Abstract
This study examined the relationships between chronic stress, food cravings, and body mass index. A community-based sample of adults (N = 619) completed a comprehensive assessment battery and heights and weights were measured. Chronic stress had a significant direct effect on food cravings, and food cravings had a significant direct effect on body mass index. The total effect of chronic stress on body mass index was significant. Food cravings partially mediated the relationship between chronic stress and body mass index. These findings are consistent with research that chronic stress may potentiate motivation for rewarding substances and behaviors and indicate that high food cravings may contribute to stress-related weight gain.
Keywords: body mass index, eating behaviors, food cravings, obesity, stress
Currently, 34.9 percent of adults in the United States are obese, and little progress has been made in reducing the number of individuals with this complex problem (Ogden et al., 2014). The increasing societal burden of obesity has prompted the development of numerous interventions for prevention and treatment. While these interventions are multifaceted and heterogeneous, with varied behavioral and biological targets, lifestyle modifications form the foundation of prevention and treatment options.
Obesity interventions are diverse in terms of delivery and duration, although the conventional cornerstones are dietary, physical activity, and behavioral changes (Jensen et al., 2013). Many obesity interventions focus on strategies to improve nutrition, increase physical activity, and decrease sedentary behavior (e.g. self-monitoring calorie intake, increasing fruit and vegetable intake, decreasing fat intake, goal setting pertaining to physical activity, and learning to read nutrition labels). Although there are a multitude of obesity interventions, many result in only modest and short-term improvements in weight (Lemmens et al., 2008; Seo and Sa, 2008).
There are multiple reasons why only modest and short-term improvements result from current obesity interventions, including the challenges of finding the correct fit between treatments and individuals. Solutions to this challenge require a more nuanced understanding of the mechanisms related to obesity. Studying mechanisms of behaviors is crucial to intervention development and enhancement. It can allow for amplification, optimization, and targeting of interventions to relevant processes. In addition, studying mechanisms can help advance what is known about a problem, develop solutions, and simplify complex interventions. One such relationship in which further clarification is needed is that between chronic stress and obesity.
Chronic stress and obesity
Stress is a complex and multidimensional concept referring to a real or perceived disruption in homeostasis (Chrousos and Gold, 1992). While there are some studies that demonstrate the relationship between increased stress and higher body mass index (BMI), the literature is mixed (Torres and Nowson, 2007; Wardle et al., 2011). This is partially due to the varying conceptualizations and measures of stress. While some focus on specific stress events (e.g. traumas, lay-offs, divorce; Udo et al., 2014), this study will focus on the role of chronic stress, the subjective experience of continuous stressors or ongoing life problems and hassles that can last for months to years (Turner and Lloyd, 1995).
While it is recognized that chronic stress is associated with obesity (Chen and Qian, 2012; Kouvonen et al., 2005; Wardle et al., 2011), the mechanisms underlying this process are unclear. There are several potential mechanisms that may contribute to the relationship between chronic stress and obesity including decreased physical activity, increased sedentary behavior, changes in stress-related hormones, changes in eating patterns, decreased sleep duration, and increased food cravings. The current study focuses on a possible mechanism in which there is a paucity of literature and that may provide beneficial knowledge for obesity intervention development: food cravings.
Stress and food cravings
The etiology of food craving, defined as an intense and specific desire to consume a certain food or food type that is difficult to resist (Weingarten and Elston, 1990, 1991), has generated much interest from the research community: multiple theories pertaining to the etiology of food cravings have been proposed. Physiological theories include those pertaining to nutritional and energetic homeostatic mechanisms and the psychoactive influences of components of craved foods on neurotransmitter systems (Pelchat, 2002). For example, some researchers have found that food deprivation increases food cravings (Massey and Hill, 2012) while others have found no relationship between food deprivation and cravings (Pelchat and Schaefer, 2000; Polivy et al., 2005). Learning theories posit that food cravings are conditioned to food-related cues. These may be emotional cues or external food cues such as a location or the smell or sight of a food (Jansen et al., 2011). Psychological and affect-based theories include the roles of mood and emotional states such as stress (Nijs et al., 2007; Rogers and Smit, 2000).
According to the Reward Based Stress Eating Model and Selye’s Theory of Stress, stress results in physiological responses to prepare the body to cope with stress, including activation of the hypothalamic–pituitary–adrenocortical (HPA) axis (Adam and Epel, 2007; Selye, 1956). Activation of the HPA axis results in the secretion of cortisol, a steroid hormone that regulates eating behaviors and choices (Pacák and Palkovits, 2001). Although acute stress typically results in decreased food intake, chronic activation of the HPA axis may result in the prolonged action of cortisol and a subsequent orexigenic response (Dallman et al., 2003; Torres and Nowson, 2007). This response may manifest as cravings for certain foods: neurobiological mechanisms related to stress may potentiate motivation and reward of highly palatable foods thus increasing food cravings and the risk for overeating (Sinha and Jastreboff, 2013). In prior studies, researchers have found that after HPA axis activation, there is an increase in sweet cravings in individuals with binge eating disorder (Rosenberg et al., 2013).
Food cravings and BMI
Food cravings are a commonly experienced phenomenon among the general population (Weingarten and Elston, 1991). Although not all food cravings are pathological, cravings are typically for foods that are high in fat, sugar, and carbohydrates such as chocolate, pizza, and fast foods (White et al., 2002). Researchers have also found that higher food cravings are associated with higher intake of respective food types craved and higher BMIs (Chao et al., 2014; Martin et al., 2008). Given the observed relationships among stress, food cravings, overeating, and BMI, it is possible that food cravings mediate the relationship between chronic stress and BMI.
The primary aim of this study was to examine the relationships between chronic stress, food cravings, and BMI. Based on prior literature, we hypothesized that food cravings would mediate the relationship between chronic stress and BMI.
Materials and methods
Design
The hypothesis was tested using a cross-sectional design from a large observational data set obtained from a collaborative, interdisciplinary set of studies that examined the effects of stress and self-control on the maladaptive behaviors of overeating, excessive alcohol use, and nicotine smoking.
Participants
The sample for this study is a convenience sample of adult men and women who were recruited from weekly advertisements in local newspapers and flyers at community centers and churches in and around New Haven, Connecticut. Participants include individuals from a variety of racial and socioeconomic backgrounds. Some individuals have the addictive behaviors of cigarette smoking, alcohol drinking, and/or overeating, while others do not engage in these behaviors. Inclusion criteria were that participants were between the ages of 18–50 years and were able to read English at least at the sixth-grade level. Exclusion criteria were dependence on any drug other than alcohol or nicotine, use of prescribed medications for any psychiatric disorders, pregnancy, and medical conditions that would preclude participation in the study (e.g. current cancer, type 1 diabetes, major head trauma). Study procedures were conducted at the Yale Stress Center, and participants received compensation for completion of assessment sessions.
The mean age of the sample was 29.55 (standard deviation (SD) = 9.06) years with a mean BMI of 27.42 (SD = 5.53) kg/m2. A little more than half (54.9%) of the sample was female. The sample was 67.0 percent White, 20.9 percent Black, and 12.2 percent “other.”
Procedures
The Yale University Institutional Review Board approved the parent study protocol. Potential participants completed an initial screening over the telephone or in person to determine eligibility based on inclusion and exclusion criteria. Following screening, eligible participants met with a research assistant for an intake session to obtain informed consent. Participants then completed an assessment battery including physical examinations, diagnostics, and cognitive and psychological assessments. Heights were collected using a height rod and weight was collected using a standard procedure.
Measures
Chronic stress.
Chronic stress was measured using the chronic stress subscale of the Cumulative Adversity Interview (Turner and Lloyd, 1995). The Cumulative Adversity Interview is a well-established, 140-item interview that assesses for the accumulation of stressful life events over a lifetime. The chronic stress subscale consists of 62 items relating to the subjective experience of continuous stressors or ongoing life problems and hassles. Items are on a 3-point Likert-type scale ranging from not true to very true and refer to perceived difficulties with ongoing interpersonal, social, and financial relationships and responsibilities including difficulties in the work and home environment and relationships with family and significant others. A 3-month test–retest reliability for the chronic stress subscale was .79 (Ansell et al., 2012). The use of interview techniques is recommended to decrease participant recall bias (Dohrenwend et al., 2006).
Food cravings.
Food cravings were measured using the Food Craving Inventory (FCI; White et al., 2002). The FCI is a 28-item self-report measure that assesses general and specific types (high fat foods, complex carbohydrates/starches, sweets, and fast-food fats) of food cravings. Participants are asked to rate how often each food was craved over the past month using a 5-point Likert-type scale ranging from 1 (never) to 5 (always/almost every day; White et al., 2002). The FCI has established content validity from experts in the field of eating behaviors (White et al., 2002). Concurrent validity has been established with the Conceptual Craving Scale (Hill et al., 1991) and disinhibition and hunger scales of the Three-Factor Eating Questionnaire (TFEQ; Stunkard and Messick, 1985), and discriminant validity with the restraint scale of the TFEQ. The FCI has demonstrated acceptable internal consistency reliability and test–retest reliability in adults (White et al., 2002) as well as diverse community and clinical samples (Barnes and Tantleff-Dunn, 2010; Barnes and White, 2010; White and Grilo, 2005). In the current study, Cronbach’s alpha was .93 for general food cravings.
BMI.
BMI was calculated from measured heights and weight using the formula weight (kg)/[height (m)]2.
Age, gender, race/ethnicity.
Age, gender, and race/ethnicity were assessed using a demographic questionnaire designed for this study.
Statistical analysis
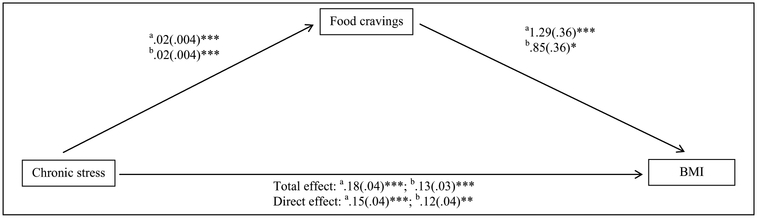
We calculated descriptive statistics and examined the bivariate associations using Pearson’s correlations for continuous variables, point-bise-rial correlations for a dichotomous and continuous variable, and phi coefficients for two dichotomous variables. To test our primary hypothesis, we used a mediation analysis with bootstrapping as recommended by Preacher and Hayes (2008). We used the SPSS macro provided by Preacher and Hayes (2008) to calculate direct and indirect effects using 1000 bootstrap samples and a 95 percent confidence interval. For the mediation model (Figure 1), chronic stress was the independent variable, food cravings (FCI total score) was the mediator variable, and BMI was the dependent variable. All models were estimated with and without adjusting for age, gender, and race/ethnicity.
Figure 1.
Food cravings mediate the effect of chronic stress on body mass index (BMI; n = 619). Unstandardized coefficients are provided. Total effect = effect of chronic stress on BMI. Direct effect = effect of chronic stress on BMI after controlling for food cravings.
aUnadjusted.
bAdjusted for age, gender, and race/ethnicity.
*p < .05; **p < .01; ***p < .001.
Results
Descriptive statistics
The mean score on the chronic stress subscale was 10.03 (SD = 5.93) and the mean of the food cravings (FCI) total score was 1.95 (SD = 0.62). Almost all participants (97.9%) endorsed having at least one food craving over the past month.
Correlations
The correlations between study variables are shown in Table 1. Chronic stress was positively correlated with food cravings, BMI, age, and Black race/ethnicity (r(617) = .14 to .24, p < .001) and negatively correlated with White race/ethnicity and being male (r(617) = −.24 and −.14, p < .001, respectively). Food cravings were positively correlated with BMI, age, and Black race/ethnicity (r(617) = .12 to .28, p < .001) and negatively associated with White race/ethnicity (r(617) = −.27, p < .001).
Table 1.
Correlations among study variables (n = 619).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Chronic stress | – | ||||||
| 2. Food cravings | .24** | – | |||||
| 3. BMI | .19** | .18** | – | ||||
| 4. Age | .14** | .12** | .21** | – | |||
| 5. White | −.24** | −.27** | −.17** | −.05 | – | ||
| 6. Black | .20** | .28** | .22** | .13** | −.73** | – | |
| 7. Male | −.14** | −.05 | .03 | −.02 | .09* | −.04 | – |
BMI = body mass index.
The following statistics were used: Pearson correlations for continuous variables, point-biserial correlations for a dichotomous and continuous variable, and phi coefficients for two dichotomous variables.
p < .05
p < .001.
Mediation analysis
Results from the bootstrapped analysis supported the hypothesis that food cravings mediate the relationship between chronic stress and BMI. Figure 1 displays the mediation models with and without adjusting for age, gender, and race/ethnicity. Unadjusted results demonstrated that chronic stress had a significant direct effect on food cravings (B = .03 ± .004; p < .001), and food cravings had a significant direct effect on BMI (B = 1.29 ± .36, p < .001). The total effect of chronic stress on BMI was significant (B = .18 ± .04, p < . 001). Food cravings partially mediated the relationship between chronic stress and BMI (effect of chronic stress on BMI controlling for food cravings was B = .15 ± .04, p < .001; unadjusted, bootstrapped 95 percent bias-corrected confidence interval of .01 to .06). Both unadjusted and adjusted confidence intervals exclude 0, suggesting mediation (Preacher and Hayes, 2008).
Discussion
These findings from a large and diverse community sample of adults support our hypothesis that food cravings statistically mediate the relationship between chronic stress and increased BMI albeit the effect size was small. To our knowledge, this is one of the first studies to examine the role of food cravings as a statistical mediator of this relationship. These results serve to generate hypotheses about possible mechanisms underlying the association between chronic stress and BMI and demonstrate the potential effect of food cravings in this relationship.
This work supports the Reward Based Stress Eating Model and Selye’s Theory of Stress (Adam and Epel, 2007; Selye, 1956) and builds upon previous research exploring eating-related correlates and mechanisms related to chronic stress and BMI. Researchers have found that stress-related eating is associated with greater preference for calorie-dense and highly palatable foods (Dallman, 2010; Epel et al., 2004; Laitinen et al., 2002). Furthermore, stress has been shown to potentiate brain motivation and habit regions that are active under craving for high calorie foods (Page et al., 2011; Pelchat et al., 2004). Thus, we have posited that stress and brain food and reward circuits overlap significantly and stress potentiates food craving via activation of habit-based circuits as in other types of addictions (Sinha and Jastreboff, 2013). Our results are in concordance with this research as well as research demonstrating that perceived stress and chronic stressor exposure are associated with an increased drive to eat as measured by disinhibition, hunger, binge eating, and palatable, non-nutritious food consumption (Groesz et al., 2012). Our findings support this relationship and add to the literature by demonstrating the relationship with food cravings. Food cravings are differentiated from other constructs such as hunger and food consumption as a food craving is a subjective experience that is intense and specific for a certain food (Hill, 2007; White et al., 2002). Although food cravings are associated with increased consumption of craved foods (Chao et al., 2014; Martin et al., 2008), food cravings are not synonymous with increased consumption, and food cravings can occur in the absence of hunger (Hill, 2007; Weingarten and Elston, 1990).
Few studies have examined mediators and mechanisms relating chronic stress to increased BMI. Aligning with our results, researchers have suggested that among older adults, poor health habits (i.e. low physical activity, high sedentary activity, and unhealthy dietary intake) mediate the relationship between chronic stress and the metabolic syndrome (Vitaliano et al., 2002). Our results also align with findings from basic research demonstrating the role of reward circuitry and hedonic mechanisms in the consumption of unhealthy foods and obesity (Corwin et al., 2011; Finlayson et al., 2007; Jastreboff et al., 2013; Patterson and Abizaid, 2013).
Given the suggestion that there are differences in stress and obesity by gender and race/ethnicity, it is of note that although there was some attenuation, the statistical mediation remained after controlling for these factors. Researchers have demonstrated that the relationships between stress, weight gain, and obesity are stronger in women than men (Laitinen et al., 2002; Sinha and Jastreboff, 2013; Udo et al., 2014). There is evidence indicating that in comparison to Whites, Blacks have higher levels of stress (Geronimus et al., 2006; Troxel et al., 2003) and obesity (Ogden et al., 2014). Our results suggest that food cravings may be an important factor accounting for the relationship between stress and obesity across these groups.
The results of this study must be interpreted in light of several limitations. First, this study was cross-sectional and non-experimental; thus, causality and temporality cannot be inferred. The cross-sectional nature of these data does not allow us to discriminate between our hypothesis and alternative hypotheses. Additionally, alternative hypotheses were not tested statistically as the FCI assesses food craving over the past month whereas the Cumulative Adversity Interview assesses chronic stress over months to years. Thus, the results from this analysis would not have been theoretically valid (Iacobucci et al., 2007). Longitudinal and experimental studies are necessary to provide more insight into the directionality of these relationships and alternative models cannot be ruled out. Second, despite the diversity and size of the sample, a convenience sampling approach was used which may limit generalizability. Third, there are several potential mechanisms that may contribute to the relationship between stress and obesity-related metabolic abnormalities including behavioral changes in eating behaviors and physical activity, sympathetic nervous system activation, and changes in HPA axis function (De Vriendt et al., 2009; Kyrou and Tsigos, 2009).
Previous work has established that chronic stress is associated with increased BMI, but to our knowledge, this study is one of the first studies to propose and demonstrate that food cravings statistically mediate this relationship. These findings suggest that creating interventions to help adults cope with stress and with food cravings may help them attain a healthier weight. Further longitudinal and experimental studies as well as exploration of behavioral and physiological mechanisms related to chronic stress, food cravings, and BMI are needed.
Acknowledgements
The authors gratefully acknowledge all participants in this study and research staff. The authors would also like to thank their funding sources. Study concept and design: A.C., C.M.G., M.A.W., R.S. Acquisition and collection of data: R.S. Analysis of data: A.C. Obtained funding for study: R.S. Administrative, technical, and material support: R.S. All authors were involved in writing and revising the article and provided final approval of the article.
Funding
This study was funded by The National Institute on Drug Abuse/National Institute of Health (NIH) grants PL1-DA024859 and UL1-DE019859. A.C. was funded by pre-doctoral fellowships from the Jonas Center for Nursing Excellence and the National Institute of Nursing Research/NIH (T32-NR00834610; F31-NR014375). C.M.G. was funded, in part, by NIDDK/NIH (K24-DK070052).
References
- Adam TC and Epel ES (2007) Stress, eating and the reward system. Physiology & Behavior 91(4): 449–458. [DOI] [PubMed] [Google Scholar]
- Ansell EB, Rando K, Tuit K, et al. (2012) Cumulative adversity and smaller gray matter volume in medial prefrontal, anterior cingulate, and insula regions. Biological Psychiatry 72(1): 57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes RD and Tantleff-Dunn S (2010) Food for thought: Examining the relationship between food thought suppression and weight-related outcomes. Eating Behaviors 11(3): 175–179. [DOI] [PubMed] [Google Scholar]
- Barnes RD and White MA (2010) Psychometric properties of the food thought supression inventory in men. Journal of Health Psychology 15(7): 1113–1120. [DOI] [PubMed] [Google Scholar]
- Chao A, Grilo CM, White MA, et al. (2014) Food cravings, food intake, and weight status in a community-based sample. Eating Behaviors 15(3): 478–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y and Qian L (2012) Association between lifetime stress and obesity in Canadians. Preventive Medicine 55(5): 464–467. [DOI] [PubMed] [Google Scholar]
- Chrousos GP and Gold PW (1992) The concepts of stress and stress system disorders. Overview of physical and behavioral homeostasis. JAMA: Journal of the American Medical Association 267(9): 1244–1252. [PubMed] [Google Scholar]
- Corwin RL, Avena NM and Boggiano MM (2011) Feeding the reward: Perspectives from three rat models of binge eating. Physiology & Behavior 104(1): 87–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallman MF (2010) Stress-induced obesity and the emotional nervous system. Trends in Endocrinology and Metabolism 21: 159–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallman MF, Pecoraro N, Akana SF, et al. (2003) Chronic stress and obesity: A new view of “comfort food.” Proceedings of the National Academy of Sciences of the United States of America 100(20): 11696–11701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vriendt T, Moreno LA and De Henauw S (2009) Chronic stress and obesity in adolescents: Scientific evidence and methodological issues for epidemiological research. Nutrition, Metabolism, and Cardiovascular Diseases 19(7): 511–519. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP (2006) Inventorying stressful life events as risk factors for psychopathology: Toward resolution of the problem of intracategory variability. Psychological Bulletin0 132(3): 477–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epel ES, Jimenez S, Brownell K, et al. (2004) Are stress eaters at risk of metabolic syndrome? Annals of the New York Academy of Sciences 1032: 208–210. [DOI] [PubMed] [Google Scholar]
- Finlayson G, King N and Blundell JE (2007) Liking vs. wanting food: Importance for human appetite control and weight regulation. Appetite 31(7): 987–1002. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keen D, et al. (2006) “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health 96(6): 826–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groesz L, McCoy S, Carl J, et al. (2012) What is eating you? Stress and the drive to eat. Appetite 58(2): 717–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill AJ, Weaver CF and Blundell JE (1991) Food craving, dietary restraint and mood. Appetite 17: 187–197. [DOI] [PubMed] [Google Scholar]
- Hill AJ (2007) The psychology of food craving. Proceedings of the Nutrition Society 66: 277–285. [DOI] [PubMed] [Google Scholar]
- Iacobucci D, Saldanha N and Deng X (2007) A mediation on mediation: Evidence that structural equation models perform better than regressions. Journal of Consumer Psychology 17(2): 140–154. [Google Scholar]
- Jansen A, Havermans RC and Nederkoorn C (2011) Cued overeating In: Preedy VR, Watson RR and Martin CR (eds) Handbook of Behavior, Food and Nutrition. New York: Springer, pp. 1431–1443. [Google Scholar]
- Jastreboff AM, Sinha R, Lacadie C, et al. (2013) Neural correlates of stress- and food cue-induced food cravings in obesity. Diabetes Care 36(2): 394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MD, Ryan DH, Hu FB, et al. (2013) 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults. Circulation 129: S102–S138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouvonen A, Kivimäki M, Cox SJ, et al. (2005) Relationship between work stress and body mass index among 45,810 female and male employees. Psychosomatic Medicine 67(4): 577–583. [DOI] [PubMed] [Google Scholar]
- Kyrou I and Tsigos C (2009) Stress hormones: Physiological stress and regulation of metabolism. Current Opinion in Pharmacology 9(6): 787–793. [DOI] [PubMed] [Google Scholar]
- Laitinen J, Ek E and Sovio U (2002) Stress-related eating and drinking behavior and body mass index and predictors of this behavior. Preventive Medicine 34: 29–39. [DOI] [PubMed] [Google Scholar]
- Lemmens V, Oenema A, Klepp KI, et al. (2008) A systematic review of the evidence regarding efficacy of obesity prevention interventions among adults. Obesity Reviews 9(5): 446–455. [DOI] [PubMed] [Google Scholar]
- Martin CK, O’Neil PM, Tollefson G, et al. (2008) The association between food cravings and consumption of specific foods in a laboratory taste test. Appetite 51(2): 324–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey A and Hill AJ (2012) Dieting and food craving. A descriptive, quasi-prospective study. Appetite 58(3): 781–785. [DOI] [PubMed] [Google Scholar]
- Nijs IM, Franken IH and Muris P (2007) The modified trait and state food-cravings questionnaires: Development and validation of a general index of food craving. Appetite 49(1): 38–46. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, et al. (2014) Prevalence of childhood and adult obesity in the United States, 2011–2014. JAMA: Journal of the American Medical Association 311(8): 806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacák K and Palkovits M (2001) Stressor specificity of central neuroendocrine responses: Implications for stress-related disorders. Endocrine Reviews 22(4): 502–548. [DOI] [PubMed] [Google Scholar]
- Page KA, Seo D, Belfort-DeAguiar R, et al. (2011) Circulating glucose levels modulate neural control of desire for high-calorie foods in humans. Journal of Clinical Investigation 121(10): 4161–4169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson ZR and Abizaid A (2013) Stress induced obesity: Lessons from rodent models of stress. Frontiers in Neuroscience 7: 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelchat ML (2002) Of human bondage: Food craving, obsession, compulsion, and addiction. Physiology & Behavior 76(3): 347–352. [DOI] [PubMed] [Google Scholar]
- Pelchat ML and Schaefer S (2000) Dietary monotony and food cravings in young and elderly adults. Physiology & Behavior 68(3): 353–359. [DOI] [PubMed] [Google Scholar]
- Pelchat ML, Johnson A, Chan R, et al. (2004) Images of desire: Food-craving activation during fMRI. NeuroImage 23(4): 1486–1493. [DOI] [PubMed] [Google Scholar]
- Polivy J, Coleman J and Herman CP (2005) The effect of deprivation on food cravings and eating behavior in restrained and unrestrained eaters. International Journal of Eating Disorders 38(4): 301–309. [DOI] [PubMed] [Google Scholar]
- Preacher KJ and Hayes AF (2008) Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods 40(3): 879–891. [DOI] [PubMed] [Google Scholar]
- Rogers PJ and Smit HJ (2000) Food craving and food “addiction”: A critical review of the evidence from a biopsychosocial perspective. Pharmacology Biochemistry and Behavior 66(1): 3–14. [DOI] [PubMed] [Google Scholar]
- Rosenberg N, Bloch M, Avi IB, et al. (2013) Cortisol response and desire to binge following psychological stress: Comparison between obese subjects with and without binge eating disorder. Psychiatry Research 208(2): 156–161. [DOI] [PubMed] [Google Scholar]
- Selye H (1956) The Stress of Life. New York: McGraw-Hill. [Google Scholar]
- Seo DC and Sa J (2008) A meta-analysis of psycho-behavioral obesity interventions among US multiethnic and minority adults. Preventive Medicine 47(6): 573–582. [DOI] [PubMed] [Google Scholar]
- Sinha R and Jastreboff AM (2013) Stress as a common risk factor for obesity and addiction. Biological Psychiatry 73(9): 827–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stunkard AJ and Messick S (1985) The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research 29(1): 71–83. [DOI] [PubMed] [Google Scholar]
- Torres SJ and Nowson CA (2007) Relationship between stress, eating behavior, and obesity. Nutrition 23(11–12): 887–894. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Bromberger JT, et al. (2003) Chronic stress burden, discrimination and subclinical carotid artery disease in African American and Caucasian women. Health Psychology 22(3): 300–309. [DOI] [PubMed] [Google Scholar]
- Turner RJ and Lloyd DA (1995) Lifetime traumas and mental health: The significance of cumulative adversity. Journal of Health and Social Behavior 36(4): 360–376. [PubMed] [Google Scholar]
- Udo T, Grilo CM and McKee SA (2014) Gender differences in the impact of stressful life events on changes in body mass index. Preventive Medicine 69: 49–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitaliano PP, Scanlan J, Zhang J, et al. (2002) A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosomatic Medicine 64(3): 418–435. [DOI] [PubMed] [Google Scholar]
- Wardle J, Chida Y, Gibson EL, et al. (2011) Stress and adiposity: A meta-analysis of longitudinal studies. Obesity 19(4): 771–778. [DOI] [PubMed] [Google Scholar]
- Weingarten HP and Elston D (1990) The phenomenology of food cravings. Appetite 15(3): 231–246. [DOI] [PubMed] [Google Scholar]
- Weingarten HP and Elston D (1991) Food cravings in a college population. Appetite 17(3): 167–175. [DOI] [PubMed] [Google Scholar]
- White MA and Grilo CM (2005) Psychometric properties of the food craving inventory among obese patients with binge eating disorder. Eating Behaviors 6(3): 239–245. [DOI] [PubMed] [Google Scholar]
- White MA, Whisenhunt BL, Williamson DA, et al. (2002) Development and validation of the food-craving inventory. Obesity 10(2): 107–114. [DOI] [PubMed] [Google Scholar]