Abstract
Objective
To describe the demographic characteristics of patients who present to the emergency department (ED) for low-acuity issues and to explore their self-reported contact with other sources of primary health care before presenting to the ED.
Design
Survey distributed in the ED waiting room.
Setting
A high-volume ED in Vancouver, BC.
Participants
A total of 232 respondents aged 18 years or older in the ED waiting room.
Main outcome measures
Actions taken to seek health care for the current issue before presenting to the ED and predictors of first seeking nonurgent care.
Results
Of the 398 people approached, 232 (58.3%) people completed the survey. Exactly half (95% CI 43.6% to 56.4%) sought alternative care before presenting to the ED. Predictors for having sought alternative care included illness presentation and longer symptom duration, while injury presentation and work-related presentation were associated with not seeking alternative care. Most participants (162 patients, 87.6%) believed that the ED was the most appropriate place for them to receive care for their problem, while only 87 (45.3%) believed that an adjacent primary care clinic would be an acceptable alternative.
Conclusion
Many patients do attempt to seek alternative care before presenting to the ED with low acuity issues. Most patients believe that the ED is the best place for them to receive care and are uncertain about using a primary care alternative. Further research is needed to explore barriers and motivators patients face in their decisions to seek care, as well as potential patient education methods to improve appropriate ED use.
Résumé
Objectif
Établir les caractéristiques des patients qui se présentent à l’urgence pour des problèmes de santé de peu de gravité et vérifier s’ils disent avoir d’abord visité un autre établissement de soins primaires avant de se présenter à l’urgence.
Type d’étude
Un sondage distribué aux patients dans la salle d’attente.
Contexte
Une urgence très achalandée de Vancouver, en Colombie-Britannique.
Participants
Un total de 232 répondants d’au moins 18 ans, dans la salle d’attente.
Principaux paramètres à l’étude
Les efforts des participants pour pour se faire traiter ailleurs avant de se présenter à l’urgence et les prédicteurs de cette façon de faire.
Résultats
Sur les 398 personnes auxquelles on a offert de participer, 232 (58,3 %) ont répondu au questionnaire. La moitié d’entre elles (IC à 95 %, 43,6 % à 56,4 %) avaient essayé de se faire soigner ailleurs avant d’aller à l’urgence. Les prédicteurs d’un tel choix incluaient le fait qu’il s’agissait d’une maladie et que les symptômes duraient depuis un certain temps, alors que dans le cas d’une blessure ou d’un problème lié au travail, on était moins porté à chercher un autre endroit pour se faire traiter. La plupart des participants (162 patients, 87,6 %) estimaient que la salle d’urgence était le meilleur endroit pour être traités, alors que seulement 87 d’entre eux (45,3 %) croyaient qu’une clinique de soins primaires dans le voisinage serait une alternative acceptable.
Conclusion
Plusieurs patients qui présentent un problème de peu de gravité essaient de se faire traiter ailleurs avant d’aller à l’urgence. La plupart des patients croient que l’urgence est le meilleur endroit pour être traités et ne sont pas convaincus qu’un établissement de soins primaires serait adéquat. D’autres études seront nécessaires pour identifier les obstacles ou les incitatifs qui influent sur les décisions des patients lorsqu’ils cherchent à se faire soigner, et pour trouver d’éventuelles façons de renseigner les patients sur la façon adéquate d’utiliser l’urgence.
Emergency departments (EDs) in Canada are designed to give near-immediate access to care for critically ill patients in their times of need. With rising health care costs in Canada and internationally, there is incentive to divert these cases from the ED and manage them in a more cost-effective primary care visit.1 Patients presenting to the ED for nonurgent, low-acuity medical conditions also contribute to ED overcrowding and worsen long ED wait times,2 although there is some evidence suggesting low-complexity patients have a negligible effect on wait times for patients with higher acuity.3
Emergency department visits for low-acuity or non-urgent issues make up 25% to 30% of ED visits across Canada.4,5 Previous research has suggested that patients present to the ED for low-acuity issues for many reasons, including perceiving their issues as very urgent, trust in the hospital, proximity of the hospital to their home, expediency of being seen by a doctor, and referral from another physician to the ED.5–7 In North America, the frequency of ED visits for low-acuity issues has been found to be higher in populations that are younger, are male, are homeless, have lower socioeconomic status, and have no regular primary health care provider.8–10
The purpose of this study is to describe the patterns of use of other primary health care services (family doctors, walk-in clinics, telephone support) before accessing the ED of patients who present for low-acuity medical issues. For the purposes of this article, we will refer to other primary care services outside of the ED as alternative care. Understanding the patterns of access or attempted access to alternative care before accessing the ED might help inform policy decisions on interventions to reduce ED wait times and costs, and it might provide more accessible primary care options.
METHODS
Study design
A validated, paper-based survey was presented to patients in the ED of St Paul’s Hospital in Vancouver, BC, over a 5-month period from July to December 2015.11 St Paul’s Hospital is a busy inner-city ED that manages more than 83 000 patient visits per year. Pope et al have previously described this hospital as follows:
Because of its location, a large number of these patients are homeless, are unemployed or are receiving social assistance, or have complex or chronic medical problems, including HIV-related illness and substance abuse.12
The study protocol, survey, and all research-related materials were reviewed by the University of British Columbia Providence Health Care Clinical Research Ethics Board.
Study participants
Study personnel (medical student volunteers) distributed surveys in the ED waiting room to patients aged 18 years or older between 8:00 am and 10:00 pm. It was assumed that these patients had nonacute or low-acuity problems by virtue of being asked to stay in the waiting room by the triage nurses.4 All patients were invited to participate in the survey unless the volunteers believed the patients would be unable to complete the survey because they appeared to be actively delirious, under the influence of illicit substances, or exhibiting violent behaviour. Study personnel were given the discretion to determine whether to approach potential participants. The survey was only presented in English, so patients who were unable to communicate in written English were excluded.
Survey instrument
The survey tool was a modified version of one used by Han et al,11 who created and distributed a survey that described demographic characteristics and patient efforts to access alternative care before presenting to the ED in Edmonton, Alta. Slight modifications were applied to reflect local health care priorities, namely ED presentations related to frailty, mental health, and substance use. The 37-question paper-based survey was presented to patients in the waiting room of the ED by volunteers. Patients were given a short verbal introduction to the survey and a detailed introductory letter that explained the consent implied by completing the survey. The survey took 10 to 20 minutes to complete and a volunteer was available at all times to answer questions that arose. To ensure anonymity, there was no attempt to link survey respondents with any personal data or health care records.
Sample size
Target sample size for this study was calculated with the goal of obtaining a margin of error for binary outcomes of 6%, which resulted in a target sample size of 300 completed surveys.
Statistical analysis
Dichotomous variables were summarized with percentages; continuous variables were summarized with means and SDs. Bivariate analyses using
 2 tests were used to compare 2 groups—those who did and those who did not seek alternative care before their ED presentation. This allowed assessment of factors that might be associated with an increased or decreased likelihood of seeking alternative care before presenting to the ED. The data were analyzed with SPSS software, version 22.
2 tests were used to compare 2 groups—those who did and those who did not seek alternative care before their ED presentation. This allowed assessment of factors that might be associated with an increased or decreased likelihood of seeking alternative care before presenting to the ED. The data were analyzed with SPSS software, version 22.
RESULTS
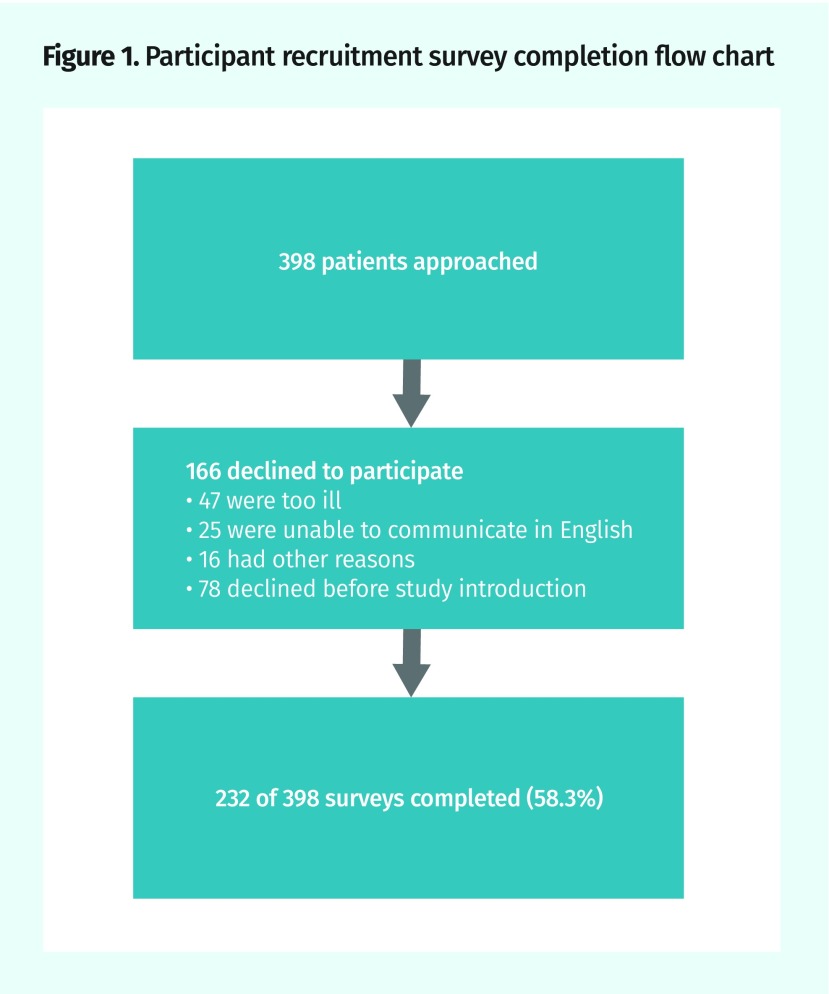
Overall, the survey was presented to 398 patients. Of these, 166 declined to participate (Figure 1). A total of 232 patients completed the survey (response rate of 58.3%). Not all survey questions were answered by all patients. Response rates reported for each question reflect those for which any response was recorded and the denominators were adjusted accordingly.
Figure 1.
Participant recruitment survey completion flow chart
Participant characteristics and predictors of seeking alternative care
Characteristics of the study participants are summarized in Table 1, comparing those who had sought alternative care before ED presentation (n = 116, 50.0%; 95% CI 43.6% to 56.4%) with those who had not (n = 116, 50.0%). Factors associated with seeking alternative care before the ED visit were illness presentation (
 2
P = .024) and symptom duration (
2
P = .024) and symptom duration (
 2
P = .007, with a longer duration of symptoms associated with increased likelihood of having sought alternative care). Conversely, factors that were significantly associated with not seeking alternative care before the ED visit included injury presentation (
2
P = .007, with a longer duration of symptoms associated with increased likelihood of having sought alternative care). Conversely, factors that were significantly associated with not seeking alternative care before the ED visit included injury presentation (
 2
P = .044) and work-related presentation (injury or illness;
2
P = .044) and work-related presentation (injury or illness;
 2
P = .028). There were no other statistically significant differences observed between the 2 groups.
2
P = .028). There were no other statistically significant differences observed between the 2 groups.
Table 1.
Characteristics of patients presenting to the ED: Not all survey questions were answered by all patients. Response rates reported for each question reflect those for which any response was recorded and the denominators were adjusted accordingly. P values in bold are statistically significant.
| VARIABLE | TOTAL PARTICIPANTS (N = 232) | ATTEMPTED ALTERNATIVE CARE (N = 116) | DID NOT ATTEMPT ALTERNATIVE CARE (N = 116) |  2P VALUE 2P VALUE |
|---|---|---|---|---|
| Mean (SD) age, y | 42.65 (17.12) | 43.14 (17.23) | 42.03 (17.06) | NA |
| Female sex, n (%) | 97 (51.1) | 55 (56.7) | 42 (43.3) | .48 |
| Marital status, n (%) | .68 | |||
| • Married or common law | 83 (41.3) | 46 (55.4) | 37 (44.6z) | |
| • Currently single | 111 (55.2) | 59 (53.2) | 52 (46.8) | |
| • Prefer not to answer | 7 (3.5) | 5 (71.4) | 2 (28.6) | |
| Living arrangements, n (%) | .91 | |||
| • Living alone | 57 (28.2) | 29 (50.9) | 28 (49.1) | |
| • Homeless | 6 (3.0) | 3 (50.0) | 3 (50.0) | |
| • Other | 5 (2.5) | 3 (60.0) | 2 (40.0) | |
| • Prefer not to answer | 134 (66.3) | 75 (56.0) | 59 (44.0) | |
| Residence, n (%) | .67 | |||
| • Independent living (eg, house, apartment) | 176 (87.1) | 96 (54.5) | 80 (45.5) | |
| • Assisted living or long-term care | 2 (1.0) | 1 (50.0) | 1 (50.0) | |
| • Homeless | 10 (5.0) | 7 (70.0) | 3 (30.0) | |
| • Other | 11 (5.4) | 4 (36.4) | 7 (63.6) | |
| • Prefer not to answer | 3 (1.5) | 2 (66.7) | 1 (33.3) | |
| Education level, n (%) | .091 | |||
| • High school or less | 58 (29.0) | 25 (43.1) | 33 (56.9) | |
| • Postsecondary | 136 (68.0) | 81 (59.6) | 55 (40.4) | |
| • Prefer not to answer | 6 (3.0) | 4 (66.7) | 2 (33.3) | |
| Primary activity in past 12 mo, n (%) | .96 | |||
| • Unemployed or disabled | 35 (17.4) | 18 (51.4) | 17 (48.6) | |
| • Other (eg, work, school, retired) | 149 (74.1) | 82 (55.0) | 67 (45.0) | |
| • Multiple activities | 5 (2.5) | 3 (60.0) | 2 (40.0) | |
| • Prefer not to answer | 12 (6.0) | 7 (58.3) | 5 (41.7) | |
| Cigarette smoking, n (%) | .95 | |||
| • Never | 107 (53.2) | 58 (54.2) | 49 (45.8) | |
| • Ex-smoker | 41 (20.4) | 22 (53.7) | 19 (46.3) | |
| • Current smoker | 53 (26.4) | 30 (56.6) | 23 (43.4) | |
| Walking ability, n (%) | .28 | |||
| • Unable to walk outside | 2 (1.0) | 1 (50.0) | 1 (50.0) | |
| • < 2 blocks | 34 (17.3) | 23 (67.6) | 11 (32.4) | |
| • ≥ 2 blocks | 161 (81.7) | 85 (52.8) | 76 (47.2) | |
| Has a family physician, n (%) | 157 (72.4) | 68 (43.3) | 89 (56.7) | .078 |
| Injury presentation, n (%) | 55 (24.6) | 21 (38.2) | 34 (61.8) | .044 |
| Illness presentation, n (%) | 122 (54.0) | 70 (57.4) | 52 (42.6) | .024 |
| Work-related illness or injury presentation, n (%) | 11 (4.9) | 2 (18.2) | 9 (81.8) | .028 |
| Mental health presentation, n (%) | 29 (12.8) | 17 (58.6) | 12 (41.4) | .32 |
| Substance use presentation, n (%) | 13 (5.8) | 8 (61.5) | 5 (38.5) | .41 |
| Symptom duration, n (%) | .007 | |||
| • < 48 h | 60 (34.7) | 21 (35.0) | 39 (65.0) | |
| • 2–7 d | 54 (31.2) | 26 (48.1) | 28 (51.9) | |
| • 8–30 d | 28 (16.2) | 20 (71.4) | 8 (28.6) | |
| • > 30 d | 31 (17.9) | 19 (61.3) | 12 (38.7) |
ED—emergency department, NA—not applicable.
Type of alternative care accessed
Among the 116 patients who sought alternative care before their ED presentation (Table 2), 78 (67.2%) reported they had been assessed by a physician and 26 (22.4%) sought help from another type of health care professional. An additional 54 (46.6%) obtained advice over the telephone. Some patients reported having sought alternative care from more than 1 source. Of those patients who reported having been assessed by a physician before presenting to the ED, 49 (62.8%) reported having been advised to present to the ED.
Table 2.
Alternative care providers accessed before the emergency department visit: N = 116; not all survey questions were answered by all patients. Response rates reported for each question reflect those for which any response was recorded and the denominators were adjusted accordingly.
| TYPE OF PRACTITIONER | PATIENTS WHO ATTEMPTED ACCESS, N (%) |
|---|---|
| Physician visit | 78 (67.2) |
| • Family physician | 30 (25.9) |
| • Walk-in clinic | 33 (28.4) |
| • Non–family physician specialist | 7 (6.4) |
| • Other | 1 (0.9) |
| Other health care professional visit | 26 (22.4) |
| • Naturopath | 2 (1.7) |
| • Massage therapist | 1 (0.9) |
| • Other | 18 (15.5) |
| • Multiple | 2 (1.7) |
| • No response | 3 (2.6) |
| Called a physician’s office | 54 (46.6) |
| Called provincial health information line | 13 (11.2) |
Satisfaction and acceptability of alternatives
Among all surveyed patients, 162 (87.6%) maintained that the ED was the best place for them to obtain care at that time. When asked whether a primary care sidetrack to the ED might be an acceptable alternative, 87 (45.3%) responded yes, while 50 (26.0%) responded no and 55 (28.6%) were unsure.
DISCUSSION
This study described the characteristics of patients presenting to an urban ED with low-acuity issues and assessed their attempts to seek alternative health care before arriving there. The data revealed that half of low-acuity ED patients attempted to access care elsewhere before presenting to the ED, which is consistent with the findings of Han et al.11
While injury presentation appears to be a consistent predictor of not seeking alternative care, other factors that were found to have statistically significant effects by Han et al, including living arrangements, smoking status, and whether or not the patient had a family doctor, were not found to have significant effects in this study.11 Locally, there are few alternatives to the ED after typical weekday business hours and few, if any, primary care clinics are able to offer imaging, diagnostic tests, and treatments such as casts or intravenous therapy. The choice of our surveyed population to go to the ED might be a reasonable one based on their past experiences or their own assessment of their current needs. As research in this area is limited, additional studies in other settings and centres would be useful to clarify predictors and trends.
In this study population, a substantial proportion of patients (27.6%) stated that they did not have a family doctor. A recent community survey13 reported that 23% of Vancouver residents do not have a family doctor. This is above the 2014 national average of approximately 14.9%.14 An Ontario study demonstrated that patients who have good access to a family physician are less likely to seek care in the ED15; however, in our study no significant relationship was found between having a family physician and seeking primary care before emergency care. Our results are consistent with a 2014 New Brunswick study that found no significant difference in the proportions of patients presenting to the ED with or without a primary care provider.16
We found that 62.8% of the 78 patients who first sought alternative care were advised by their physicians to visit the ED for their nonurgent issue. This frequency is higher than those previously reported in Canada. A study of nonurgent presentations to the pediatric ED found that 15% of respondents had been referred to the ED by a primary care provider.17 Our findings were more consistent with those of Lobachova et al,18 who found in their American study that 76% of patients who reached a health care provider by telephone were referred to the ED and half of those referrals seem to have been for nonurgent issues, as the patient was not subsequently admitted to the hospital. Our results suggest that primary care providers might be a direct source of referrals to the ED, possibly owing to limitations of diagnosis and treatment in community-based practices. Lobachova et al18 surveyed family physicians who said that 24-hour community radiology and laboratory services and extended primary care urgent care hours would reduce primary care provider referrals to the ED. Additional research into the factors that determine primary care physicians’ referrals to the ED would help illuminate this finding. Further, the availability of these same services might contribute to our finding that patients with an injury or work-related presentation—both presumably perceived to require more urgent, accessible care and investigations—were less likely to have sought alternative care before presenting to the ED.
Most survey respondents (87.6%) believed the ED was the best place for them to receive care for their problem, which is consistent with the study by Han et al.11 These findings have important implications for health planners and policy makers striving to reduce ED overcrowding. These patient perceptions suggest that simply offering a primary care alternative to the ED will not solve the problem; rather, an evaluation of interventions that emphasize both patient and health care provider education regarding appropriate ED use and referral, as well as potential alternatives, would likely be a more advantageous focus in the future. Further research exploring the relationship between primary care attachment and frequency of ED use might also provide evidence for future interventions.
Limitations
Patient recruitment was more challenging than anticipated. Owing to specific recommendations from the approving ethics board, survey distribution had to be done by unpaid volunteers not directly involved in the research. This affected how evenly the survey was distributed during our investigation period. There were often few patients in the waiting room when data collection was attempted, which might have been related to a change in ED work flow that was implemented part way through our study period. Study personnel chose whether to approach patients who appeared to be delirious, under the influence of drugs or alcohol, or exhibiting violent behaviour, which might have also limited survey participation. As a result, the sample was smaller than initially projected and smaller than those of similar studies.11,19
Patients’ hospital records were not accessed or included in this study, and so the assumption that patients in the waiting room were presenting with low-acuity problems could not be confirmed; it is possible that some patients might have been seriously ill. Additionally, this study looked only at the population at one urban ED, specifically one that is known for serving a marginalized population. This might limit the generalizability of these results to other settings, such as rural areas, or even to other urban centres.
Conclusion
This study adds to the limited literature examining reasons why people present to the ED with low-acuity issues. Despite a general assumption among health care providers that many low-acuity ED presentations could be adequately treated in a primary care setting,4 most ED patients believed that the ED was the best place for them. This belief was reinforced by health care providers, who referred most patients who first sought alternative care to the ED for nonurgent issues.
Editor’s key points
▸ Despite a general assumption among health care providers that many low-acuity emergency department (ED) presentations could be adequately treated in a primary care setting, most patients surveyed in this study (87.6%) believed that the ED was the best place for them.
▸ Half of low-acuity ED patients attempted to access care elsewhere before presenting to the ED. This was reinforced by health care providers, who referred most (62.8%) patients who first sought alternative care for nonurgent issues to the ED.
▸ A substantial proportion of patients (27.6%) stated that they did not have a family doctor. However, no significant relationship was found between having a family physician and seeking primary care before emergency care.
Points de repère du rédacteur
▸Bien qu’un bon nombre de soignants soient d’avis que plusieurs problèmes de santé de peu de gravité pourraient être traités adéquatement dans une clinique de soins primaires, la plupart des patients ayant participé à cette enquête (87,6 %) estimaient que le service des urgences était la meilleure solution pour eux.
▸ La moitié des patients s’étant présentés à l’urgence pour des problèmes peu sévères avaient d’abord tenté d’aller ailleurs. Cette façon de faire était d’ailleurs renforcée par des soignants qui référaient 62,8 % de leurs patients à l’urgence pour des problèmes de santé non urgents.
▸ Une proportion importante des patients (27,6 %) a déclaré ne pas avoir de médecin de famille. Toutefois, aucune relation n’a été observée entre le fait de ne pas avoir de médecin de famille et celui de vouloir chercher un milieu de soins primaires avant d’aller à l’urgence.
Footnotes
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Gonçalves-Bradley D, Khangura JK, Flodgren G, Perera R, Rowe BH, Shepperd S. Primary care professionals providing non-urgent care in hospital emergency departments. Cochrane Database Syst Rev. 2018;(2):CD002097. doi: 10.1002/14651858.CD002097.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 3.Schull MJ, Kiss A, Szalai JP. The effect of low-complexity patients on emergency department waiting times. Ann Emerg Med. 2007;49(3):257–64. 264.e1. doi: 10.1016/j.annemergmed.2006.06.027. Epub 2006 Aug 22. [DOI] [PubMed] [Google Scholar]
- 4.Vertesi L. Does the Canadian Emergency Department Triage and Acuity Scale identify non-urgent patients who can be triaged away from the emergency department? CJEM. 2004;6(5):337–42. doi: 10.1017/s1481803500009611. [DOI] [PubMed] [Google Scholar]
- 5.Afilalo J, Marinovich A, Afilalo M, Colacone A, Léger R, Unger B, et al. Nonurgent emergency department patient characteristics and barriers to primary care. Acad Emerg Med. 2004;11(12):1302–10. doi: 10.1197/j.aem.2004.08.032. Erratum in: Acad Emerg Med 2005;12(1):12. [DOI] [PubMed] [Google Scholar]
- 6.Smith V, Mustafa M, Grafstein E, Doan Q. Factors influencing the decision to attend a pediatric emergency department for nonemergent complaints. Pediatr Emerg Care. 2015;31(9):640–4. doi: 10.1097/PEC.0000000000000392. [DOI] [PubMed] [Google Scholar]
- 7.Gill JM, Riley AW. Nonurgent use of hospital emergency departments: urgency from the patient’s perspective. J Fam Pract. 1996;42(5):491–6. [PubMed] [Google Scholar]
- 8.Vanstone NA, Belanger P, Moore K, Caudle JM. Socioeconomic composition of low-acuity emergency department users in Ontario. Can Fam Physician. 2014;60:355–62. [PMC free article] [PubMed] [Google Scholar]
- 9.Geurts J, Palatnick W, Strome T, Sutherland KA, Weldon E. Frequent users of an inner-city emergency department. CJEM. 2012;14(5):306–13. doi: 10.2310/8000.2012.120670. Erratum in: CJEM 2016;18(1):80. [DOI] [PubMed] [Google Scholar]
- 10.Petersen LA, Burstin HR, O’Neil AC, Orav EJ, Brennan TA. Nonurgent emergency department visits: the effect of having a regular doctor. Med Care. 1998;36(8):1249–55. doi: 10.1097/00005650-199808000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Han A, Ospina M, Blitz SB, Strome T, Rowe BH. Patients presenting to the emergency department: the use of other health care services and reasons for presentation. CJEM. 2007;9(6):428–34. doi: 10.1017/s1481803500015451. [DOI] [PubMed] [Google Scholar]
- 12.Pope D, Fernandes CM, Bouthillette F, Etherington J. Frequent users of the emergency department: a program to improve care and reduce visits. CMAJ. 2000;162(7):1017–20. [PMC free article] [PubMed] [Google Scholar]
- 13.My Health My Community . Vancouver community health profile. Vancouver, BC: Vancouver Coastal Health, Fraser Health, University of British Columbia; 2016. Available from: https://www.myhealthmycommunity.org/Portals/0/Documents/Community%20Profiles/Vancouver_final.pdf. Accessed 2018 Jul 6. [Google Scholar]
- 14.Statistics Canada . Access to a regular medical doctor, 2014. Ottawa, ON: Statistics Canada; 2015. Available from: www.statcan.gc.ca/pub/82-625-x/2015001/article/14177-eng.htm. Accessed 2016 Nov 19. [Google Scholar]
- 15.Mian O, Pong R. Does better access to FPs decrease the likelihood of emergency department use? Results from the Primary Care Access Survey. Can Fam Physician. 2012;58:e658–66. Available from: www.cfp.ca/content/cfp/58/11/e658.full.pdf. Accessed 2018 Jul 6. [PMC free article] [PubMed] [Google Scholar]
- 16.Palmer E, Leblanc-Duchin D, Murray J, Atkinson P. Emergency department use. Is frequent use associated with a lack of primary care provider? Can Fam Physician. 2014;60:e223–9. Available from: www.cfp.ca/content/cfp/60/4/e223.full.pdf. Accessed 2018 Jul 6. [PMC free article] [PubMed] [Google Scholar]
- 17.Farion KJ, Wright M, Zemek R, Neto G, Karwowska A, Tse S, et al. Understanding low-acuity visits to the pediatric emergency department. PLoS One. 2015;10(6):e0128927. doi: 10.1371/journal.pone.0128927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lobachova L, Brown DF, Sinclair J, Chang Y, Thielker KZ, Nagurney JT. Patient and provider perceptions of why patients seek care in emergency departments. J Emerg Med. 2014;46(1):104–12. doi: 10.1016/j.jemermed.2013.04.063. Epub 2013 Sep 21. [DOI] [PubMed] [Google Scholar]
- 19.Marr S, Simpson D, Hillier LM, Vinson S, Goodwill S, Jewell D. How do older adults decide to visit the emergency department? [Abstract 315.] Can Geriatr J. 2016;19(3):142. doi: 10.12927/hcq.2019.25840. Available from: www.cgjonline.ca/index.php/cgj/article/view/245/315. Accessed 2018 Jul 6. [DOI] [PubMed] [Google Scholar]