Russia: HIV prevalence, risk factors and experience with targeted HIV prevention. AIDS and Behavior, 18, 562–572. doi:0.1007/s10461-013-0577-y. [DOI] [PubMed] [Google Scholar]
- Deering KN, Montaner JS, Chettiar J, Jia J, Ogilvie G, Buchner C, …Shannon K (2015). Successes and gaps in uptake of regular, voluntary HIV testing for hidden street- and off-street sex workers in Vancouver, Canada. AIDS Care, 27(4), 499–506. doi: 10.1080/09540121.2014.978730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal AIDS Center of the Russian Federation. (2014). Fact sheet: HIV-infection in the Russian Federation on November 1, 2014 [in Russian]. Retrieved from http://www.hivrussia.org/doc/docs.shtml
- Genberg BL, Hlavka Z, Konda KA, Maman S, Chariyalertsak S, Chingono A, … Celentano DD (2009). A comparison of HIV/AIDS-related stigma in four countries: Negative attitudes and perceived acts of discrimination towards people living with HIV/AIDS. Social Science & Medicine (1982), 68(12), 2279–2287. doi: 10.1016/j.socscimed.2009.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grau LE, White E, Niccolai LM, Toussova OV, Verevochkin SV, Kozlov AP, & Heimer R (2011). HIV disclosure, condom use, and awareness of HIV infection among HIV-positive, heterosexual drug injectors in St. Petersburg, Russian Federation. AIDS and Behavior, 15(1), 45–57. doi: 10.1007/s10461-010-9775-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HHS: U.S. Department of Health and Human Services. (2014). HIV testing frequency. Retrieved from: https://www.aids.gov/hiv-aids-basics/prevention/hiv-testing/hiv-testing-frequency/.
- Kelly J, Amirkhanian Y, Yakovlev A, Musatov V, Meylakhs A, Kuznetsova A, & Chaika N (2014). Stigma reduces and social support increases engagement in medical care among persons with HIV infection in St. Petersburg, Russia. Journal of the International AIDS Society, 17(4 Suppl 3), 19618. doi: 10.7448/IAS.17.4.19618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerrigan D, Wirtz A, Baral S, Decker M, Murray L, Poteat T, … Beyrer C (2013). The global HIV epidemics among sex workers. Washington, D.C.: World Bank. [Google Scholar]
- King EJ, & Maman S (2013). Structural barriers to receiving health care services for female sex workers in Russia. Qualitative Health Research, 23(6), 1079–1088. doi: 10.1177/1049732313494854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King EJ, Maman S, Bowling JM, Moracco KE, & Dudina V (2013). The influence of stigma and discrimination on female sex workers’ access to HIV services in St. Petersburg, Russia. AIDS Behavior, 17(8), 2597–2603. doi: 10.1007/s10461-013-0447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozlov AP, Shaboltas AV, Toussova OV, Verevochkin SV, Masse BR, Perdue T, …Hoffman IF (2006). HIV incidence and factors associated with HIV acquisition among injection drug users in St. Petersburg, Russia. AIDS, 20(6), 901–906. [DOI] [PubMed] [Google Scholar]
- Lux K, & Petosa R (1995). Using the HBM to predict safer sex intentions of incarcerated youth. Health Education Quarterly, 22(1), 487–497. [DOI] [PubMed] [Google Scholar]
- Maguen S, Armistead LP, & Kalichman S (2000). Predictors of HIV antibody testing among Gay, Lesbian, and bisexual youth. Journal of Adolescent Health, 26(4), 252–257. [DOI] [PubMed] [Google Scholar]
- Maman S, Mbwambo J, Hogan NM, Kilonzo GP, & Sweat M (201). Women’s barriers to HIV-1 testing and disclosure: Challenges for HIV-1 voluntary counselling and testing. AIDS Care, 13(5), 595–603. [DOI] [PubMed] [Google Scholar]
- Niccolai LM, Toussova OV, Verevochkin SV, Barbour R, Heimer R, & Kozlov AP (2010). High HIV prevalence, suboptimal HIV testing, and low knowledge of HIV-positive serostatus among injection drug users in St. Petersburg, Russia. AIDS Behavior, 14(4), 932–941. doi: 10.1007/s10461-008-9469-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokrovskaya A, Popova A, Ladnaya N, & Yurin O (2014). The cascade of HIV care in Russia, 2011–2013. Journal of the International AIDS Society, 17(4 Suppl 3), 19506. doi: 10.7448/IAS.17.4.19506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock IM (1966). Why people use health services. The Millbank Memorial Fund Quarterly, 44, 94–127. [PubMed] [Google Scholar]
- Sarang A, Rhodes T, & Sheon N (2013). Systemic barriers accessing HIV treatment among people who inject drugs in Russia: A qualitative study. Health Policy Plan, 28(7), 681–691. doi: 10.1093/heapol/czs107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scorgie F, Nakato D, Harper E, Richter M, Maseko S, Nare P, … Chersich M (2013). ‘We are despised in the hospitals’: Sex workers’ experiences of accessing health care in four African countries. Culture, Health & Sexuality, 15(4), 450–465. doi: 10.1080/13691058.2012.763187. [DOI] [PubMed] [Google Scholar]
- Shahrabani S, & Benzion U (2012). How experience shapes health beliefs: The case of influenza vaccination. Health Education Behavior, 39(5), 612–619. doi: 10.1177/1090198111427411 [DOI] [PubMed] [Google Scholar]
- Shannon K, Strathdee SA, Goldenberg SM, Duff P, Mwangi P, Rusakova M, …Boily MC (2015). Global epidemiology of HIV among female sex workers: Influence of structural determinants. Lancet, 385(9962), 55–71. doi: 10.1016/S0140-6736(14)60931-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeer W, Bos AE, Mbwambo J, Kaaya S, & Schaalma HP (2008). Social and cognitive variables predicting voluntary HIV counseling and testing among Tanzanian medical students. Patient Education and Counseling, 75(1), 135–140. doi: 10.1016/j.pec.2008.08.022. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2004). HIV-related sentinel surveillance among risky populations in the Republic of Azerbaijan, Republic of Moldova and the Russian Federation. Retrieved from http://www.euro.who.int/Document/E84675.pdf.