Abstract
Aims/hypothesis
This study aimed to examine recent time trends in the incidence and prevalence of type 2 diabetes in Norway.
Methods
In this Norwegian nationwide cohort study, we linked data from national registries with prospectively collected data on diabetes medication and diabetes diagnoses for all residents in Norway aged 30 to 89 years (>3.2 million people). We analysed trends in incidence and prevalence of type 2 diabetes from 2009 to 2014 by type of treatment, sex, age, education level and place of birth.
Results
During 15,463,691 person-years of follow-up from 2009 to 2014, we identified 75,496 individuals with new-onset type 2 diabetes. Of these, 36,334 (48%) were treated with blood-glucose-lowering drugs within 6 months of diagnosis. A low education level and being born in Asia, Africa or South America were significant risk factors for incident type 2 diabetes. While the prevalence of type 2 diabetes increased from 4.9% to 6.1% during the study period, the incidence decreased significantly from 609 cases per 100,000 person-years in 2009 to 398 cases per 100,000 in 2014, an annual reduction of 10.1% (95% CI −10.5, −9.6). A declining incidence was seen for both pharmacologically and non-pharmacologically treated type 2 diabetes, and in all subgroups defined by sex, age group, education level and place of birth.
Conclusions/interpretations
This nationwide study shows that, despite a decreasing incidence of type 2 diabetes in Norway, the prevalence continues to rise, probably due to diagnosis at a younger age and increased longevity.
Electronic supplementary material
The online version of this article (10.1007/s00125-018-4681-4) contains peer-reviewed but unedited supplementary material, which is available to authorised users.
Keywords: Incidence, Prevalence, Register-based study, Time trends, Type 2 diabetes

Introduction
The prevalence of type 2 diabetes seems to be increasing in most parts of the world [1]. Prevalence of type 2 diabetes is determined by the incidence of the disease, mortality rates and other factors, such as population ageing, immigration and composition of ethnic groups, age at diagnosis, and changes in diagnostic criteria and screening activities [2]. Time trends in incidence are, therefore, potentially more informative than prevalence estimates with regards to the effects of modifiable risk factors for type 2 diabetes. Few studies report time trends in incidence of type 2 diabetes, particularly from nationally representative cohorts. Norwegian data showed no increase in incidence of non-insulin glucose lowering drug use during 2006–2011 [3]. This study, however, lacked information about the type of diabetes, non-pharmacologically treated diabetes and important demographic factors, such as immigration, ethnic background and education level.
Although the majority of people with type 2 diabetes receive pharmacological treatment [4–6], a proportion of adults with type 2 diabetes (20–40%) are omitted from analyses when only pharmacologically treated individuals are included [7–10]. Thus, differences over time in treatment patterns have not been covered by previous studies. This provides justification for the present study, which includes time trends in both pharmacologically and non-pharmacologically treated type 2 diabetes.
The complex relationship between incidence, mortality and prevalence of type 2 diabetes remains to be elucidated. In the current study, data from mandatory nationwide registries on demographic characteristics, prescription drugs, and primary and specialist healthcare visits were combined to examine recent trends in incidence and prevalence of diagnosed type 2 diabetes in Norway.
Methods
The Regional Committee for Medical and Health Research Ethics and the Norwegian Data Protection Authority approved the study.
Participants
In this open cohort study, we included all residents aged 30 to 89 in the period 2009 to 2014 (>3.2 million individuals). Individuals were followed from either 1 January 2009, at the age of 30 years, or 1 year after immigration to Norway, whichever occurred later. We followed individuals until diabetes diagnosis, dispense of blood-glucose-lowering medication, emigration, death, 90 years of age or the end of study period, whichever occurred first.
Data sources
The Norwegian public health system is financed through government funding. Hospitalisations are free of charge, while there is a fee for consultations in primary care and out-of-hospital visits. We used individual-level data from three national databases (the Norwegian Prescription Database, the Norwegian Patient Registry [NPR] and the primary care database). Data were linked by means of the personal identification number unique to every Norwegian resident.
The Norwegian Prescription Database was established in 2004 and holds information on all drugs dispensed by Norwegian pharmacies. Blood-glucose-lowering drug prescriptions are classified according to the Anatomical Therapeutic Chemical (ATC) classification system in group A10 (‘Drugs used in diabetes’). In the present study, we collected information about dates and details of all glucose-lowering drugs dispensed from Norwegian pharmacies from 2004 to 2014. We included insulins and analogues classified as A10A (‘Insulins and analogues’), and non-insulin glucose-lowering medications, classified in A10B (‘Blood glucose lowering drugs, excl. insulins’).
The NPR is an administrative database covering all hospitalisations and specialist healthcare outpatient contacts in Norway, with linkable data from 2008 onwards. Diabetes diagnoses are reported according to the International Classification of Diseases, version 10 (ICD-10, www.who.int/classifications/icd/en/), in the group E10–E14 (‘Diabetes mellitus’). We collected information on date of first diagnosis and the number of times individuals were registered with these diagnoses. In the primary care database, diabetes was reported from 2006 according to The International Classification of Primary Care, Second Edition (ICPC-2; www.who.int/classifications/icd/adaptations/icpc2/en/) codes T89 (‘Diabetes insulin dependent’) and T90 (‘Diabetes non-insulin dependent’). Reporting to these health registries is compulsory and linked to the reimbursement system, with nearly complete coverage of the population (ESM Fig. 1).
Type 2 diabetes case definition
We defined type 2 diabetes from register-based data as at least one registration of type 2 diabetes diagnosis and use of non-insulin glucose-lowering drugs, or two registrations if individuals were not treated with non-insulin glucose-lowering drugs (either E11 diagnosis code from specialist care (ICD-10) or T90 diagnosis code from the primary care database [ICPC-2]).
Case definition of prevalent type 2 diabetes
Prevalent type 2 diabetes cases were defined as having at least one E11 or T90 diagnosis of type 2 diabetes and one or more prescriptions of non-insulin glucose-lowering drugs, or being registered with a type 2 diabetes diagnosis on at least at two different occasions. For each calendar year from 2009 to 2014, we defined the period prevalence as the number of people defined as having type 2 diabetes in that year or earlier, divided by the total number of individuals alive, aged 30 to 89 years and residing in Norway during the same calendar year (ESM Fig. 2). The end of follow-up was 31 December 2014.
Case definition of incident type 2 diabetes
To avoid any prevalent cases of type 2 diabetes at baseline, we excluded individuals with a diagnosis of any type of diabetes or who used any blood-glucose-lowering drugs before the study start on 1 January 2009. We defined incident cases of pharmacologically treated type 2 diabetes as having the first occurrence of diabetes diagnosis in primary or specialist care and one or more prescriptions of non-insulin glucose-lowering drugs within 6 months of diagnosis. Incident cases of non-pharmacologically treated diabetes were defined as no registrations of glucose-lowering drugs and having been registered with a diagnosis of type 2 diabetes (in primary and/or specialist care) on at least two different occasions (ESM Fig. 3). The end of follow-up was 30 June 2014. Data are available until 31 December 2014, but to allow ascertainment for 6 months with or without A10 medication in the incidence analysis, we stopped follow-up time 6 months before the end of the study period. Of all incident cases, 39% were recorded in the three health registers, 36% in two registers and 26% in one register with at least two registrations of a type-2-diabetes diagnosis (ESM Fig. 4).
Covariates
Information on sex and dates of birth, emigration and death were obtained from the National Registry [11]. Statistics Norway provided information on immigration, place of birth and education level [12]. We had information on the highest education level achieved in year 2013. Place of birth was categorised in seven broad categories: Norway, Europe except Norway, Africa, Asia, North and Central America, South America and Oceania.
Sensitivity analysis
The number of individuals per year with possible diabetes but excluded in our algorithm (unclassified diabetes and those treated with glucose-lowering medication without a registered diagnosis of type 2 diabetes) were assessed to identify if misclassification could explain the changes in incidence trends.
Data analysis
We estimated prevalence by counting all individuals with type 2 diabetes who were alive and aged 30–89 at some time during the given calendar year, until they emigrated or died, and dividing this number by the total number of individuals alive, aged 30 to 89 years and residing in Norway during the same calendar year (ESM Fig. 2). We estimated incidence rates with 95% CI per 100,000 person-years of follow-up, stratified by covariates such as calendar year and age group. Incidence rates were not adjusted or standardised.
Associations between risk factors and type 2 diabetes were assessed using Cox regression. We calculated annual percentage difference in incidence using Poisson regression. To assess whether the time trend in incidence changed after the date when HbA1c ≥48 mmol/mol (6.5%) was recommended for diagnosing diabetes in Norway (September 2012), we used interrupted time series analysis [13]. Details of the Poisson regression models used for the latter are described in ESM Methods. Data handling and analyses were done using Stata version 15 (StataCorp, College Station, TX, USA).
Results
Time trends in prevalence
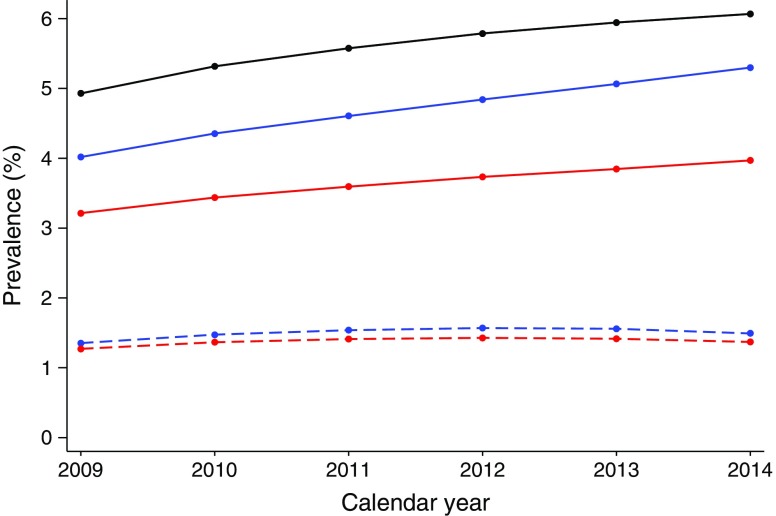
From 2009 to 2014, the prevalence of type 2 diabetes in Norway increased from 4.9% to 6.1% of the total population aged 30–89 (ESM Table 1). Overall, 23.6% of individuals with diabetes did not use glucose-lowering medications (Fig. 1). Type 2 diabetes was more prevalent in males than females (6.8% vs 5.3% in 2014) and the prevalence increased with age (ESM Fig. 5).
Fig. 1.
Time trends in proportion of people diagnosed with type 2 diabetes in the population aged 30–89 years in Norway from 2009 to 2014, in all participants and by treatment and sex. Black line, all participants; blue lines, men; red lines, women; solid lines, pharmacologically treated; dashed lines, non-pharmacologically treated
Time trends in incidence
A total of 3,227,454 individuals aged 30–89 years were included in the analysis, with a mean follow-up of 4.8 years (range 0.002–5.5 years) (Table 1). During 15,463,691 person-years of follow-up, we identified 75,496 new cases of type 2 diabetes, corresponding to an overall incidence rate of 488.2 per 100,000 person-years (Table 2). In total, 39,162 (51.9%) of incident cases were not treated with glucose-lowering medication within 6 months of diagnosis, while 36,334 (48.1%) were treated (ESM Table 2). The mean age at diagnosis was 59.2 years for those pharmacologically treated and 62.8 years for the non-pharmacologically treated. Of the pharmacologically treated individuals, 82.6% used monotherapy metformin as their initial treatment, 4.4% used sulfonylurea monotherapy, 0.3% used other oral agents and 0.9% started treatment with insulin only (ESM Table 3). Eleven per cent started with two or more drugs within the first month of treatment (ESM Table 3).
Table 1.
Characteristics of the study population for incidence analysis
| Characteristic | All participants | Type 2 diabetes, pharmacologically treateda | Type 2 diabetes, non-pharmacologically treatedb |
|---|---|---|---|
| n | 3,227,454 | 36,334 | 39,162 |
| Sex, n (%) | |||
| Male | 1,609,058 (50) | 22,168 (61) | 21,720 (56) |
| Female | 1,618,396 (50) | 14,166 (39) | 17,442 (45) |
| Year of birth | |||
| 1910–1919 | 8685 (0.3) | 13 (0.04) | 15 (0.04) |
| 1920–1929 | 174,081 (5.4) | 1951 (5.4) | 3087 (7.9) |
| 1930–1939 | 261,321 (8.1) | 4824 (13.3) | 7235 (18.5) |
| 1940–1949 | 464,082 (14.4) | 8955 (24.6) | 11,503 (29.4) |
| 1950–1959 | 592,202 (18.3) | 9673 (26.6) | 9670 (24.7) |
| 1960–1969 | 704,276 (21.8) | 7489 (20.6) | 5492 (14.0) |
| 1970–1979 | 716,390 (22.2) | 3163 (8.7) | 2000 (5.1) |
| 1980–1989 | 306,417 (9.5) | 266 (0.7) | 160 (0.4) |
| Education level, n (%) | |||
| ≤10 years | 739,443 (23) | 12,904 (36) | 13,153 (34) |
| 11–13 years | 1,352,663 (42) | 16,551 (46) | 18,532 (47) |
| >13 years | 1,020,357 (32) | 6129 (17) | 7017 (18) |
| No information | 114,991 (4) | 750 (2) | 460 (1) |
| Place of birth, n (%) | |||
| Norway | 2,745,774 (85.1) | 30,714 (84.5) | 34,765 (88.8) |
| Europe (except Norway) | 284,417 (8.8) | 2233 (6.1) | 1702 (4.3) |
| Asia | 117,438 (3.6) | 2303 (6.3) | 1921 (4.9) |
| Africa | 44,061 (1.4) | 731 (2.0) | 513 (1.3) |
| North and Central America | 19,557 (0.6) | 158 (0.4) | 135 (0.3) |
| South America | 14,012 (0.4) | 188 (0.5) | 116 (0.3) |
| Oceania | 2195 (0.07) | 7 (0.02) | 10 (0.03) |
Individuals aged 30–89 years in Norway from 2009 to 2014 were included in the analysis
aAt least one diagnosis of type 2 diabetes and use of non-insulin glucose-lowering medication within 6 months of first being registered with diabetes
bAt least two diagnoses of type 2 diabetes and not treated with glucose-lowering medication within 6 months of first being registered with diabetes
Table 2.
Incidence of registered type 2 diabetes in the population aged 30–89 years in Norway from 2009 to 2014 and association of covariates with the risk of type 2 diabetes diagnosis
| Characteristic | Incidence cases (n) | Person-years | Incidence rate per 100,000 person-years (95% CI) | HR (95% CI)a | |
|---|---|---|---|---|---|
| Unadjusted | Adjustedb | ||||
| All participants | 75,496 | 15,463,691 | 488.2 (484.7, 491.7) | ||
| Male | 43,888 | 7,642,520 | 574.3 (568.9, 579.7) | 1 | 1 |
| Female | 31,608 | 7,821,171 | 404.1 (399.7, 408.6) | 0.67 (0.66, 0.68) | 0.66 (0.65, 0.67) |
| Year of birth | |||||
| 1910–1919 | 28 | 4327 | 647.1 (446.8, 937.2) | 8.70 (5.62, 13.48) | 8.73 (5.63, 13.53) |
| 1920–1929 | 5038 | 658,818 | 764.7 (743.9, 786.1) | 6.58 (5.47, 7.91) | 6.60 (5.48, 7.95) |
| 1930–1939 | 12,059 | 1,282,636 | 940.2 (923.5, 957.1) | 4.14 (3.48, 4.90) | 4.15 (3.55, 5.00) |
| 1940–1949 | 20,458 | 2,397,076 | 853.5 (841.8, 865.2) | 2.65 (2.26, 3.12) | 2.73 (2.32, 3.22) |
| 1950–1959 | 19,343 | 3,114,908 | 621.0 (612.3, 629.8) | 1.90 (1.63, 2.22) | 1.98 (1.69, 2.32) |
| 1960–1969 | 12,981 | 3,708,046 | 350.1 (344.1, 356.2) | 1.53 (1.32, 1.77) | 1.57 (1.35, 1.82) |
| 1970–1979 | 5163 | 3,644,665 | 141.7 (137.8, 145.6) | 1.27 (1.11, 1.44) | 1.29 (1.13, 1.48) |
| 1980–1989 | 426 | 653,215 | 65.2 (59.3, 71.7) | 1 | 1 |
| Education level | |||||
| ≤10 years | 26,057 | 3,488,171 | 747.0 (738.0, 756.1) | 2.15 (2.10, 2.19) | 2.10 (2.05, 2.14) |
| 11–13 years | 35,083 | 6,702,359 | 523.4 (518.0, 528.9) | 1.59 (1.55, 1.62) | 1.60 (1.57, 1.63) |
| >13 years | 13,146 | 4,944,843 | 265.9 (261.3, 270.4) | 1 | 1 |
| Place of birth | |||||
| Norway | 65,479 | 13,565,793 | 482.7 (479.0, 486.4) | 1 | 1 |
| Europe (except Norway) | 3935 | 1,089,376 | 361.2 (350.1, 372.7) | 1.08 (1.05, 1.12) | 1.14 (1.10, 1.17) |
| Africa | 1244 | 169,999 | 731.8 (692.2, 773.6) | 2.95 (2.79, 3.12) | 2.72 (2.57, 2.88) |
| Asia | 4224 | 486,508 | 868.2 (842.4, 894.8) | 3.15 (3.05, 3.25) | 3.08 (2.98, 3.18) |
| North and Central America | 293 | 86,535 | 338.6 (302.0, 379.7) | 0.88 (0.78, 0.98) | 1.02 (0.91, 1.15) |
| South America | 304 | 57,033 | 533.0 (476.4, 596.4) | 1.75 (1.56, 1.96) | 1.83 (1.63, 2.05) |
| Oceania | 7 | 8447 | 201.2 (125.1, 323.7) | 0.68 (0.42, 1.10) | 0.76 (0.47, 1.23) |
aHRs are from Cox regression analysis
bAdjusted for sex, year of birth (in 10-year categories), education level and place of birth
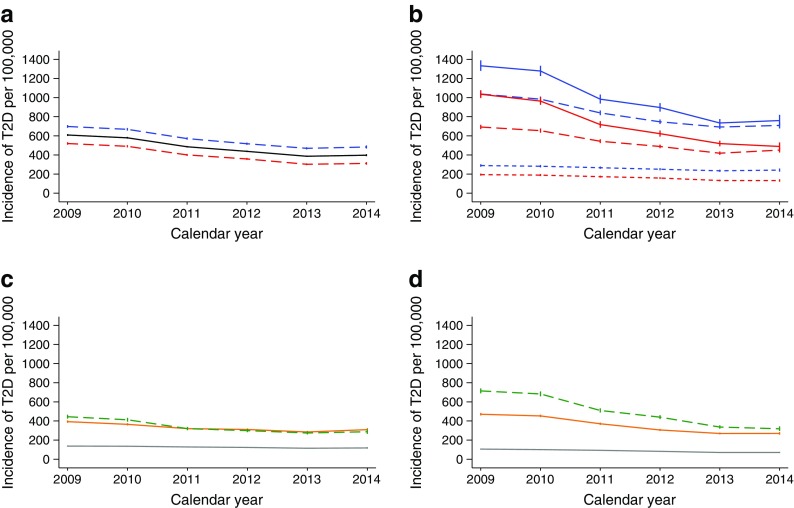
During the study period, there was a significant decrease in the incidence of type 2 diabetes in all age groups examined, and we observed a decrease for both pharmacologically treated and non-pharmacologically treated type 2 diabetes (Fig. 2). The incidence of type 2 diabetes decreased from 609 cases per 100,000 person-years in 2009 to 398 cases per 100,000 person-years in 2014. The annual reduction was 10.1% (95% CI −10.5, −9.6). The absolute decrease in incidence was most pronounced in the group aged 70–89, particularly for those not treated with glucose-lowering medication (Fig. 2).
Fig. 2.
Incidence trends in type 2 diabetes (a) Stratified by sex: blue line, men; red line, women; black line, all participants. Average annual per cent change in incidence rate: −10.1 (95% CI −10.5, −9.6). (b) Stratified by age group and sex: blue line, men; red line, women; solid line, age group 70–89 years; long dashed line, age group 50–69 years; short dashed line, age group 30–49 years. (c) Stratified by age for those treated with glucose-lowering medication within 6 months of diagnosis. (d) Stratified by age group for those not treated with glucose-lowering medication within the first 6 months of diagnosis. In (c) and (d): grey line, age group 30–49 years; orange line, age group 50–69 years; green line, age group 70–89 years. Data are presented as cases per 100,000 person-years with vertical bars representing 95% CI. T2D, type 2 diabetes
The decline in incidence was statistically significant in all groups except for people born in Africa (Fig. 3a). While the incidence of type 2 diabetes was higher for people with lower levels of education, there was a statistically significant decrease in incidence in all education groups (Fig. 3b). Time trends were similar for men and women (Fig. 2a).
Fig. 3.
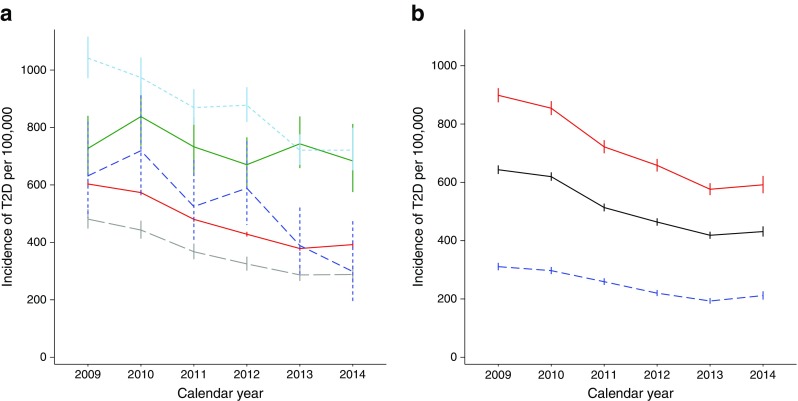
Incidence trends for type 2 diabetes by place of birth and by education level. (a) By place of birth: red line, Norway; dashed grey line, Europe (except Norway); green line, Africa; dashed light-blue line, Asia; dashed dark-blue line, South America. Since there were very few cases from Oceania and North and Central America, to improve interpretability, data from these places of birth have not been included in the graph. (b) By education: red line, lower education level (≤10 years); black line, medium education level (11–13 years); dashed blue line, high education level (>13 years). Results stratified by education level are shown for individuals born in Norway only (85% of the source population), because of a high proportion of missing data on education level for people born abroad. Data are presented as cases per 100,000 person-years with vertical bars representing 95% CI. T2D, type 2 diabetes
Change in time trends after recommended use of HbA1c for diabetes diagnosis
We found a small but statistically significant reduction in the rate of change in incidence from September 2012, when HbA1c was introduced as a recommended diagnostic criterion for diabetes in Norway (ESM Fig. 6). While there was a 12.0% decline per year up to this point, the decline in incidence was 7.9% per year thereafter (test for slope change, p = 0.001).
Sensitivity analysis
To investigate whether the observed time trends were sensitive to our operational definition of incident type 2 diabetes, we evaluated whether there were time trends in the number of individuals per year with possible diabetes who did not satisfy our criteria. There were no clear changes in incident unclassified diabetes and in those using non-insulin glucose-lowering medication without having a registered diabetes diagnosis (ESM Fig. 7). These findings indicate that our observed time trends in incidence of type 2 diabetes were robust to different operational definitions.
Discussion
We observed decreasing incidence of diagnosed type 2 diabetes in Norway during 2009–2014, although prevalence increased at the same time. The declining incidence was seen for both pharmacologically and non-pharmacologically treated type 2 diabetes, and in subgroups defined by age, sex, education level and place of birth.
The main strength of the present study was the use of nationwide registries with nearly complete registration of data and precise linkage by means of the unique personal identification number. We used information on diabetes diagnoses reported from both primary and specialist healthcare, as well as data on dispensing of glucose-lowering medication from pharmacies. The registry-based approach we used relies on clinical judgement and correct coding and reporting [14]. However, we find it likely that we have captured most individuals with diabetes through our pre-defined algorithm for case ascertainment that used combined, longitudinal information from three independent sources.
A major limitation of this registry-based study was that we had no information available on laboratory data. We were therefore not able to formally validate the classification of diabetes based on variables such as islet autoantibodies or C-peptide. Furthermore, some individuals with possible diabetes were inevitably excluded according to our algorithm. Requiring a registered diagnosis of type 2 diabetes, for those treated with non-insulin glucose-lowering medication, could have led to some degree of underestimation of incidence rates. However, the number of individuals per year with incident unclassifiable or potential diabetes (not fulfilling our requirements) was stable over the time period studied, supporting our observation that the declining incidence of type 2 diabetes was not due to an increased number of unclassified cases. The registries used do not register diagnoses or medications received in nursing homes, which may, to some extent, underestimate the incidence and prevalence values in the upper age groups. However, nursing-home residents may also receive primary or specialist healthcare. In addition, the majority of nursing-home residents arrive after a hospital stay (when any diabetes diagnosis should be registered). Only 3.8% of Norwegian residents aged 67–89 live in nursing homes [15] and the average time of residing in nursing homes is only 3.2 years. Thus, missing information on healthcare and medication for people residing in nursing homes is not likely to be a major source of error.
Another possible source of error is misclassification of prevalent cases as incident cases of type 2 diabetes [16]. This could occur for individuals not treated with glucose-lowering medication, or if diabetes diagnoses are not registered because they co-exist with other diseases or conditions. However, if such mechanisms were to contribute strongly to the observed declining incidence, we would expect a much stronger decline from 2009 to 2010 than that from 2010 to 2011, and so forth. As this was not the case, and as we used a relatively long washout period, we consider it most likely that the observed decline in type 2 diabetes incidence was real.
Only a few published studies present recent trends in the incidence of type 2 diabetes. Data from the UK [17] and from Scotland [18], also based on databases, reported stable or decreasing incidence of type 2 diabetes up to 2013. Furthermore, two studies from the USA, one based on claim data [19] and one based on the National Health Interview Survey [20], showed decreasing incidence of diagnosed diabetes in recent years. We are not aware of any previous studies of type-2-diabetes incidence trends that have shown results separately for pharmacologically and non-pharmacologically treated type 2 diabetes. A number of studies have reported trends in the use of glucose-lowering medication, without independent documentation of type 2 diabetes diagnoses. Norwegian data from 2006 to 2011 [3] and Swedish data from 2006 to 2013 [21] both showed a decrease in new users of glucose-lowering medication, despite concomitantly stable or increasing prevalence of diabetes, in accordance with our results.
The Norwegian Health Directorate introduced HbA1c as the primary diagnostic criterion for diabetes in September 2012 [22]. We observed a change in incidence trends thereafter and thus changes in diagnostic practice may have affected trends in incidence.
Our data do not explain why incidence trends have changed. Possibly, some of the observed decline may be a result of an increase in the ratio of undiagnosed to diagnosed individuals in the population after changes in diagnostic activity. General practitioners may also have started using HbA1c in active case finding before 2012, and part of the declining incidence rates may be influenced by this. The introduction of HbA1c as the recommended diagnostic method in 2012 seemed to have a significant, but limited, impact on trends. Furthermore, it is possible that improvements in lifestyle factors may have contributed to some of the observed changes. While the rise in the prevalence of obesity seems to have plateaued in the USA in recent years up, to 2012 [23], it continued to increase in Norwegian adults up to 2008 [24, 25]. Moreover, bariatric surgery for morbid obesity started in Norway around 2004, and approximately 3000 patients underwent such surgery per year during the study period [26]. This may have contributed to the prevention of type 2 diabetes in these individuals, but can only explain a small proportion of the changes in trends. In line with the decreasing trends in the incidence of cardiovascular disease observed in many parts of the world, including Norway [27], the decreasing incidence of type 2 diabetes may be due to changes in lifestyle factors other than obesity. One plausible candidate is the reduction in smoking. In 2006, the proportion of daily smokers among the Norwegian population (aged 16–74 years) was 24%, compared with 12% in 2016. Assuming a constant relative risk of approximately 1.4 for type 2 diabetes among smokers [28], the observed reduction in the prevalence of smokers in Norway during 2006 to 2016 [29] can only account for a small decline in the incidence of type 2 diabetes.
Our analyses of age, sex, education level and place of birth confirmed established type 2 diabetes associations [30, 31]. Importantly, we observed declining incidence rates in all subgroups analysed.
By combining registries, surveillance of type 2 diabetes and planning of appropriate health services can be improved. Incidence and prevalence trends should be considered in combination to assess the burden of diabetes and the challenges to the health system. If the observed trends continue and are confirmed in future studies, it may suggest that some of the public health actions towards improving risk factors for non-communicable diseases are acting effectively. However, further research is necessary to follow future trends, including changes in mortality as a potential explanation for the different time trends in prevalence and incidence of type 2 diabetes.
Conclusions
Despite the continuing increase in prevalence, we have shown a declining incidence of both pharmacologically and non-pharmacologically treated type 2 diabetes in Norway. This may represent another positive public health trend, in addition to decreasing cardiovascular mortality and increasing life expectancy.
Electronic supplementary material
(PDF 1196 kb)
Acknowledgements
We thank G. Tapia, Norwegian Institute of Public Health (Oslo, Norway), for his help with the figures presented in this manuscript. Data from the NPR has been used in this publication. The interpretation and reporting of these data are the sole responsibility of the authors and no endorsement by the NPR is intended, nor should be inferred. A part of the study in abstract form was presented as a Poster at the 52nd EASD Annual Meeting in Munich, 13–16 September 2016.
Abbreviations
- ICPC-2
The International Classification of Primary Care, Second Edition
- NPR
Norwegian Patient Registry
Contribution statement
LCS, PLDR and IJB had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: LCS, HLG, SEH. Acquisition, analysis or interpretation of data: all authors. PLDR, LCS and HLG wrote the first draft of the manuscript and subsequent revisions. PLDR, LCS and IJB performed the statistical analyses. SEH and IJB provided administrative, technical, and material support.
All authors critically revised the paper for important intellectual content and approved the final version.
Funding
This research was partly supported by the Norwegian Institute of Public Health and a grant from the South-Eastern Norway Regional Health Authority. This work was partly supported by the Research Council of Norway through its Centres of Excellence funding scheme, project number 262700. The sponsors had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to data protection regulations.
Duality of interest
KIB has received grants to his institution for lecturing and consulting from AstraZeneca, Novo Nordisk, Sanofi, Lilly, Boehringer Ingelheim and Merck Sharp & Dohme. HLG has received grants for lectures or consulting from AstraZeneca, Novo Nordisk, Sanofi, Boehringer Ingelheim and Merck Sharp & Dohme. Other authors do not have any conflicts of interest.
References
- 1.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387:1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ma RC, Tong PC. Epidemiology of type 2 diabetes. In: Holt RI, Cockram C, Flyvbjerg A, Goldstein BJ, editors. Textbook of diabetes. Chichester: Wiley; 2017. pp. 43–64. [Google Scholar]
- 3.Strøm H, Selmer R, Birkeland KI, et al. No increase in new users of blood glucose-lowering drugs in Norway 2006–2011: a nationwide prescription database study. BMC Public Health. 2014;14:520. doi: 10.1186/1471-2458-14-520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–149. doi: 10.2337/dc14-2441. [DOI] [PubMed] [Google Scholar]
- 5.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetologia. 2012;55:1577–1596. doi: 10.1007/s00125-012-2534-0. [DOI] [PubMed] [Google Scholar]
- 6.McGuire H, Longson D, Adler A, Farmer A, Lewin I. Management of type 2 diabetes in adults: summary of updated NICE guidance. BMJ. 2016;353:i1575. doi: 10.1136/bmj.i1575. [DOI] [PubMed] [Google Scholar]
- 7.Bakke Å, Cooper JG, Thue G, et al. Type 2 diabetes in general practice in Norway 2005–2014: moderate improvements in risk factor control but still major gaps in complication screening. BMJ Open Diabetes Res Care. 2017;5:e000459. doi: 10.1136/bmjdrc-2017-000459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rawshani A, Rawshani A, Franzén S, et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017;376:1407–1418. doi: 10.1056/NEJMoa1608664. [DOI] [PubMed] [Google Scholar]
- 9.Shah AD, Langenberg C, Rapsomaniki E, et al. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1·9 million people. Lancet Diabetes Endocrinol. 2015;3:105–113. doi: 10.1016/S2213-8587(14)70219-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lipska KJ, Yao X, Herrin J, et al. Trends in drug utilization, glycemic control, and rates of severe hypoglycemia, 2006–2013. Diabetes Care. 2017;40:468–475. doi: 10.2337/dc16-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The National Registry. Available from www.skatteetaten.no/en/person/National-Registry/. Accessed 23 Mar 2018
- 12.Statistics Norway. https://www.ssb.no/. Accessed 19 June 2018
- 13.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46:348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Lusignan S, Sadek N, Mulnier H, Tahir A, Russell-Jones D, Khunti K. Miscoding, misclassification and misdiagnosis of diabetes in primary care. Diabet Med. 2012;29:181–189. doi: 10.1111/j.1464-5491.2011.03419.x. [DOI] [PubMed] [Google Scholar]
- 15.Helsedirektoratet (2016) Helse-, omsorgs- og rehabiliteringsstatistikk. Eldres helse og bruk av kommunale helse- og omsorgstjenester [article in Norwegian]. Available from https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/1155/Helse,-omsorgs,-%20og%20rehabiliteringsstatistikk.%20Eldres%20helse%20og%20bruk%20av%20kommunale%20helse-%20og%20omsorgstjenester.%20IS-2375.pdf. Accessed 5 March 2018
- 16.Lewis JD, Bilker WB, Weinstein RB, Strom BL. The relationship between time since registration and measured incidence rates in the General Practice Research Database. Pharmacoepidemiol Drug Saf. 2005;14:443–451. doi: 10.1002/pds.1115. [DOI] [PubMed] [Google Scholar]
- 17.Sharma M, Nazareth I, Petersen I. Trends in incidence, prevalence and prescribing in type 2 diabetes mellitus between 2000 and 2013 in primary care: a retrospective cohort study. BMJ Open. 2016;6:e010210. doi: 10.1136/bmjopen-2015-010210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Read SH, Kerssens JJ, McAllister DA, et al. Trends in type 2 diabetes incidence and mortality in Scotland between 2004 and 2013. Diabetologia. 2016;59:2106–2113. doi: 10.1007/s00125-016-4054-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weng W, Liang Y, Kimball E, et al. Decreasing incidence of type 2 diabetes mellitus in the United States, 2007 to 2012: epidemiologic findings from a large US claims database. Diabetes Res Clin Pract. 2016;117:111–118. doi: 10.1016/j.diabres.2016.04.043. [DOI] [PubMed] [Google Scholar]
- 20.Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980-2012. JAMA. 2014;312:1218–1226. doi: 10.1001/jama.2014.11494. [DOI] [PubMed] [Google Scholar]
- 21.Norhammar A, Bodegård J, Nyström T, Thuresson M, Eriksson JW, Nathanson D. Incidence, prevalence and mortality of type 2 diabetes requiring glucose-lowering treatment, and associated risks of cardiovascular complications: a nationwide study in Sweden, 2006–2013. Diabetologia. 2016;59:1692–1701. doi: 10.1007/s00125-016-3971-y. [DOI] [PubMed] [Google Scholar]
- 22.Helsedirektoratet (2012) HbA1c som diagnostikum for diabetes [article in Norwegian]. Available from http://legeforeningen.no/Fagmed/Norsk-forening-for-medisinsk-biokjemi/Nyheter/20121/HbA1c-som-diagnostikum-ved-diabetes/. Accessed 16 Feb 2018
- 23.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Midthjell K, Lee CM, Langhammer A, et al. Trends in overweight and obesity over 22 years in a large adult population: the HUNT study, Norway. Clin Obes. 2013;3:12–20. doi: 10.1111/cob.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jacobsen BK, Aars NA. Changes in body mass index and the prevalence of obesity during 1994-2008: repeated cross-sectional surveys and longitudinal analyses. The Tromso study. BMJ Open. 2015;5:e007859. doi: 10.1136/bmjopen-2015-007859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Helse Bergen, Norwegian Quality Register for Bariatric Surgery. Available from https://www.kvalitetsregistre.no/registers/norsk-kvalitetsregister-fedmekirurgi. Accessed 5 Mar 2018
- 27.Sulo G, Igland J, Nygard O, Vollset SE, Ebbing M, Tell GS. Favourable trends in incidence of AMI in Norway during 2001-2009 do not include younger adults: a CVDNOR project. Eur J Prev Cardiol. 2014;21:1358–1364. doi: 10.1177/2047487313495993. [DOI] [PubMed] [Google Scholar]
- 28.Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2007;298:2654–2664. doi: 10.1001/jama.298.22.2654. [DOI] [PubMed] [Google Scholar]
- 29.Statistics Norway (2018) Snus more used than cigarettes. Available from https://www.ssb.no/en/helse/artikler-og-publikasjoner/snus-more-used-than-cigarettes. Accessed 23 Mar 2018
- 30.Sacerdote C, Ricceri F, Rolandsson O, et al. Lower educational level is a predictor of incident type 2 diabetes in European countries: the EPIC-InterAct study. Int J Epidemiol. 2012;41:1162–1173. doi: 10.1093/ije/dys091. [DOI] [PubMed] [Google Scholar]
- 31.Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40:804–818. doi: 10.1093/ije/dyr029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1196 kb)
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to data protection regulations.