Abstract
Bronchial anthracofibrosis (BAF), caused by long-standing exposure to biomass fuel smoke, has emerged as a distinct pulmonary disease. It is usually seen in elderly females who have worked long hours in poorly ventilated kitchen full of smoke due to incomplete combustion of biomass fuel. The diagnosis is confirmed on bronchoscopic visualization of bluish-black anthracotic pigmentation along with narrowing/distortion of the affected bronchus. BAF has been associated with clinical conditions such as pulmonary tuberculosis, chronic obstructive pulmonary disease, pneumonia, and malignancy. Tuberculosis, once thought to be the causative agent for BAF, is now considered to be an association. BAF has a diverse radiological presentation and the presence of associated clinical conditions often confound the radiological picture. The imaging features of BAF include primary imaging characteristics, which pertains to the disease entity directly, and secondary features based on the presence of associated conditions. High-resolution computed tomography findings of multifocal bronchial narrowing and peribronchial cuffing are considered to be specific diagnostic features of BAF. In addition, the diagnostic probability is increased in the presence of mediastinal adenopathy and collapse/atelectasis with middle lobe syndrome being the most common presentation. This pictorial essay highlights the range of imaging appearances in patients with BAF.
Keywords: Anthracosis, biomass fuel smoke exposure, bronchial anthracofibrosis, fiberoptic bronchoscopy, high-resolution computed tomography, imaging
Introduction
Bronchial anthracofibrosis (BAF), highlighted less than two decades ago, is a pulmonary disease caused by long-standing exposure to biomass fuel smoke.[1] Nearly half the world's population depends on biomass fuel for cooking and heating.[2] In India too, it is estimated by the World Health Organization[3] that 58% of the public still uses this medium for cooking. BAF is mostly seen in elderly ladies who have spent long hours cooking on wood-fire while exposed to dense smoke in poorly ventilated kitchens.[1,4,5]
Historical Perspective
“Bronchial anthracosis,” a term coined by Pearson[6] in 1813, refers to bluish-black discoloration of bronchial mucosa [Figure 1A] caused due to soot inhalation. The term BAF was popularized by Chung et al.[5] in 1998 when on bronchoscopy they recognized bronchial anthracosis accompanied with narrowing/distortion of the associated bronchi [Figure 1B]. However, it was Abraham Cohen[7] who, in 1951, first documented the occurrence of bluish-black pigmentation with narrowing of airways when he described middle lobe narrowing in eight females due to perforated tuberculous lymph nodes, six of whom had anthracotic pigmentation. Chung et al.[5] described bronchoscopically confirmed BAF in 28 patients, 20 of whom were females. Active tuberculosis was seen in 17 of 28 patients while empirical anti-tuberculous therapy was initiated in 5 of the remaining 11 patients, of whom 3 had definite radiological improvement. This led the authors to hypothesize that tuberculosis was responsible for the occurrence of BAF. However, there is now a mounting body of evidence to incriminate long-standing exposure to the smoke generated by incomplete combustion of biomass fuel in poorly ventilated kitchens as the causative factor.[8,9,10]
Figure 1 (A and B).
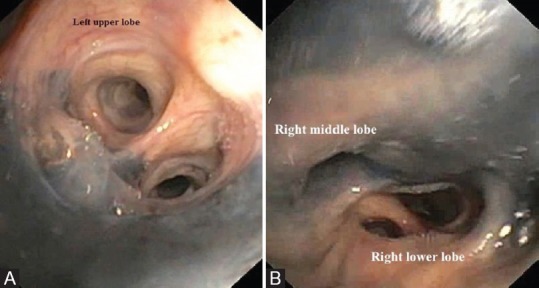
(A) Fiberoptic bronchoscopic (FOB) image showing bluish-black anthracotic pigmentation of the mucosa of the left upper lobe bronchus in a 62-year-old female with 20 years of biomass fuel smoke exposure. (B) FOB image showing bluish-black anthracotic pigmentation of the mucosa of the right middle lobe bronchus along with narrowing/distortion of the bronchus suggestive of bronchial anthracofibrosis (BAF) in a 82-year-old female with 40 years history of biomass fuel smoke exposure
BAF was first reported from India in a 65-year-old female who presented with middle lobe syndrome (MLS) and had long-standing history of wood-smoke exposure.[11] High-resolution computed tomography (HRCT) revealed multifocal narrowing of the right middle lobe bronchus. Fiberoptic bronchoscopic (FOB) done to evaluate MLS visualized bluish-black pigmentation along with narrowing and distortion of the middle lobe bronchus confirmatory of BAF. The bronchial aspirate in this patient cultured Mycobacterium tuberculosis.
Diagnostic Criteria
On FOB, the presence of bluish-black mucosal pigmentation, normal shape and opening of the bronchi with no evidence of narrowing or distortion of the bronchi is suggestive of bronchial anthracosis [Figure 1A]. In contrast, in patients with BAF [Figure 1B], the pigmentation visualized on FOB subjectively appears to be more dense and is always combined with narrowing/distortion of the associated bronchus. The differences between the two entities are summarized in Table 1. The diagnostic criteria for BAF adopted by us as well as several other authors[1,4,5,8,9,10] include: (1) long-standing history of biomass fuel smoke exposure, (2) multifocal bronchial narrowing on HRCT when present, and (3) confirmed on bronchoscopy by visualization of (a) bluish-black mucosal anthracotic pigmentation along with (b) narrowing/distortion of the affected bronchus.
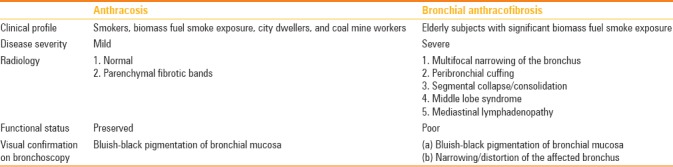
Table 1.
Differences between anthracosis and bronchial anthracofibrosis
Radiological Features
Although BAF is a bronchoscopic diagnosis, imaging often provides the initial diagnostic clue as this clinical entity has diverse but characteristic radiological manifestations.[10,12,13] The radiological findings in BAF comprise primary imaging features per se due to BAF itself while secondary imaging characteristics are due to the presence of associated disease conditions.
Radiological features such as multifocal bronchial narrowing and peribronchial cuffing are characteristic of BAF and can be considered as primary imaging features, while collapse, consolidation, and mass lesions could be due to associated conditions.[10,13] The associated clinical conditions such as pulmonary tuberculosis, chronic obstructive pulmonary disease (COPD), pneumonia, and malignancy contribute to the radiological picture.[1] Although studies on BAF[9,12,13] have included radiological aspects, however, a detailed description of the imaging pattern in patients with BAF is yet to receive the attention that it deserves. This pictorial essay highlights the spectrum of radiological appearances of BAF.
Airway involvement
Multifocal bronchial narrowing
This characteristic feature, when seen on HRCT, is often considered to be the diagnostic hallmark of BAF.[1,5,10,11] Bronchial narrowing [Figure 2] in patients with BAF tends to be multifocal in nature and usually involves right middle and upper lobe bronchi. BAF affects the segmental or lobar bronchi with sparing of trachea and the main bronchus in most of the patients. This is in stark contrast with pattern of bronchostenosis seen in endobronchial tuberculosis where the main and lobar bronchi are involved in a contiguous fashion. Pigmentary deposits in BAF are usually encountered at the branching points within the tracheobronchial tree and are followed by inflammatory response and bronchial stenosis.[13,14] A CT-based study in 58 patients with BAF reported multifocal bronchial stenosis in 23 (39.7%) with right middle lobe bronchus being most commonly affected.[13] In a recent prospective study from India, of the 80 patients with long-standing history of exposure to biomass fuel smoke, 60 consented to undergo FOB, 24 (40%) of whom were diagnosed with BAF, 17 (28.3%) had bronchial anthracosis only, while 19 (31.7%) had normal bronchial tree appearance. Five (20.8%) of the 24 patients with BAF had multifocal bronchial narrowing on HRCT.[10] All 60 patients evaluated by Pilaniya et al.[10] happened to be females.
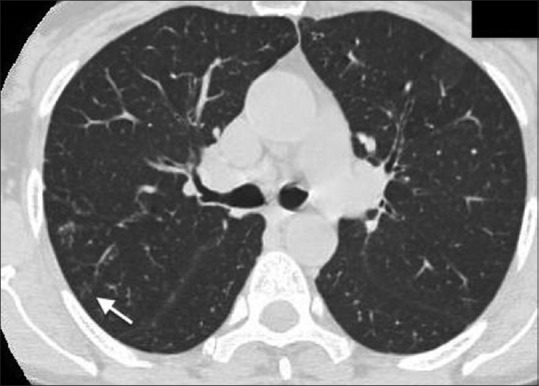
Figure 2.

High-resolution computed tomography (HRCT) of chest (lung window) showing multifocal narrowing of the left upper lobe bronchus (white arrow) in a 75-year-old female with long-standing biomass fuel smoke exposure. FOB confirmed BAF involving left upper lobe bronchus
Peribronchial cuffing
Peribronchial soft-tissue thickening/cuffing [Figure 3] on HRCT, in an appropriate setting, can raise suspicions of BAF.[13] However, this radiological feature is also thought to be suggestive of pulmonary sarcoidosis.[15] Kahkouee et al.[13] have suggested that this feature occurs due to “the encroachment of anthracotic deposits on airways, even in the absence of apparent tuberculosis or other lung diseases, which may produce central peribronchial soft tissue thickening or intraparenchymal peribronchial cuffing.” Furthermore, this may lead to the development of bronchial narrowing or lobar/segmental atelectasis. Chung et al.[5] had reported peribronchial cuffing on CT chest in 24 of 28 patients with BAF. In a series of 333 patients with BAF from Korea,[9] peribronchial cuffing was present in 80% while a study from Iran[13] documented it in 37 of 58 (63.1%) patients. In contrast, only 5 of the 24 patients with BAF from India had peribronchial soft tissue cuffing.[10]
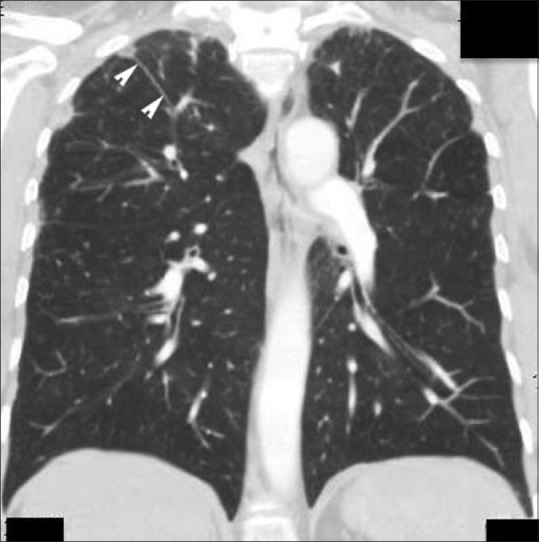
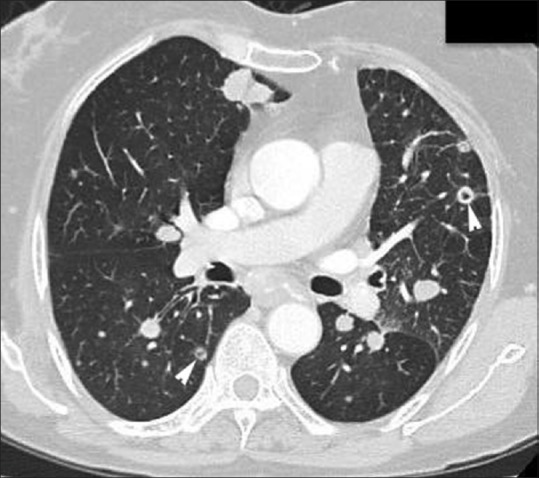
Figure 3.

HRCT of the chest (lung window) showing peribronchial cuffing of right upper lobe bronchus (white arrow) in a 62-year-old female diagnosed with BAF
Bronchiectasis
Bronchiectasis on HRCT [Figure 4] is not an uncommon finding in patients with BAF. Biomass fuel smoke acts as a chronic irritant in the airways. This leads to chronic airway inflammation, goblet cell hypertrophy, and mucous production. In addition, impairment of mucociliary escalator mechanism occurs due to exposure to biomass fuel smoke.[16] All these factors predispose to the development of bronchiectasis in patients with biomass fuel smoke exposure leading to BAF. In an earlier study from Korea,[12] bronchiectasis was reported in 30% of patients, while a study from Iran[13] documented it in 24 of 58 (41.3%) patients. Of the 58 patients, multilobar bronchiectasis was seen in nine (15.5%) with the lingula being most commonly affected.[13] Three of the 24 patients from India with BAF had bronchiectasis on HRCT.[10]
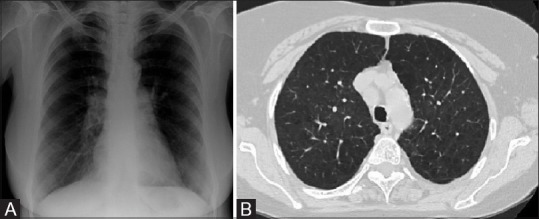
Figure 4 (A and B).
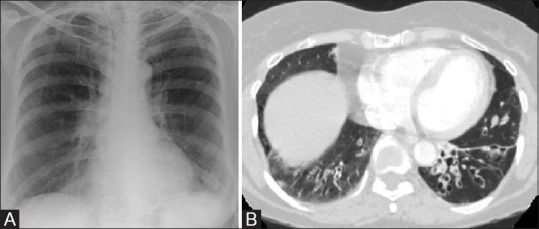
(A) Chest radiograph (PA view) in a 58-year-old female with BAF showing crowding of bronchovascular markings in bilateral lower zones and cystic shadows in left lower zone. (B) HRCT of chest (lung window) of the same patient showing bilateral lower lobe fusiform bronchiectasis (more in left lower lobe when compared with right) with thick fibrotic bands in the left lower lobe
Parenchymal involvement
Collapse
Lobar or segmental collapse is a common radiological finding in patients with BAF. Collapse may be due to bronchostenosis/obstruction or extrinsic compression of the affected bronchi. Although all lobes can be involved, the right middle lobe is most commonly affected and often presents as an MLS [Figure 5]. This striking radiological presentation raises the suspicion of BAF in an appropriate clinical setting.[1,10] Right upper lobe collapse is not infrequently seen. Lobar or segmental collapse is usually evident on chest radiograph with characteristic radiological signs [Figure 6]. Although the Golden S sign is classically described in patients with bronchial carcinoma, it can also occur due to metastasis, primary mediastinal tumor, or enlarged lymph nodes. In patients with BAF, Golden S sign can occur either due to bronchial stenosis and complete obstruction or extrinsic compression by enlarged lymph nodes.[17] However, distinct anatomical characterization of lobar/segmental collapse is possible on HRCT chest. In an earlier study on CT features in patients with BAF, segmental collapse distal to the “smoothly narrowed bronchus” was the most common finding.[12] Lobar/segmental collapse usually raises a suspicion of malignancy in these patients as BAF with concomitant adenocarcinoma has also been reported [Figure 7]. It is imperative for the pulmonologists/radiologists to exclude malignancy and/or pulmonary tuberculosis in those patients who present with a visible collapse on imaging.[18] In the recent prospective series of 24 patients with BAF, segmental collapse was seen in 13 patients.[10]
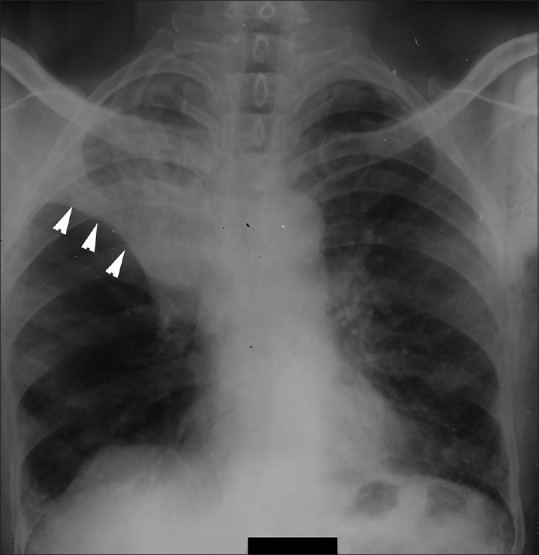
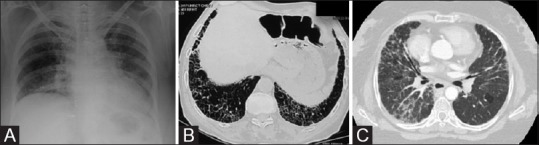
Figure 5 (A-C).
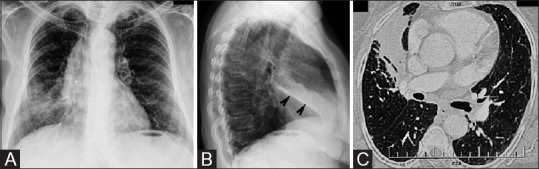
(A) Chest radiograph (PA view) in a 54-year-old female with 30 years history of biomass fuel smoke exposure showing an ill-defined opacity in the right lower zone abutting the right cardiac margin suggestive of middle lobe syndrome (MLS). (B) Chest radiograph (lateral view) of the same patient showing a wedge-shaped opacity (black arrowheads) extending in an anteroinferior direction from the hilum to the anterior chest wall suggestive of MLS. (C) HRCT of chest (lung window) showing a trapezoidal opacity with its base toward hilum and contiguous with the right cardiac border confirming the presence of MLS. FOB revealed anthracofibrosis of right middle lobe and bronchial aspirate cultured Mycobacterium tuberculosis
Figure 6.
Chest radiograph showing the characteristic golden S sign (white arrowheads) suggestive of collapse of right upper lobe in a 65-year-old female. FOB confirmed BAF of right upper lobe associated with tuberculosis
Figure 7.

HRCT of chest showing segmental collapse of right middle and lower lobe bronchi (white arrowheads) along with mass-like lesion in left lower lobe (black arrow) in a 62-year-old female with BAF involving right upper and middle lobes and left lower lobe. Transbronchial biopsy confirmed adenocarcinoma
The right middle lobe syndrome
MLS still continues to fascinate clinicians with its characteristic radiological presentation. It has been postulated that middle lobe is prone to recurrent collapse due to (a) lack of collateral ventilation leading to its anatomical isolation, (b) sharp angular take-off of the middle lobe bronchus, and (c) extrinsic compression by enlarged lymph nodes. Impaction of carbon particles present in the smoke occurs at the site of bronchial bifurcation especially around right middle lobe orifice leading to anthracotic pigmentation. Subsequently, inflammatory response results in fibrosis and stenosis of the affected bronchus.[10,11]
The index case of BAF in India,[11] a 65-year-old female with concomitant pulmonary tuberculosis, too presented radiologically as MLS. On chest radiograph, MLS appears as an ill-defined opacity in the right middle and lower zones with loss of cardiac silhouette on posteroanterior view [Figure 5A], while on the lateral view, it is visualized as a wedge-shaped opacity extending anteroinferiorly from the hilum [Figure 5B]. The diagnosis of MLS is confirmed on HRCT chest [Figure 5C].[19] Six (25%) of our 24 patients with BAF presented as an MLS on chest imaging.[13]
Consolidation
Consolidation, visible on chest radiograph, is not an uncommon finding in patients with BAF. This clinical entity is associated with pneumonia in nearly one-fourth of patients and consolidation in BAF is usually due to associated pneumonia.[1] BAF is characterized by the presence of bronchial narrowing and a majority of consolidations are seen in lobes having bronchial narrowing. The structural abnormality of the bronchus is the major predisposing factor for the development of pneumonia in patients with BAF.[1] Consolidation can be either lobar in nature [Figure 8] or multilobar involving multiple lobes [Figure 9]. The presence of consolidation with air bronchograms in patients with BAF usually points toward a diagnosis of associated pneumonia [Figure 10] or tuberculosis. In a study from Iran,[13] consolidation on HRCT chest was seen among 32 of 58 (55.2%) patients with BAF with right middle lobe being most commonly involved. Multilobar consolidation was seen in 12 of 32 (37.5%) patients.[13] The index case of BAF reported from India[11] too had consolidation of the right middle lobe along with air bronchogram. Consolidation seen on HRCT was observed in 13 of 24 (54.2%) patients with BAF.[10]
Figure 8.
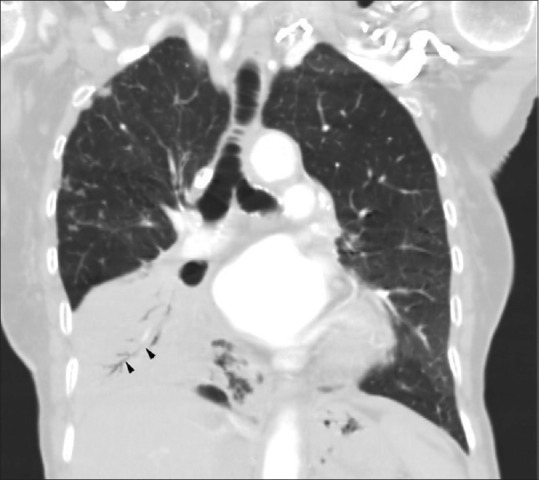
HRCT of chest (lung window, coronal view) showing lobar consolidation with air bronchogram (black arrowheads) involving right lower lobe in a 70-year-old female. FOB confirmed the diagnosis to be BAF
Figure 9.

HRCT of chest (lung window) showing multilobar consolidation in bilateral lower lobes with air bronchogram (black arrow). Visualization on FOB confirmed the presence of BAF in the right upper and middle lobe bronchi. Bronchial aspirate cultured M. tuberculosis while transbronchial biopsy was suggestive of caseating granulomas
Figure 10.
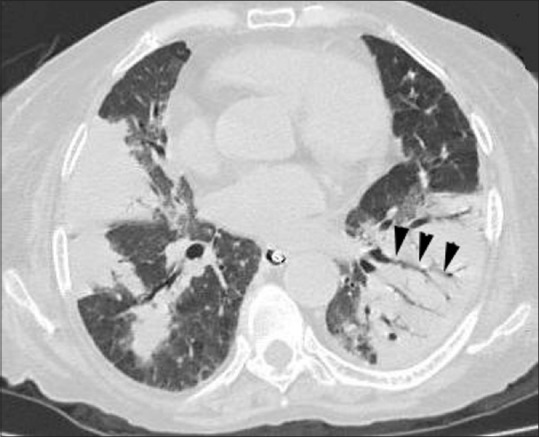
HRCT of chest (lung window) in a 66-year-old female showing consolidation in bilateral lower lobe with presence of air bronchograms (black arowheads). FOB visualized BAF involving right upper and both lower lobe bronchi while bronchial aspirate cultured Pseudomonas aeroginosa
Mass lesion
Usually most mass lesions in patients with BAF tend to be benign; however, all efforts must be made to rule out malignancy in these patients. CT-guided transthoracic biopsy and FOB are the most common modalities used to establish a diagnosis in patients with BAF and associated mass lesion. The presence of irregular margins, spiculations, and cavitation increases the possibility of malignancy [Figure 11]. Compared with other parenchymal opacities, mass lesions are a less common HRCT finding and have been documented in 7 of 27 patients with BAF from Iran.[13] Mass lesions associated with cavitation were seen in 3 of our 24 (12.5%) patients with BAF. Adenocarcinoma was confirmed in two of these patients.[10]
Figure 11.
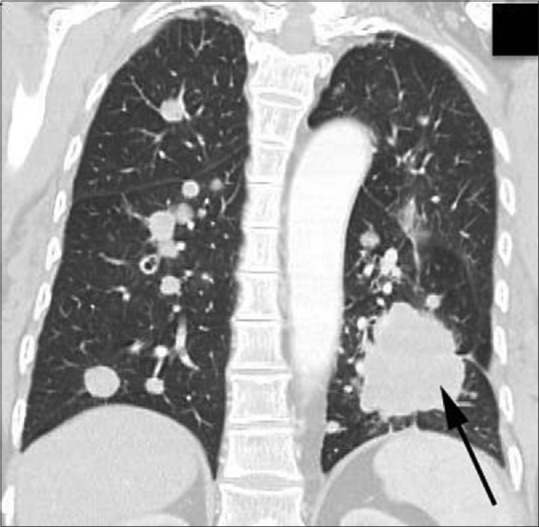
HRCT of chest (lung window, coronal view) in an 80-year-old female with BAF showing multiple discrete nodules involving right upper lobe and both lower lobes along with a mass lesion with irregular margins in left lower lobe (black arrow). Transbronchial biopsy from left lower lobe was suggestive of adenocarcinoma
Parenchymal fibrotic bands
Parenchymal fibrotic bands on HRCT are not uncommon in patients with BAF. These appear as linear opacities about 1–3 mm in thickness and usually extending up to the visceral pleura [Figure 12]. It represents pleuroparenchymal fibrosis and has been documented in nearly 53% of patients with BAF.[13] These bands represent areas of fibrosis caused due to exposure to biomass fuel smoke. This leads to activation of pulmonary fibroblasts and an increased production of fibronectin, and thus pleuroparenchymal fibrosis ensues. Parenchymal bands on HRCT were observed in 11 of the 24 (45.8%) patients with BAF.[10]
Figure 12.
HRCT of chest (lung window, coronal view) in a 56-year-old female with BAF showing a curvilinear fibrotic opacity in the right upper lobe extending peripherally upto the pleura (white arrowheads) suggestive of parenchymal fibrotic bands
Emphysema
Biomass fuel smoke exposure is a risk factor for development of both COPD and BAF.[1] Emphysema, both centrilobular and paraseptal [Figure 13], is often seen on HRCT in these patients. The presence of emphysema usually indicates coexistence of COPD as an associated condition. In a series of 333 patients with BAF from Korea, COPD was seen in 56 (16.8%) patients.[9] On HRCT, emphysema was detected in 4 (16.7%) of our 24 patients.[10]
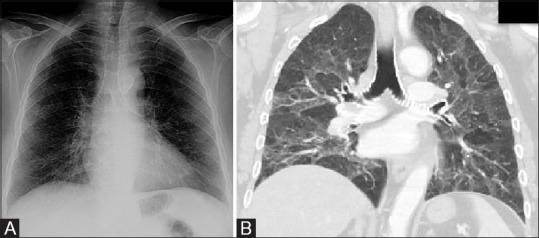
Figure 13 (A and B).
(A) Chest radiograph (PA view) in a 62-year-old female with 30 years history of biomass fuel smoke exposure and BAF showing bilateral hyperinflated lung fields. (B) HRCT of chest (lung window) of the same patient showing bilateral areas of centrilobular and paraseptal emphysema with upper lobe predominance. In addition, she was diagnosed with chronic obstructive pulmonary disease
Interstitial pattern
Interstitial involvement in patients with BAF manifests as nodular or reticulonodular opacities on chest radiograph [Figure 14A]. BAF associated with interstitial lung disease has previously been reported in literature with four reports documenting seven patients,[20,21,22,23] three of whom were reported from India.[22,23] In a Korean study[20] of 114 patients with BAF, 1 patient had a usual interstitial pneumonia (UIP) pattern; while in a Turkish study,[21] of the 27 patients with BAF, the authors documented the presence of an “interstitial pattern” on chest CT in three patients, but detailed imaging description was not mentioned. The studies from India reported UIP pattern [Figure 14B] in one patient; while in another two patients, a non-specific interstitial pneumonia pattern was seen [Figure 14C].[24]
Figure 14 (A-C).
(A) Chest radiograph (PA view) showing bilateral basilar reticulonodular opacities along with evidence of volume loss and cardiomegaly in a 76-year-old female who presented with exertional dyspnoea. FOB revealed BAF. (B) HRCT of chest (lung window) in a 76-year-old male with biomass fuel smoke exposure showing extensive bilateral basal honeycombing, reticulations, and subpleural fine fibrosis suggestive of usual interstitial pneumonia pattern. FOB revealed BAF. (C) HRCT of chest (lung window) of a 65-year-old female showing bilateral areas of ground-glass opacities along with interlobular septal thickening, peribronchial cuffing, and traction bronchiectasis in right lower lobe suggestive of non-specific interstitial pneumonia pattern. Right upper lobe BAF was visualized on FOB
Ground-glass, mosaic appearance, and nodules
On HRCT, patients with BAF may present with ground-glass opacities [Figure 15A and B], mosaic appearance [Figure 15B], micro- and macronodules as well as tree-in-bud opacities [Figure 16]. Exposure to biomass fuel smoke is a risk factor for bronchiolitis in these patients, which manifests radiologically as centrilobular nodules as well as mosaic appearance. These represent inflammatory changes, small airways obstruction, and areas of air trapping.[16] In addition, solitary and multiple nodules too may be seen on HRCT. Cavitating nodules [Figure 17], when present, usually point toward a diagnosis of malignancy. In a study from Iran,[13] mosaic appearance was seen in 21 of 58 (36.2%) patients on HRCT. In the same study, solitary and multiple pulmonary nodules were less commonly reported in 11 of 58 and 8 of 58 patients, respectively. In a series of 24 patients from India by Pilaniya et al.,[10] mosaic attenuation was documented in 5, while nodular lesions and tree-in-bud opacities were present in 1 patient each.
Figure 15 (A and B).
(A) Chest radiograph (PA view) showing bilateral basilar reticulonodular opacities in a 68-year-old female with a 50-year history of biomass fuel smoke exposure. In addition, extensive calcification of the tracheal wall is also noted. (B) HRCT of chest (lung window) of the same patient showing extensive ground glass opacities and mosaic appearance consistent with small airway narrowing suggestive of bronchiolitis along with extensive calcification of the tracheal wall
Figure 16.
HRCT in a 58-year-old male showing centrilobular nodules and “tree-in-bud” opacities in posterior segment of right upper lobe (white arrow). Along with BAF, FOB visualized caseous material in right upper lobe bronchus suggestive of endobronchial tuberculosis
Figure 17.
HRCT of chest (lung window) in an 80-year-old female BAF showing multiple discrete nodules involving right upper and both lower lobes with cavitation (white arrowheads). Transbronchial biopsy confirmed diagnosis to be of adenocarcinoma, while FOB suggested anthracofibrosis in left upper lobe
Mediastinal adenopathy
BAF can at times present with mediastinal lymphadenopathy on HRCT chest.[9,12,13] Enlarged mediastinal lymph nodes may develop calcification within them [Figure 18]. The presence of heterogeneous density (necrotic material) within enlarged lymph nodes usually suggests tuberculosis. These lymph nodes can cause extrinsic bronchial compression leading to lobar/segmental atelectasis.[1,5,12] In addition, these can erode into the bronchus and subsequently lead to bronchostenosis.[5,12] In a study from Korea, enlarged lymph nodes were seen in 166 of 252 (66%) patients, of whom 112 had calcification within the nodes.[12] In a recent clinico-radiological prediction model for BAF from Korea, lymph node enlargement and calcification were important diagnostic predictors along with age >70 years, female gender, and active tuberculosis. Other radiological findings such as atelectasis, stenosis, and bronchial wall thickening too were considered to be important predictors of BAF.[25] In a CT-based study from Iran, enlarged mediastinal and peribronchial lymph nodes were detected in 56 of 58 (96.5%) and 46 of 58 (79.3%) patients, respectively.[13] Increasing use of endobronchial ultrasound (EBUS) guidance has led to increased detection of mediastinal nodes on bronchoscopy and would be of help in confirming nodes with anthracotic pigmentation. In a retrospective study from India, of the 300 patients with mediastinal adenopathy who underwent EBUS, 17 had cytopathological evidence of anthracosis, 2 of whom were diagnosed with tuberculosis. These patients had visual evidence of BAF on FOB. EBUS-guided fine-needle aspirate from these lymph nodes revealed black particulate matter or even in some cases “black tarry thick liquid.”[26] It is postulated that mediastinal lymphadenopathy with calcification is due to inhaled carbon particles present in the biomass fuel smoke which are then phagocytosed by the pulmonary macrophages leading to deposition in the lymphatic tissue. In addition, silica present in the smoke induces parenchymal fibrosis and calcification of the lymph nodes.[1,5]
Figure 18.

Contrast-enhanced CT of chest (mediastinal window) showing calcified subcarinal (black arrow) and left hilar lymph node (white arrowhead) in a 73-year-old female with BAF involving right middle lobe
Pleural involvement
Pleural involvement in patients with BAF is usually a part of an associated disease process such as tuberculosis or malignancy. This usually manifests as pleural effusion or pleural thickening. A high index of suspicion for pulmonary tuberculosis should always be kept in mind in a patient with BAF presenting with pleural effusion [Figure 19]. In a study on HRCT findings in patients with BAF, pleural effusion was seen in 17 of 58 (29.3%) patients while pleural thickening was reported in 14 of 58 (24.1%) patients.[13] In the series by Chung et al.,[5] pleural effusion was seen in 4 of 28 patients.
Figure 19.

Contrast-enhanced CT of chest (mediastinal window) in a 70-year-old female with 40 years history of biomass fuel smoke exposure and right lower lobe BAF showing left-sided pleural effusion. Bronchial aspirate cultured Mycobacterium tuberculosis
Radiological features of BAF associated with tuberculosis
Pulmonary tuberculosis, seen in a third of patients with BAF, is now considered to be an associated condition rather than a causative factor. BAF associated with tuberculosis has a distinct radiological presentation.[18] HRCT findings in these patients include consolidation both lobar and multifocal [Figure 9], cavitation, “tree-in-bud” nodules [Figure 16], mediastinal adenopathy, and pleural involvement [Figure 19].[27] On contrast-enhanced CT chest, these mediastinal lymph nodes frequently show contrast enhancement with heterogeneous densities suggestive of areas with necrosis. Dhamija et al.[26] reported that 17 of 300 patients with mediastinal adenopathy who underwent EBUS had visual evidence of BAF, 2 of whom were culture-positive for M. tuberculosis. Transbronchial or EBUS-guided needle aspirations from these nodes show anthracotic pigment-laden macrophages, areas of necrosis, and granulomas.[26]
Conclusion
The diagnosis of BAF can only be established on bronchoscopic visualization of anthracotic pigmentation along with narrowing/distortion of the affected bronchus. Biomass fuel smoke exposure is a common risk factor for the development of COPD and BAF. If no further investigations are done, these patients would continue to be treated as COPD and the diagnosis of BAF would be overlooked. Since most patients are reluctant to undergo bronchoscopy, an invasive procedure, a diagnosis of BAF often remains unconfirmed. Although associated conditions such as tuberculosis, COPD, pneumonia, and malignancy, when present, can confound the radiological picture, HRCT may still provide the initial diagnostic clues in an appropriate clinically setting. Imaging by proving the initial clue also helps decision-making and facilitates bronchoscopy. Multifocal bronchial narrowing, when present on HRCT, is the most characteristic feature of BAF.[1,3] In addition, peribronchial cuffing and mediastinal lymphadenopathy too can be considered as diagnostic predictors of BAF.[25]
There is a need to focus on the development of noninvasive techniques for an early diagnosis of BAF and to evolve appropriate treatment strategies. Currently, it appears that a preventive approach remains the only means of reducing morbidity and mortality by highlighting the perilous consequences of biomass fuel smoke exposure, especially in developing countries.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors are grateful to Dr Shruti Mittal, Junior Resident, Department of Radiodiagnosis, Maulana Azad Medical College and associated Lok Nayak Hospital for her help with the imaging.
References
- 1.Gupta A, Shah A. Bronchial anthracofibrosis: An emerging pulmonary disease due to biomass fuel exposure. Int J Tuberc Lung Dis. 2011;15:602–12. doi: 10.5588/ijtld.10.0308. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. World Health Statistics, 2010. Geneva, Switzerland: World Health Organization; 2010. [accessed on July 17, 2017]. Available from URL: http://www.who.int/whosis/whostat/2010/en/ [Google Scholar]
- 3.World Health Organization. The World health statistics: 2012. [accessed on July 17, 2017]. Available from URL: http://www.who.int/whois/whostat/2012/en/
- 4.Shah A. Bronchial anthracofibrosis: A perilous consequence of exposure to biomass fuel smoke [Editorial] Indian J Chest Dis Allied Sci. 2015;57:151–3. [PubMed] [Google Scholar]
- 5.Chung MP, Lee KS, Han J, Kim H, Rhee CH, Han YC, et al. Bronchial stenosis due to anthracofibrosis. Chest. 1998;113:344–5. doi: 10.1378/chest.113.2.344. [DOI] [PubMed] [Google Scholar]
- 6.Klotz O. Pulmonary anthracosis -a community disease. Am J Public Health (NY) 1914;4:887–916. doi: 10.2105/ajph.4.10.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen AG. Atelectasis of the right middle lobe resulting from perforation of tuberculous lymph nodes into bronchi in adults. Ann Intern Med. 1951;35:820–35. doi: 10.7326/0003-4819-35-4-820. [DOI] [PubMed] [Google Scholar]
- 8.Sigari N, Mohammadi S. Anthracosis and anthracofibrosis. Saudi Med J. 2009;30:1063–6. [PubMed] [Google Scholar]
- 9.Kim YJ, Jung CY, Shin HW, Lee BK. Biomass smoke induced bronchial anthracofibrosis: Presenting features and clinical course. Respir Med. 2009;103:757–65. doi: 10.1016/j.rmed.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 10.Pilaniya V, Kunal S, Shah A. Occurrence of bronchial anthracofibrosis in respiratory symptomatics with exposure to biomass fuel smoke. Adv Respir Med. 2017;85:127–35. doi: 10.5603/ARM.2017.0022. [DOI] [PubMed] [Google Scholar]
- 11.Kala J, Sahay S, Shah A. Bronchial anthracofibrosis and tuberculosis presenting as a middle lobe syndrome. Prim Care Respir J. 2008;17:51–5. doi: 10.3132/pcrj.2008.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim HY, Im JG, Goo JM. Bronchial anthracofibrosis (inflammatory bronchial stenosis with anthracotic pigmentation): CT findings. AJR Am J Roentgenol. 2000;174:523–7. doi: 10.2214/ajr.174.2.1740523. [DOI] [PubMed] [Google Scholar]
- 13.Kahkouee S, Pourghorban R, Bitarafan M, Najafizadeh K, Makki SS. Imaging findings of isolated bronchial anthracofibrosis: A computed tomography analysis of patients with bronchoscopic and histologic confirmation. Arch Bronconeumol. 2015;51:322–7. doi: 10.1016/j.arbres.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 14.Kim HJ, Kim SD, Shin DW, Bae SH, Kim AL, Kim JN, et al. Relationship between bronchial anthracofibrosis and endobronchial tuberculosis. Korean J Intern Med. 2013;28:330–8. doi: 10.3904/kjim.2013.28.3.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Criado E, Sánchez M, Ramírez J, Arguis P, de Caralt TM, Perea RJ, et al. Pulmonary sarcoidosis: Typical and atypical manifestations at high-resolution CT with pathologic correlation. Radiographics. 2010;30:1567–86. doi: 10.1148/rg.306105512. [DOI] [PubMed] [Google Scholar]
- 16.Moran-Mendoza O, Pérez-Padilla JR, Salazar-Flores M, Vazquez-Alfaro F. Wood smoke-associated lung disease: A clinical, functional, radiological and pathological description. Int J Tuberc Lung Dis. 2008;12:1092–8. [PubMed] [Google Scholar]
- 17.Gupta P. The Golden S sign. Radiology. 2004;233:790–1. doi: 10.1148/radiol.2333021407. [DOI] [PubMed] [Google Scholar]
- 18.Kunal S, Shah A. The concomitant occurrence of pulmonary tuberculosis with bronchial anthracofibrosis. Indian J Tuberc. 2017;64:5–9. doi: 10.1016/j.ijtb.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 19.Gudbjartsson T, Gudmundsson G. Middle lobe syndrome: A review of clinicopathological features, diagnosis and treatment. Respiration. 2012;84:80–6. doi: 10.1159/000336238. [DOI] [PubMed] [Google Scholar]
- 20.Lee HS, Maeng JH, Park PG, Jang JG, Park W, Ryu DS, et al. [Clinical features of simple bronchial anthracofibrosis which is not associated with tuberculosis] Tuberc Respir Dis. 2002;53:510–8. [Google Scholar]
- 21.Torun T, Gungor G, Ozmen I, Maden E, Bolukbasi Y, Tahaoglu K. Bronchial anthracostenosis in patients exposed to biomass smoke. Turkish Respir J. 2007;8:48–51. [Google Scholar]
- 22.Kunal S, Pilaniya V, Shah A. Bronchial anthracofibrosis with interstitial lung disease: An association yet to be highlighted. BMJ Case Rep 2016. 2016 doi: 10.1136/bcr-2015-213940. pii:bcr2015213940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kunal S, Pilaniya V, Shah A. The co-occurrence of bronchial anthracofibrosis and interstitial lung disease. Arch Bronconeumol. 2017;53:218–9. doi: 10.1016/j.arbres.2016.06.017. [DOI] [PubMed] [Google Scholar]
- 24.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: Glossary of terms for thoracic imaging. Radiology. 2008;246:697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 25.Park TY, Heo EY, Chung HS, Jin KN, Kim DK. Prediction of anthracofibrosis based on clinico-radiographic findings. Yonsei Med J. 2017;58:355–61. doi: 10.3349/ymj.2017.58.2.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dhamija A, Basu A, Sharma V, Bakshi P, Verma K. Mediastinal adenopathy in India: Through the eyes of endobranchial ultrasound. J Assoc Physicians India. 2015;63:15–8. [PubMed] [Google Scholar]
- 27.Choe HS, Lee IJ, Lee Y. [The CT findings of bronchial anthracofibrosis: Comparison of cases with or without active tuberculosis] J Korean Radiol Soc. 2004;50:109–14. [Google Scholar]


