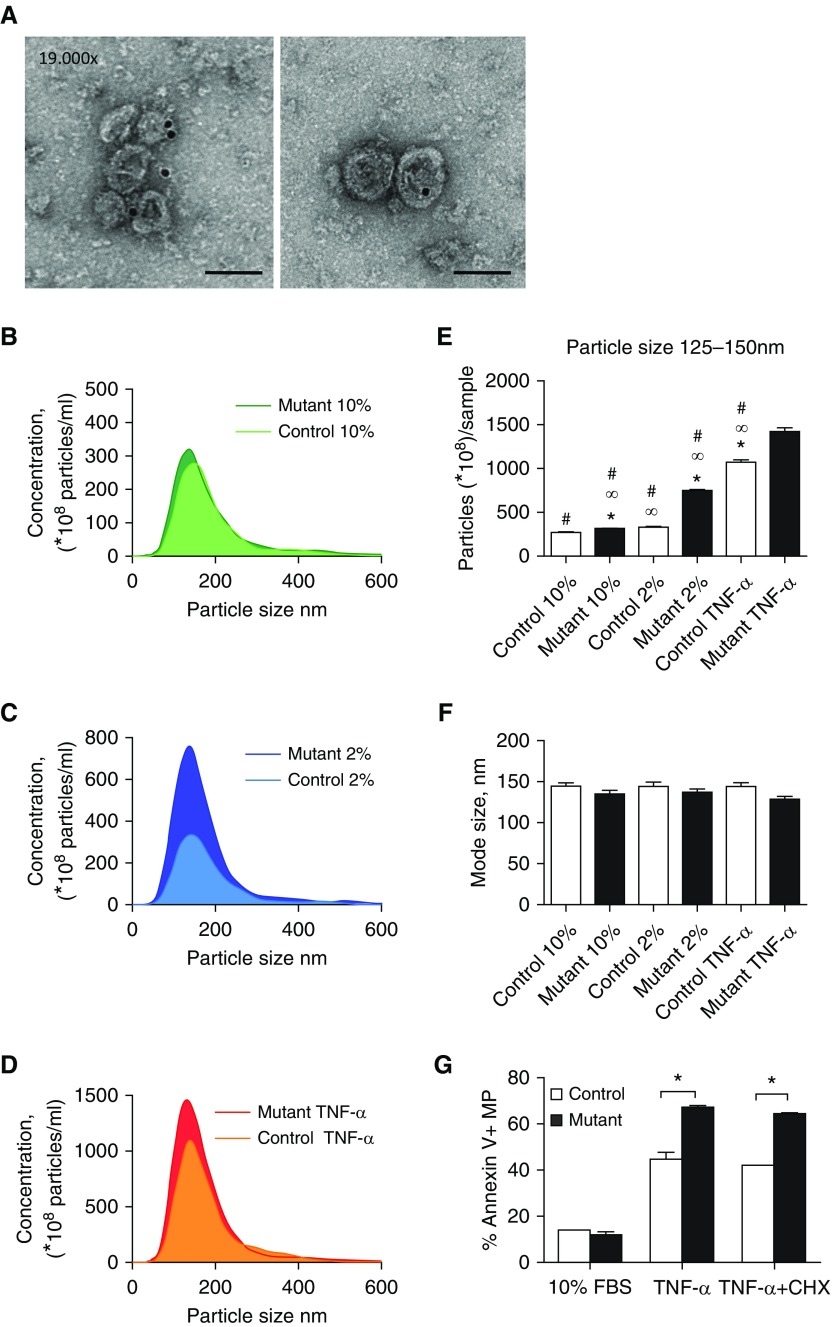
Figure 2.
BOECs bearing BMPR2 mutations produce and release more extracellular vesicles. (A) Electron microscopy images of exosomes isolated by ultracentrifugation and positive immunogold staining with anti-CD81 antibody. Scale bars: 100 nm. (B–D) Nanoparticle tracking analysis (NTA) assessment of exosomes from human control (light color) and heritable pulmonary arterial hypertension (HPAH)-derived (dark color) BOECs (three replicates for each group; n = 4). (B) Basal conditions: 10% exosome-free FBS plus growth factors for 24 hours (10%). (C) Activation conditions: 2% exosome-free FBS for 24 hours (2%). (D) Stress conditions: 2% exosome-free FBS for 24 hours with TNF-α (3 ng/ml) for the final 6 hours. (E) Particle concentration evaluation of exosomes ranging from 125–150 nm by NTA from control and HPAH-derived BOECs in the above conditions (n = 4 in triplicates; one-way ANOVA, ∞P < 0.05 versus control 10% FBS, *P < 0.05 versus control 2% FBS, #P < 0.05 versus mutant TNF-α). (F) Mode size of nanoparticles in all groups corresponding to the range of exosome size (125–150 nm) (n = 4; one-way ANOVA). (G) Microparticles (<1 μm) were identified and quantified by flow cytometry by positive staining for AnnexinV. Microparticles were derived from control and HPAH-derived BOECs under the following conditions: basal conditions (10% exosome-free FBS plus growth factors for 24 hours [10% FBS; n = 4]; stress conditions (2% exosome-free FBS for 24 hours with TNF-α [3 ng/ml] [TNF-α; n = 4]; and apoptosis/stress conditions (2% exosome-free FBS for 24 hours with TNF-α [3 ng/ml] and cycloheximide [CHX; 20 μg/ml] for the final 6 hours [TNF-α + CHX; n = 4]). One-way ANOVA; *P < 0.05. Error bars represent mean ± SEM.