Abstract
Background
An impact of regular physical activity (RPA) on the abdominal muscles may be significant when comparing various symptomatic groups. However, there is lack comprehensive information in this field. The objective of this study was to assess the lateral abdominal wall at rest and during abdominal drawing-in manoeuvre in adolescent physically active girls in different body positions.
Methods
One hundred and forty-four female students, 13–17 years of age, participated in the study. Participants were divided into 2 groups based on a physical activity (PA) statement. Measurements of the thickness of the abdominal muscles at rest and during abdominal drawing-in manoeuvre were made in the supine and standing positions by ultrasound imaging.
Results
Compared to the control group, activities of the obliquus internus and transversus abdominis muscles were higher in the regular PA group by 8.9% (95%CI: 3.1–14.7) and 36% (95%CI: 19.1–47.5), respectively. In the RPA group, the transversus abdominis preferential activation ratio was greater by 0.03 (95%CI: 0.01–0.04), and the contraction ratio was greater by a mean value of 0.35 (95%CI: 0.18–0.46).
Conclusion
RPA does not have any effect on the resting thickness of the abdominal muscles in the supine and standing positions. Girls performing RPA have a greater ability to perform an independent activation and greater contractions of the transversus abdominis.
Keywords: External oblique abdominis, Internal oblique abdominis, Physical activity, Transversus abdominis, Ultrasound
1. Introduction
The lateral wall of the abdomen is built of the transversal abdominal (TrA), abdominal oblique internal (OI), and abdominal oblique external (OE) muscle. Of these abdominal muscles, the greatest role is ascribed to the TrA, which, together with the posterior portion of the OI, is part of a deep cylinder providing stability for the lumbar spine.1, 2 Involuntary action of these muscles is associated with the protective lumbar spine mechanism,3 which is disturbed in adults with low back pain (LBP).4, 5 Currently, imaging ultrasonography (USI), a reliable and valid technique, most often used by therapists and investigators, is employed for the evaluation of structure, function, and activities of the abdominal muscles.6, 7 The measurements obtained by USI are similar to those obtained by magnetic resonance imaging and correlate well with electromyography.8, 9
A potentially important role of the abdominal muscle in the stabilisation of the lumbar spine made many researchers analyse the characteristics of these muscles in healthy and LBP population.4, 10, 11, 12, 13, 14, 15 In these reports, in addition to the evaluation of the muscle thickness at rest, the authors studied the activity of the abdominal muscles during the “abdominal drawing-in manoeuvre” (ADIM), which is used to evaluate the TrA function.7 Moreover, the researchers evaluated possible effects of sex, age, height, body weight, body mass index (BMI), and hand dominance in search for variables that can affect the USI of the abdominal muscles at rest and during ADIM.10, 13, 16 However, in studies of the adult population, in professional cricket players, the TrA and OI are thicker than in the normal population.8 Thus, the effect of physical activity (PA) on theabdominal muscles may be significant when comparing various symptomatic groups. However, we do not have full information on this subject. The results for the TrA contraction ratio (TrA during ADIM/TrA at rest) are also somewhat inconsistent because in some studies of healthy adults, this factor is approximately 1.5,10, 17 and in others 1.8.16 In these studies, the authors did not provide the level of PA of the persons studied; however, all participants in the study of Springer et al.16 were from the department of defence, and probably their level of PA was greater than average. This may explain the differences in the results.
Recently, Linek et al.18 indicated lower thickness of the TrA, OI, and OE on both sides of the body in children and adolescents with scoliosis. The mean values of the abdominal muscle thickness obtained in other studies in scoliosis patients do not seem to confirm it.19 The easiest way to explain such difference in the thickness of the abdominal muscles is the different types and severity of scoliosis in both mentioned studies. However, it also may be that in the paper by Linek et al.,18 the population free of scoliosis (control group) was more physically active than population with scoliosis, and this may explain the difference in muscle thickness at rest between the control and experimental groups, as was observed in professional cricket players.8 Taking into consideration a growing interest in abdominal muscles in children and adolescents, at this state of the studies, in addition to the assessment of the height, body mass, or BMI on the thickness of the abdominal muscles,20 it is necessary to evaluate the effect of regular PA (RPA) on the OE, OI, and TrA at rest and during ADIM in adolescents. Such information will allow more controlled planning of future studies on adolescents.
The studies to date demonstrate that women also activate the TrA much better during ADIM,10 which points to a greater role of this muscle in motor control in women.10, 16 The studies also clearly show that adolescent girls are more sensitive to LBP21, 22 and scoliosis.23 Thus, abnormalities in the TrA can have a greater effect on the condition of the musculoskeletal system in females. Longitudinal studies clearly demonstrate that in female athletes, with improper motor control of the trunk, the incidence of knee injuries is higher.24, 25 Hides and Stanton26 pointed out a possible negative impact of sports on the TrA. Thus, taking into consideration a greater role of TrA in females and the possible negative effect of sports on its characteristics, the authors attempted to determine the effect of RPA on the characteristics of the muscles of the lateral wall of the abdomen in teenage girls at rest and during ADIM and in different body positions (supine, standing).
2. Methods
2.1. Participants
A total of 144 female students of middle school and subsequent levels, 13–17 years of age, participated in the study. Prior to qualifying an individual for the study, a preliminary selection was performed, during which body posture was evaluated and a short medical history of a given person was taken. Thus, in each individual, external signs of scoliosis were evaluated and/or other abnormalities in body posture. For this purpose, Adams' test was performed and a scoliometer was used for the evaluation of the body rotation. Adams' test and a scoliometer are widely used for the evaluation of body rotation and scoliosis, as well as in clinical studies on children with scoliosis.27, 28 The intra-rater reliability of axial trunk rotation measures measured by the scoliometer was very good and excellent for the upper, medium, and lower thorax and lumbar segments.29 Based on this examination, only the subjects in whom no body rotation angle was detected (the acceptable range of trunk rotation measured with the scoliometer was between 0° and 3°) were included. Moreover, based on an interview, the following girls were excluded: (a) in whom any surgical procedure was performed in the chest, the abdominal cavity, the pelvic girdle, and/or the spine; (b) with chronic cardiovascular/respiratory system disease; (c) who experienced an illness and/or trauma that was associated with a prolonged (>14 days) hospitalisation or immobilisation during a period of 2 years prior to the study; (d) who experienced pain in the spine, pelvic girdle or lower limbs during 3 months preceding the study; (e) who took medications that may affect the function of the nervous and muscular systems within 1 year preceding the study.
Finally, each subject responded to questions about current and past PAs. This was the basis for dividing subjects into 2 groups. The individuals who currently do not perform RPA were included in the first (control) group (n = 74). The individuals who stated that they belonged to a sport club, and therefore regularly practice a specific sport discipline or activity, were included in the second group (RPA group, n = 70). A statement that a person has regularly been performing RPA for at least 2 years was a condition for the inclusion in the RPA group, and a statement that a person has not been performing RPA for at least 2 years was a condition for inclusion in the control group. RPA is interpreted as performance of a particular sports discipline or activity at least twice a week (with the exception of off-season periods).
The study conformed to the standards set by the Declaration of Helsinki and was approved by the Bioethics Committee for Scientific Studies at The Jerzy Kukuczka Academy of Physical Education in Katowice, Poland. All participants and their parents received verbal and written information about all procedures and gave their signed informed consent to participate.
2.2. Procedures
The ultrasound scanning procedures were performed by 1 investigator. The entire procedure, the sequence of measurements, and the instructions were identical for all study participants.
A real-time ultrasound B-scanner (MINDRAY DP-6600 Digital Ultrasonic Diagnostic Imaging System; Medical Corp., Redmond, WA, USA) with a 60 mm wide 75L38EA linear array transducer (5.0/7.5/10 MHz) was used to obtain images of the abdominal muscles. The penetration depth was 5.39 cm at a sampling frequency of 7.5 MHz. The transducer was always placed on the anterolateral wall of the abdomen, between the iliac crest and the costal margin, perpendicular to the longitudinal axis of the body. It was finally adjusted to ensure that, at rest, the fascial borders of the 3 muscles (TrA, OI, OE) appeared parallel on the screen. Individuals with an unclear ultrasound image of the abdominal muscle (mainly obese) were excluded from the study.
Measurements of the thickness of the muscles OE, OI, and TrA at rest were made in the supine and standing positions. In the supine position the knees of the examined individuals were extended and the upper limbs were placed along the sides of the trunk. While standing, the subjects were asked to keep straight and relaxed, and to place equal weight on lower limbs. The thickness of the muscles at rest was stored in at the end of normal expiration. The thickness of the muscles at ADIM was measured in the same positions, after giving the same instructions to each person examined. The instructions included an explanation of the manoeuvre that was required of them.30 Next, all participants had the opportunity to perform 1 trial without the USI control (in order to check whether the exercise was properly performed, but not for feedback).
At rest and during ADIM, 3 consecutive measurements were performed alternately for each side, always starting with the right side. Therefore, each person had to perform the ADIM 6 times in each body position. To evaluate the reliability of the measurements, in 20 randomly selected subjects, a second series (identical to the first one) of abdominal muscle measurements was performed.
All pictures obtained were saved in an external medium, transferred to a computer where they were further processed using Photoshop software (Adobe Systems Inc., San Jose, CA, USA), which had earlier been used for the evaluation of the thickness of the muscles.31 In this work, each picture was enlarged (300%), made brighter, contrast was added, and horizontal and vertical lines were inserted to increase the accuracy of the measurements. The vertical marking line positioned 15 mm from the left and right musculofascial junction of the TrA (the location for the first vertical line) was consistently used to re-measure the thickness for each muscle. The vertical distance between the musculofascial layers represented individual thickness of the OE, OI, and TrA. Fig. 1 clearly illustrates the methods used to measure OE, OI, and TrA muscle thickness at rest and during ADIM on both sides of the body. A person performing measurements and a person analysing ultrasounds did not know in which group a given subject was included.
Fig. 1.
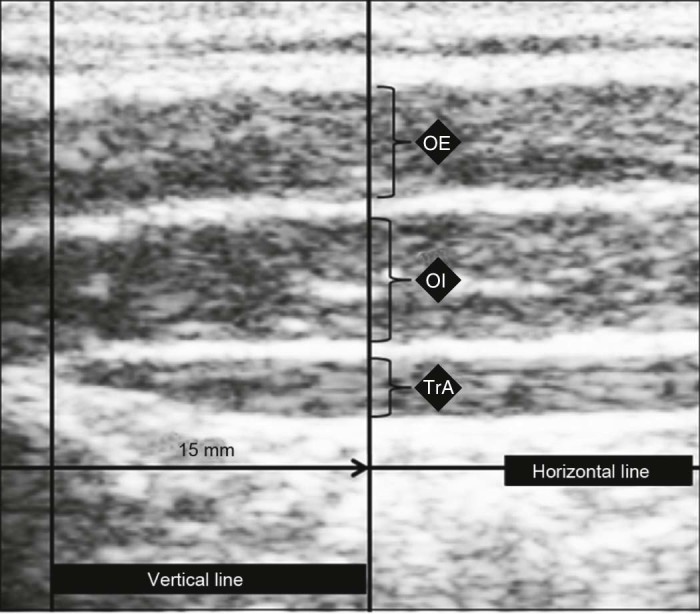
Ultrasound measurement procedure of the abdominal muscles. OE = external oblique abdominis; OI = internal oblique abdominis; TrA = transversus abdominis.
2.3. Outcome measures
The mean of 3 measurements of the OE, OI, and TrA obtained from the USI was used for the analysis of the measurements performed separately for the right and left sides of the body, both in the resting position and during ADIM (supine and standing positions, separately). In this study, the thickness of the muscle during ADIM was normalised with the thickness produced during the resting position (Eq. (1)). The calculation gave the percentage change in the thickness of all listed abdominal muscles during ADIM. In this study, for the TrA 2 indices were also calculated (Eqs. (2) and (3)).15
| (1) |
| (2) |
| (3) |
2.4. Data analysis
An intraclass correlation coefficient (ICC) was calculated to assess intra-rater reliability (ICC3,k) of each muscle thickness measurement.32 In addition, the smallest detectable differences () were calculated for each measurement. Differences in demographic data between control and sport groups were examined using an independent sample t test. USG data, thickness change, resting thickness, and TrA ratio were analysed using an analysis of variance (ANOVA), with between subjects factor being group (control vs. sport) and within subjects factor being body side (right side vs. left side). The analysis was conducted separately for the supine and standing positions. The results were presented as a mean difference and 95% confidence interval (CI). For all analyses, the threshold of the p value considered as significant was set at <0.05.
3. Results
3.1. Participants
Comparative analysis between RPA group and control group did not demonstrate any statistically significant differences in terms of height, body weight, or age. The complete characteristics of the study population, divided into groups, are presented in Table 1. The complete list of sports disciplines in the RPA group, along with the practice time, is shown in Table 2.
Table 1.
The mean ± SD of groups and the mean differences between groups and the t test result for independent samples.
| Characteristic | Group | Difference between groups | ||
|---|---|---|---|---|
| Control (n = 74) | RPA (n = 70) | Controls—RPA (95%CI) | t testa | |
| Age (year) | 15.32 ± 1.17 | 15.19 ± 1.84 | 0.18(−0.33to0.71) | 0.69 |
| Weight(kg) | 57.14 ± 10.11 | 56.42 ± 9.11 | 0.72(−2.61to4.06) | 0.42 |
| Height(cm) | 159.21 ± 24.67 | 164.33 ± 8.31 | −4.99(−11.6to1.64) | −1.49 |
Abbreviations: CI = confidence interval; RPA = regular physical activity.
In all cases p > 0.05.
Table 2.
Classification and incidence and the mean years of practice sport in regular physical activity group (mean ± SD).
| Sport type | No. of subjects (%) | Time (year) |
|---|---|---|
| Volleyball | 35(50.0) | 3.33 ± 1.17 |
| Dance | 16(22.8) | 7.18 ± 4.55 |
| Ski | 8(11.4) | 4.20 ± 1.20 |
| Run | 5(7.1) | 2.50 ± 1.10 |
| Swim | 4(5.8) | 3.00 ± 0.00 |
| Badminton | 2(2.9) | 3.00 ± 0.00 |
3.2. Reliability study
The intra-rater ICC3,3 values (n = 20) and the SDD for all of the lateral abdominal muscles were presented in Table 3.
Table 3.
Mean estimates of intra-rater reliability.
| Muscle state | Supine position | Standing position | ||
|---|---|---|---|---|
| ICC | SDDa | ICC | SDDa | |
| OE | ||||
| Rest | 0.96 | 0.60 | 0.97 | 0.65 |
| ADIM | 0.70 | 20.53 | 0.85 | 21.52 |
| OI | ||||
| Rest | 0.98 | 0.45 | 0.96 | 0.89 |
| ADIM | 0.82 | 18.93 | 0.87 | 23.74 |
| TrA | ||||
| Rest | 0.98 | 0.30 | 0.96 | 0.54 |
| ADIM | 0.84 | 29.79 | 0.81 | 36.59 |
Abbreviations: ADIM = % change during abdominal drawing-in manoeuvre; ICC = intraclass correlation coefficient; OE = external oblique abdominis; OI = internal oblique abdominis; SDD = the smallest detectable differences; TrA = transversus abdominis.
Rest in millimetre but ADIM in percent.
3.3. Thickness at rest
For the supine position, statistically significant side-to-side thickness differences were noted only in case of the OE and OI. The data showed that, irrespective of a group studied (control or RPA), the OE and OI on the left side were thicker by 0.53 mm (95%CI: 0.15–0.92) and 0.86 mm (95%CI: 0.33–1.40), respectively. No such observation was made in the standing position (Table 4).
Table 4.
Mean ± SD (95%CI) values of abdominal muscle size at rest and during ADIM in supine and standing positions in RPA and control groups.
| Control group | RPA group | p value from ANOVA | |||||
|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Main effect | Interaction | ||
| Group | Side | ||||||
| OE | |||||||
| Rest (mm) | |||||||
| Supine | 4.19 ± 0.88(3.90to4.48) | 4.84 ± 1.12(4.47to5.22) | 4.36 ± 1.29(3.87to4.85) | 4.73 ± 1.27(4.26to5.21) | 0.87 | 0.01* | 0.48 |
| Standing | 5.28 ± 1.01(4.94to5.61) | 4.81 ± 1.06(4.45to5.16) | 5.33 ± 1.72(4.67to5.98) | 5.01 ± 1.41(4.49to5.54) | 0.57 | 0.09 | 0.73 |
| ADIM(%) | |||||||
| Supine | 2.37 ± 11.10(−1.30to6.08) | −4.60 ± 16.90(−10.20to1.03) | 1.27 ± 19.30(−6.10to8.64) | −1.08 ± 18.10(−7.90to5.70) | 0.67 | 0.11 | 0.42 |
| Standing | 0.74 ± 18.10(−5.30to6.80) | −1.09 ± 18.40(−7.23to5.05) | 5.24 ± 31.50(−6.75to17.20) | 6.29 ± 34.10(−6.45to19.00) | 0.19 | 0.93 | 0.75 |
| OI | |||||||
| Rest(mm) | |||||||
| Supine | 6.28 ± 1.24(5.87to6.70) | 7.35 ± 2.09(6.65to8.04) | 6.22 ± 1.20(5.76to6.67) | 6.83 ± 1.41(6.30to7.36) | 0.28 | <0.001* | 0.40 |
| Standing | 7.46 ± 1.74(6.88to8.04) | 7.76 ± 2.04(7.07to8.44) | 7.69 ± 1.87(6.97to8.40) | 7.82 ± 2.01(7.07to8.57) | 0.66 | 0.52 | 0.81 |
| ADIM(%) | |||||||
| Supine | 9.81 ± 18.20(3.74to15.80) | 5.66 ± 16.50(0.14to11.20) | 19.70 ± 18.4(12.70to26.70) | 13.60 ± 13.50(8.57to18.70) | <0.001* | 0.09 | 0.74 |
| Standing | 12.30 ± 19.70(5.78to18.90) | 5.41 ± 14.80(0.46to10.40) | 24.70 ± 27.1(14.40to35.10) | 12.90 ± 24.50(3.53to21.80) | 0.01* | 0.01* | 0.50 |
| TrA | |||||||
| Rest(mm) | |||||||
| Supine | 2.88 ± 0.91(2.58to3.19) | 3.24 ± 1.19(2.84to3.64) | 2.76 ± 0.94(2.40to3.11) | 2.96 ± 0.99(2.59to3.33) | 0.25 | 0.11 | 0.66 |
| Standing | 3.54 ± 1.07(3.18to3.89) | 3.71 ± 1.00(3.38to4.05) | 3.58 ± 1.37(3.06to4.10) | 3.76 ± 1.63(3.15to4.37) | 0.83 | 0.42 | 1.00 |
| ADIM(%) | |||||||
| Supine | 46.02 ± 34.33(34.61to57.03) | 47.38 ± 47.92(31.42to63.04) | 86.30 ± 42.42(70.21to102.05) | 69.99 ± 41.12(54.97to85.99) | <0.001* | 0.31 | 0.23 |
| Standing | 39.92 ± 35.59(27.99to51.82) | 36.11 ± 41.33(22.29to49.88) | 56.19 ± 52.44(36.22to76.09) | 58.63 ± 60.82(35.79to81.33) | 0.01* | 0.93 | 0.71 |
| Ratio for TrA | |||||||
| Preferential | |||||||
| Supine | 0.05 ± 0.04(0.04to0.07) | 0.06 ± 0.05(0.04to0.08) | 0.09 ± 0.03(0.08to0.10) | 0.08 ± 0.04(0.06to0.09) | <0.001* | 0.64 | 0.19 |
| Standing | 0.04 ± 0.04(0.03to0.06) | 0.05 ± 0.04(0.04to0.06) | 0.05 ± 0.03(0.04to0.06) | 0.06 ± 0.05(0.04to0.08) | 0.27 | 0.30 | 0.64 |
| Contraction | |||||||
| Supine | 1.46 ± 0.34(1.35to1.57) | 1.47 ± 0.48(1.31to1.63) | 1.86 ± 0.42(1.70to2.02) | 1.70 ± 0.41(1.55to1.86) | <0.001* | 0.31 | 0.23 |
| Standing | 1.40 ± 0.36(1.28to1.52) | 1.36 ± 0.41(1.22to1.50) | 1.56 ± 0.52(1.36to1.76) | 1.59 ± 0.61(1.36to1.81) | 0.02* | 0.93 | 0.71 |
Abbreviations: ADIM = % change during abdominal drawing-in manoeuvre; CI = confidence interval; OE = obliquus externus abdominis; OI = obliquus internus abdominis; RPA = regular physical activity; TrA = transversus abdominis.
p < 0.05.
3.4. ADIM
In the supine position, only 1 statistically significant difference was observed in the activities of the OI and TrA between the groups (Table 4). A detailed analysis demonstrated that the OI activity in the RPA group was higher by 8.9% (95%CI: 3.1–14.7). In case of the TrA, this difference was greater because the mean activity of this muscle in the RPA group was greater by 36% (95%CI: 19.1–47.5).
In the standing position, differences in the activities of the OI and TrA between the groups were also observed (Table 4). Similarly to the supine position, the OI activity in the RPA group was greater by 9.7% (95%CI: 2.3–17.6), and the activity of the TrA was greater by 19.4% (95%CI: 3.0–35.8). However, for OI, significant side-to-side differences were also shown; in each group, the activity of this muscle on the right side was greater by 9.11% (95%CI: 1.7–16.5).
3.5. Ratio
In the supine position, TrA preferential activation and TrA contraction ratio during ADIM were significantly greater in the RPA group. The TrA preferential activation ratio was greater by 0.03 (95%CI: 0.01–0.04), and the contraction ratio was greater by a mean of value of 0.35 (95%CI: 0.18–0.46). However, in the standing position, greater TrA capacity for contraction was only demonstrated in the RPA group where the contraction ratio was greater by 0.20 (95%CI: 0.03–0.36). In the standing position, no differences in the TrA preferential activation ratio were observed between the study groups (Table 4).
4. Discussion
This is the first report in which the effect of RPA on the muscles of the lateral wall of the abdomen at rest and during ADIM in the supine and standing positions in girls between 13 and 17 years of age was assessed. This is also the first work in which the reliability of the USI at rest and during ADIM in the supine and standing positions in physically active girls during adolescence was assessed. The analysis of the reliability demonstrated that the abdominal muscle USI in this population is highly reliable. Irrespective of the body position and muscular status (at rest or contracted), 3 repeated measurements yield a high ICC, which is consistent with other studies in children and adolescents33 and adult population.13, 34
The results obtained in this report suggest that in girls between 13 and 17 years of age, RPA does not affect rest muscle thickness of the OE, OI, and TrA in the standing or supine positions. In the supine position, the mean thickness of the OE was approximately 4.54 mm, OI 6.67 mm, and TrA 2.95 mm. In professional cricket players, Hides et al.8 demonstrated that in the players, the muscles of the lateral abdominal wall are thicker compared with the normal population.10 In this report, there was no significant effect of RPA on the thickness of the abdominal muscles in teenage girls. It is likely that these differences are due to types and levels of PAs. Cricketprofessionals must have strong trunk muscles, whereas in this study, girls performing only RPA were used. Thus, no analysis of the type of PA was performed. Moreover, at the professional level, training is certainly much more demanding compared with the amateur level. On the other hand, disproportions in the muscle thickness caused by the RPA may be revealed only at later stages of life (after many years of performing 1 type of sport). These data should be the basis for future studies in this area.
In both study groups in this report, the thickness of the OE and OI on the left side was greater. In case of OE this is probably a measurement error because the SDD for this muscle is greater than the mean side-to-side difference in the thickness of this muscle. However, the difference in the case of OI is real and, what is more interesting, greater in the group with no RPA. Studies of an adult population did not reveal any side-to-side differences in the thickness of the lateral abdominal wall.10, 13, 16 Rather, this asymmetry is linked to a pathology because it was observed in subjects with LBP.16 In these studies, the individuals in the control group were healthy and did not report any pain. It may be, however, that a more sedentary lifestyle has already caused certain abnormalities, compensatory in nature, in the muscles of the lateral abdominal wall, which, after being latent for many years, may cause pain. Such side-to-side differences in the thickness of the abdominal muscles during the stabilisation of the trunk may also cause muscular imbalance, which may cause micro-injuries in the facet joints or intervertebral discs.35, 36 The studies of Wedderkopp et al.37 demonstrated that a high level of PA seems to protect against LBP and mild back pain in early adolescence. On the other hand, individual side-to-side differences in the thickness of the lateral abdominal muscles among healthy adult subjects sometimes were large.10, 13 Interestingly, in the standing position, no significant differences in the resting thickness of the abdominal muscles were found in either group. At this point, however, it is difficult to explain why the asymmetry in the supine position disappears in the standing position.
Regarding the activity of the abdominal muscles during ADIM, some significant differences between the study groups were noted. The activity of the OI and TrA muscles was clearly higher in the supine and standing positions in the group performing RPA. In case of OI in the supine position and OI and TrA in the standing position, the differences can be due to measurement errors because of a higher SDD value compared to mean differences. However, the difference in the ADIM in the supine position is greater than SDD and suggests a real difference. This may imply that the girls performing RPA can better activate the TrA during ADIM in the supine position. Furthermore, in the supine position, the TrA preferential activation ratio in the girls performing RPA is significantly higher. Thus, one can conclude that the RPA positively affects the ability to activate TrA during ADIM in girls during adolescence. During ADIM, the body of the TrA shortens, resulting in a reduced cross section of the trunk.8 A limited ability to reduce transversal cross section of the trunk during AIDM is observed in professional athletes with LBP,38 and also in a normal, general population of subjects with LBP.39 On the other hand, Teyhen et al.7 believed that the ability of the TrA to perform independent work during ADIM depends on the respiratory pattern, deep sensation, and capacity of motor learning. It may be that RPA in adolescence affects the cross section of the trunk, deep sensation, and capacity of motor learning, and therefore, prevents spine pain. Indeed, it was demonstrated that a high level of PA seems to protect against LBP and mild back pain in early adolescence.37 Thus, the results obtained in no way indicate a negative effect of RPA on TrA as was observed in the studies performed on elite Australian football players.26 However, one cannot eliminate the possibility that certain sports can predispose an individual to a disorder of the muscles of the lateral abdominal walls. Perhaps this is only a problem of athletes at the highest levels. Therefore, a limitation of this work is the inclusion in the RPA group of the individuals performing various sports whose nature (despite regularity) can only be recreational. In future studies, characteristics of different muscles of the lateral wall in various sport discipline and at different sports levels, also in adolescents, should be studied.
These studies also explain the reason for the discrepancy in TrA contraction ratio between Mannion et al.10 and Springer et al.16 The data presented in Table 4 show that in the group with no RPA, this ratio is only 1.50 – similar to the results of the studies in a normal adult population,10 while the TrA contraction ratio in the RPA group is less than 1.8 and similar to the results obtained by Springer et al.16 Thus, in the report by Springer et al.,16 most likely, the subjects are distinctly more physically active than those in other studies.10, 17 This calls for greater caution in using a TrA contraction ratio in subjects with LBP and/or other musculoskeletal disorders (e.g., scoliosis) because it may, to a great extent, depend on PA.
5. Conclusion
RPA does not have any effect on the resting thickness of the OE, OI, and TrA muscles in the supine and standing positions in girls between 13 and 17 years of age. Girls performing RPA have a greater ability to perform an independent activation and greater contractions of TrA while supine down, which affects the stabilisation of the pelvis and lumbar spine. The level of PA in the study subject can also affect the results of the TrA contraction ratio in the supine and standing positions. Thus, this fact should be taken into account in future studies comparing various symptomatic groups.
Authors' contributions
PL conceived of the study, carried out the ultrasound measurements, performed statistical analysis, and drafted the manuscript; ES carried out the statistical analysis and helped to draft the manuscript; TW carried out the material selection and participated in its design and coordination; AM carried out the material selection and participated in its design. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
None of the authors declare competing financial interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.Bergmark A. Stability of the lumbar spine. A study in mechanical engineering. Acta Orthop Scand Suppl. 1989;230:20–24. doi: 10.3109/17453678909154177. [DOI] [PubMed] [Google Scholar]
- 2.Hodges P.W. Is there a role for transversus abdominis in lumbo-pelvic stability? Man Ther. 1999;4:74–86. doi: 10.1054/math.1999.0169. [DOI] [PubMed] [Google Scholar]
- 3.Hodges P.W., Moseley G.L. Pain and motor control of the lumbopelvic region: effect and possible mechanisms. J Electromyogr Kinesiol. 2003;13:361–370. doi: 10.1016/s1050-6411(03)00042-7. [DOI] [PubMed] [Google Scholar]
- 4.Ferreira P.H., Ferreira M.L., Hodges P.W. Changes in recruitment of the abdominal muscles in people with low back pain: ultrasound measurement of muscle activity. Spine (Phila Pa 1976) 2004;29:2560–2566. doi: 10.1097/01.brs.0000144410.89182.f9. [DOI] [PubMed] [Google Scholar]
- 5.Hides J.A., Belavý D.L., Cassar L., Williams M., Wilson S.J., Richardson C.A. Altered response of the anterolateral abdominal muscles to simulated weight-bearing in subjects with low back pain. Eur Spine J. 2009;18:410–418. doi: 10.1007/s00586-008-0827-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Costa L.O., Maher C.G., Latimer J., Smeets R.J. Reproducibility of rehabilitative ultrasound imaging for the measurement of abdominal muscle activity: a systematic review. Phys Ther. 2009;89:756–769. doi: 10.2522/ptj.20080331. [DOI] [PubMed] [Google Scholar]
- 7.Teyhen D.S., Gill N.W., Whittaker J.L., Henry S.H., Hides J.A., Hodges P. Rehabilitative ultrasound imaging of the abdominal muscles. J Orthop Sports Phys Ther. 2007;37:450–466. doi: 10.2519/jospt.2007.2558. [DOI] [PubMed] [Google Scholar]
- 8.Hides J., Wilson S., Stanton W., McMahon S., Keto H., McMahon K. An MRI investigation into the function of the transversus abdominis muscle during ‘drawing-in’ of the abdominal wall. Spine (Phila Pa 1976) 2006;31:E175–8. doi: 10.1097/01.brs.0000202740.86338.df. [DOI] [PubMed] [Google Scholar]
- 9.Hodges P.W., Pengel L.H., Herbert R.D., Gandevia S.C. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve. 2003;27:682–692. doi: 10.1002/mus.10375. [DOI] [PubMed] [Google Scholar]
- 10.Mannion A.F., Pulkovski N., Toma V., Sprott H. Abdominal muscle size and symmetry at rest and during abdominal hollowing exercises in healthy control subjects. J Anat. 2008;213:173–182. doi: 10.1111/j.1469-7580.2008.00946.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manshadi F.D., Parnianpour M., Sarrafzadeh J., Azghani M.R., Kazemnejad A. Abdominal hollowing and lateral abdominal wall muscles' activity in both healthy men & women: an ultrasonic assessment in supine and standing positions. J Bodyw Mov Ther. 2011;15:108–113. doi: 10.1016/j.jbmt.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Pulkovski N., Mannion A.F., Caporaso F., Toma V., Gubler D., Helbling D. Ultrasound assessment of transversus abdominis muscle contraction ratio during abdominal hollowing: a useful tool to distinguish between patients with chronic low back pain and healthy controls? Eur Spine J. 2011;21:750–759. doi: 10.1007/s00586-011-1707-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rankin G., Stokes M., Newham D.J. Abdominal muscle size and symmetry in normal subjects. Muscle Nerve. 2006;34:320–326. doi: 10.1002/mus.20589. [DOI] [PubMed] [Google Scholar]
- 14.Rho M., Spitznagle T., Van Dillen L., Maheswari V., Oza S., Prather H. Gender differences on ultrasound imaging of lateral abdominal muscle thickness in asymptomatic adults: pilot study. PM R. 2013;5:374–380. doi: 10.1016/j.pmrj.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 15.Teyhen D.S., Miltenberger C.E., Deiters H.M., Del Toro Y.M., Pulliam J.N., Childs J.D. The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J Orthop Sports Phys Ther. 2005;35:346–355. doi: 10.2519/jospt.2005.35.6.346. [DOI] [PubMed] [Google Scholar]
- 16.Springer B.A., Mielcarek B.J., Nesfield T.K., Teyhen D.S. Relationships among lateral abdominal muscles, gender, body mass index, and hand dominance. J Orthop Sports Phys Ther. 2006;36:289–297. doi: 10.2519/jospt.2006.2217. [DOI] [PubMed] [Google Scholar]
- 17.Critchley D.J., Coutts F.J. Abdominal muscle function in chronic low back pain patients: measurement with real-time ultrasound scanning. Physiotherapy. 2002;88:322–332. [Google Scholar]
- 18.Linek P., Saulicz E., Kuszewski M., Wolny T. Ultrasound assessment of the abdominal muscles at rest and during the ASLR test among adolescents with scoliosis. Clin Spine Surg. 2016 doi: 10.1097/BSD.0000000000000055. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Yang H.S., Yoo J.W., Lee B.A., Choi C.K., You J.H. Inter-tester and intra-tester reliability of ultrasound imaging measurements of abdominal muscles in adolescents with and without idiopathic scoliosis: a case-controlled study. Biomed Mater Eng. 2014;24:453–458. doi: 10.3233/BME-130830. [DOI] [PubMed] [Google Scholar]
- 20.Linek P., Saulicz E., Wolny T., Myśliwiec A., Kokosz M. Lateral abdominal muscle size at rest and during abdominal drawing-in manoeuvre in healthy adolescents. Man Ther. 2015;20:117–123. doi: 10.1016/j.math.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 21.Lemos A.T., Santos F.R., Moreira R.B., Machado D.T., Braga F.C., Gaya A.C. Low back pain and associated factors in children and adolescents in a private school in Southern Brazil. Cad Saude Publica. 2013;29:2177–2185. doi: 10.1590/0102-311x00030113. [DOI] [PubMed] [Google Scholar]
- 22.Wirth B., Knecht C., Humphreys K. Spine day 2012: spinal pain in Swiss school children – epidemiology and risk factors. BMC Pediatr. 2013;5:159. doi: 10.1186/1471-2431-13-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Konieczny M.R., Senyurt H., Krauspe R. Epidemiology of adolescent idiopathic scoliosis. J Child Orthop. 2013;7:3–9. doi: 10.1007/s11832-012-0457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zazulak B.T., Hewett T.E., Reeves N.P., Goldberg B., Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35:1123–1130. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 25.Zazulak B.T., Hewett T.E., Reeves N.P., Goldberg B., Cholewicki J. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007;35:368–373. doi: 10.1177/0363546506297909. [DOI] [PubMed] [Google Scholar]
- 26.Hides J., Stanton W. Muscle imbalance among elite Australian rules football players: a longitudinal study of changes in trunk muscle size. J Athl Train. 2012;47:314–319. doi: 10.4085/1062-6050-47.3.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bunnell W.P. An objective criterion for scoliosis screening. J Bone Joint Surg Am. 1984;66:1381–1387. [PubMed] [Google Scholar]
- 28.Korovessis P., Koureas G., Zacharatos S., Papazisis Z. Backpacks, back pain, sagittal spinal curves and trunk alignment in adolescents: a logistic and multinomial logistic analysis. Spine (Phila Pa 1976) 2005;30:247–255. doi: 10.1097/01.brs.0000150505.59690.1b. [DOI] [PubMed] [Google Scholar]
- 29.Bonagamba G.H., Coelho D.M., Oliviera A.S. Inter and intra-rater reliability of the scoliometer. Rev Bras Fisioter. 2010;14:432–438. [PubMed] [Google Scholar]
- 30.Hides J., Richardson C., Hodges P. Local segmental control. In: Richardson C., Hodges P., Hides J., editors. Therapeutic exercise for lumbopelvic stabilization. Churchill Livingstone; Edinburg: 2004. pp. 185–220. [Google Scholar]
- 31.Gnat R., Saulicz E., Miądowicz B. Reliability of real-time ultrasound measurement of transversus abdominal thickness in healthy trained subjects. Eur Spine J. 2012;21:1508–1515. doi: 10.1007/s00586-012-2184-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shrout P.E., Fleiss J.L. Intraclass correlation: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 33.Linek P., Saulicz E., Wolny T., Myśliwiec A. Reliability of B-mode sonography of the abdominal muscles in healthy adolescents in different body positions. J Ultrasound Med. 2014;33:1049–1056. doi: 10.7863/ultra.33.6.1049. [DOI] [PubMed] [Google Scholar]
- 34.Mew R. Comparison of changes in abdominal muscle thickness between standing and crook lying during active abdominal hollowing using ultrasound imaging. Man Ther. 2009;14:690–695. doi: 10.1016/j.math.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 35.Cholewicki J., McGill S.M. Mechanical stability of the in vivo lumbar spine: implications for injury and low back pain. Clin Biomech (Bristol, Avon) 1996;11:1–15. doi: 10.1016/0268-0033(95)00035-6. [DOI] [PubMed] [Google Scholar]
- 36.Vera-Garcia F.J., Brown S.H., Gray J.R., McGill S.M. Effects of different levels of torso coactivation on trunk muscular and kinematic responses to posteriorly applied sudden loads. Clin Biomech (Bristol, Avon) 2006;21:443–445. doi: 10.1016/j.clinbiomech.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 37.Wedderkopp N., Kjaer P., Hestbaek L., Korsholm L., Leboeuf-Yde C. High-level physical activity in childhood seems to protect against low back pain in early adolescence. Spine J. 2009;9:134–141. doi: 10.1016/j.spinee.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Hides J.A., Bouqhen C.L., Stanton W.R., Strudwick M.W., Wilson S.J. A magnetic resonance imaging investigation of the transversus abdominis muscle during drawing-in of the abdominal wall in elite Australian Football League players with and without low back pain. J Orthop Sports Phys Ther. 2010;40:4–10. doi: 10.2519/jospt.2010.3177. [DOI] [PubMed] [Google Scholar]
- 39.Richardson C.A., Hides J.A., Wilson S., Stanton W., Snijders C.J. Lumbo-pelvic joint protection against antigravity forces: motor control and segmental stiffness assessed with magnetic resonance imaging. J Gravit Physiol. 2004;11:119–122. [PubMed] [Google Scholar]


