Abstract
Background and Aims:
There is a paucity of literature on comparative effects of different inhalational anaesthetics in beach chair position (BCP) for shoulder arthroscopy. We aimed to investigate and compare the haemodynamic effects, anaesthetic and surgical outcomes between two inhalational agents.
Methods:
In this randomised study, patients of age 18–60 years, were allotted to two groups (29, sevoflurane and 28, isoflurane) and received protocol-based anaesthesia. Intraoperatively, different haemodynamic and other data were recorded.
Results:
All mean of averages of individual subject's vitals were comparable between the groups [P = 0.681, 0.325, 0.803, and 0.051, respectively for systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MBP) and heart rate (HR)]. Higher mean HR was recorded for maximum readings of isoflurane (P = 0.028). Equivalency was observed for SBP, MBP, and DBP (P = 0.000, 002, and 0.027, respectively). Process capability indices indicated that sevoflurane had better values (Pp: 0.55 versus 0.41, Ppk: 0.35 versus 0.22) for SBP as with MBP (Pp: 0.62 versus 0.51, Ppk: 0.36 versus 0.33). For achieving optimal vision, higher pump pressures (PPs) were demanded by surgeon (P = 0.025) and higher differences observed between initial and highest PPs (P = 0.027), in isoflurane subjects. Multivariable analysis revealed that no continuous predictor was able to predict the quality of vision except additional pump flow factor, for both groups.
Conclusion:
Both inhalational agents demonstrated equivalent haemodynamic effects. Increased arthroscopic PP requirements were observed with isoflurane anaesthesia. Sevoflurane may be superior to isoflurane during BCP arthroscopy.
Key words: Arthroscopy, block, brachial plexus, general anaesthesia, hemodynamic, inhalation anaesthesia, surgery
INTRODUCTION
Shoulder arthroscopic surgery is often performed in beach chair position (BCP). The effects of several anaesthetic techniques and agents for the procedure have been extensively studied.[1,2] Haemodynamic effects induced by BCP in anaesthetised patients are well-known.[3] Different inhalational agents at equivalent minimal alveolar concentration (MAC) dosages may exhibit dissimilar haemodynamic effects especially in patients with a prior interscalene plexus blockade (ISSB). While these observations could be accounted for by their established mechanisms of action, an unfamiliar yet plausible explanation could be the local anaesthetic-inhalational agent interaction.[4,5] Previous studies have shown that both sevoflurane and isoflurane reduce mean arterial blood pressure (MBP) to an equivalent magnitude but under different circumstances.[6,7]
Haemodynamic parameters are of prime importance in arthroscopic surgery due to their direct relationship with arthroscopic pump pressures (PPs), intra-articular bleed, and clarity of vision.[8] An agent which is capable of preserving autoregulation of cerebral blood flow would be the anaesthetic of choice.[9] Considering the comparability of isoflurane with sevoflurane at equal MAC, we investigated the hypothesis that both agents produce equivalent haemodynamic effects. Simultaneously, we investigated whether either drug has any additional advantage over the other using secondary outcome measures.
METHODS
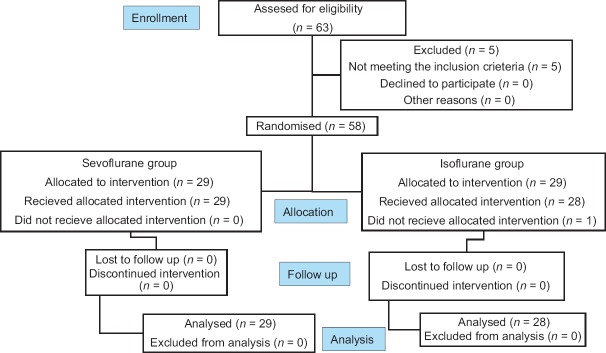
This prospective, randomised, parallel design study protocol was approved by the University's Institutional Ethical Committee. The trial was registered prior to patient enrolment at Clinical Trials of Registry of India (http://ctri.nic.in, CTRI/2016/04/006830). All patients gave informed consent. Randomly assigned (random number generator, Random#generator, application, Jess Tucker, version 1.1.3, 2013, Webberface, LLC, iOS application, Category: Utilities, info@webberface.com) patients belonging to American Society of Anesthesiologists (ASA) status I and II, 18–60 years of age, who underwent shoulder arthroscopic surgery over 16-month period (April 2016–August 2017) were enrolled [Figure 1]. Exclusion criteria included allergy to local anaesthetics, preexisting cerebrovascular disease, history of orthostatic hypotension, body mass index of 36 kg/m2 or more, impaired kidney function, and coagulopathy. Since an effective preliminary interscalene block formed an essential part of the anaesthetic procedure, patients in whom the regional block was not performed were excluded from the study [Figure 1].
Figure 1.
CONSORT flowchart study inclusion criteria
After preoperative assessment and recording of baseline vitals, patients were premedicated with oral ranitidine 150 mg, having fasted overnight before the surgical procedure. No sedatives or opioids were used for premedication.
In the operating room, patients were administered supplemental oxygen while they received intravenous (IV) fentanyl 1–2 μg/kg. Following local infiltration of the skin with 2%, 1 mL lignocaine, ultrasound-guided (SonoSite, M-turbo® system, SonoSite Inc., high frequency, linear 13-6 MHz transducer) interscalene, in-plane block was performed with mixture of 6 mL lignocaine 2% and 20 mL levobupivacaine 0.25% using 23-guage blunt-bevel needle. The effectiveness of the block was confirmed by absence of sensations over C5–C7 dermatomal distribution and/or free and painless abduction (passive) in patients with painful shoulders. This abolition of touch sensation was tested approximately 15 min later.
After measurements of the preinduction vitals and preoxygenation, anaesthesia was induced with IV propofol 2–2.8 mg/kg. Tracheal intubation was facilitated using IV vecuronium or rocuronium in 2*ED95 doses or succinylcholine 1.5 mg/kg and ventilation was instituted to achieve normocarbia. Five lead electrocardiogram, pulse oximetry, noninvasive blood pressure (in nonoperative upper arm), end-tidal carbon dioxide, and inhalational agent monitoring (Airway Gas Analyser, MDL 94267 OPT-L19; Spacelabs Healthcare, Inc. Snoqualmie, WA, USA) were done during the entire procedure.
Achieving BCP was done over approximately 10–15 min after induction of general anaesthesia. The head was secured in a neutral position. The back of operating table was then raised to 75°–85° above the horizontal plane. With the knees and hips in flexed positions, and the patients' feet resting on protective paddings, care was taken for positioning of arms and neck. Anaesthesia was maintained using either sevoflurane (Datum Vaporizer, MEDITEC England, Abbot Ltd) or isoflurane (Abbott loan vaporiser; Abbott Australia Pty. Ltd) at 1.2–1.5 iso-MAC dosages. Oxygen 33% and nitrous oxide (N2O) 67% mixture was used in both the groups. Age-related iso-MAC[10] inhalational concentrations (ChronoMAC, Application Timeline, version 1.0: 2011) were used to achieve the desired end-tidal concentrations for maintenance. Vecuronium- or rocuronium-induced neuromuscular blockade was carefully controlled by train of four (TOF) monitoring. Systolic blood pressure (SBP), diastolic blood pressure (DBP), MBP, and heart rate (HR) were recorded every third minute.
Standard protocol for maintenance of anaesthesia was followed. The minimum difference between the SBP and PP to begin the arthroscopy was 49 mmHg.[8] End-tidal inhalational agent concentration was adjusted to achieve 1.2–1.5 iso-MAC values for the respective agent during maintenance. Additional opioids and iso-MAC of inhaled agent were adjusted as shown in Supplementary Figure 1 (68.3KB, pdf) . Hypotension was defined as MBP less than 65 mmHg during the surgical period. If two successive readings were less than 65 mmHg, then a vasopressor (ephedrine 3–6 mg, IV) was used. The study interval considered was from insertion of the arthroscope to its removal. The arthroscopic automated pump (Continuous Wave III Arthroscopy Pump; Arthrex, Arthrex Med. Inst. GmbH, Germany) pressure was 30–40 mmHg and irrigate flow at 30%–40% was to begin with and maintained throughout the procedure. Requirement of increase or decrease in PPs and pump flow, as requested by surgeon, was documented. All patients were administered ondansetron IV, 4 mg, 30 min before the anticipated completion of the surgical procedure. Neuromuscular block was reversed with neostigmine 50–70 μg/kg and glycopyrrolate 10 μg/kg when TOF count of 4 was demonstrated.
Anaesthetic maintenance management protocol. The minimum difference between the SBP and arthroscopic PP to begin the arthroscopy was 49 mmHg ensured. End-tidal inhalational agent concentration was adjusted to achieve 1.2-1.5 iso-MAC values for the respective agent during maintenance of anaesthesia. Additional opioids and iso-MAC of inhaled agent were adjusted as shown. We intended to keep MBP above 65 mmHg. If two successive readings of MBP were recorded less than 65 mmHg, then a vasopressor would be considered. Opioid included fentanyl and vasopressor was ephedrine. Higher or lower iso-MAC would be considered for higher or lower SBP readings, accordingly. MAC - Minimal alveolar concentration, MBP - Mean blood pressure, SBP - Systolic blood pressure
The primary outcome variable was ‘haemodynamic parameters’ which included the recordings of all vitals. We recorded induction to incision time, duration of surgery, initial PPs, highest PP used, initial flow, highest flow used, total saline consumption, difference between highest and initial PPs and flows, average saline consumption/minute, and opioid consumption. The categorical visual analogue scale scores were rated by surgeon (who was blinded for the study) based on vision during arthroscopy as excellent = 4, good = 3, average = 2, and poor = 1. In addition, details of MAC adjustments, additional opioids, hypotension episodes, and vasopressor requirements were noted. All these constituted our secondary outcomes.
Our previous study on shoulder arthroscopy in lateral decubitus position (LDP) demonstrated approximately 10 mmHg mean difference of SBP between group subjects when different techniques and inhalational agents were compared.[11,12] Based on this, we calculated the sample size for this study. A minimum of 16 patients were required in each group to detect a mean BP difference of 10 mmHg [power 80%, α = 0.05, with standard deviation (SD) of 10 in each group] assuming that differences of <10 mmHg would not be clinically significant. However, we included a higher number of subjects since additional statistical methodology using process capability index (PCI) analysis for haemodynamic data evaluation necessitated a minimum number of 25 subjects in each group. A priori: compute sample size using two-tailed test (effect size of 1, critical t, 2.006, Df = 52) with 27 patients in each group revealed that the actual power of our study would be 95%. An assumption of 10% dropouts was made.
Statistical analysis was performed using Minitab® 17.1.0., © 2013 Minitab Inc. All data distribution analysis was checked using Shapiro–Wilk (Ryan–Joiner) test. Data were evaluated using different methods using conventional statistical tests, equivalent tests, PCIs, and multivariable analysis [Supplementary Figure 2 (224.9KB, pdf) ]. To test for the differences between study arms, patient characteristics were analysed using independent sample t tests for continuous variables or Mann–Whitney U test for nonparametric data. Mean (SD) and 95% confidence intervals (CIs) or median (range) were considered. Chi-square test was used to analyse categorical data.
Data analysis methods. 1. Mean (SD) of mean vitals for both groups, mean of maximum and minimum vitals, initial and highest PPs and flows, and its differences between the groups were compared. 2. Since SDs of individual patients were not considered during conventional evaluations, PCIs were used as additional method to evaluate an individual patient’s vitals’ fluctuations. 3. The two-sample equivalence independent tests were necessary since statistically proving ‘not being different’ is not as same as the ‘equivalent’. 4. Finally, an ordinal logistic regression analysis was used to find out the associations between visual grading and predictors influencing arthroscopic vision for both agents, separately. DBP - Diastolic blood pressure; HR - Heart rate; HP - Highest pressure; HF - Highest flow; HF - IFdiff - Difference between highest and initial pump flow; HP - IPdiff - Difference between highest and pump initial pressure; iso - Isoflurane; MBP - Mean blood pressure; max - Mean of maximum blood pressure or heart rate recorded for individual subject; mean - Mean of mean blood pressure or heart rate of individual subject; min - Mean of minimum blood pressure or heart rate recorded for individual subject; PCI - Process capability index; Pp and Ppk - Representation for process capability indices; SBP - Systolic blood pressure; SD - Standard deviation; sevo - Sevoflurane
Additional statistical analysis was done using equivalency tests and PCIs. Presuming the hypothesis of equivalency with respect to the haemodynamic effects of sevoflurane and isoflurane in patients undergoing shoulder arthroscopy, we used the two-sample equivalence tests.[13] This independent conclusion was necessary since statistically proving ‘not being different’ is not as same as ‘equivalent’. A two-sample equivalence test would test two separate null hypotheses in our study. First, the difference between sevoflurane haemodynamics was less than or equal to isoflurane lower limit for equivalence and second, the difference was greater than or equal to upper limit for equivalence. If mean, μ, denoted the average vitals of each group subjects, μsevo and μiso were individual averages for sevoflurane and isoflurane, respectively. The two one-sided test procedures required rejecting both of null hypotheses μsevo− μiso≥10 mmHg and μsevo− μiso <10 mmHg to declare the equivalence. If both null hypotheses were rejected, then the difference would fall within our equivalence interval and we could claim that the means for the vital readings were equivalent.
PCIs[11,14] were used to evaluate an individual patient's haemodynamic parameter fluctuations since SDs of individual patients were not assessed during conventional evaluations. We derived PCIs for the desired range of maintained SBP, that is, between 100 and 80 mmHg. These formed the upper specification limit (USL) and lower specification limit (LSL) of systolic pressures (SBP(100, 80)). Similar to SBPs, PCIs for MBPs and PP usage were derived for SLs, separately [SLs for MBP(80,60), PP(30,50)]. All PCI data were checked for distribution and data were transformed prior to analysis and derivation of indices. To determine the ability of the inhalational agent to maintain the blood pressure with respect to a predefined range (SL), the PCI, Pp was derived. To analyse whether the fluctuations deviated to higher or lower side of expected limits, the PCI, Ppk was considered.
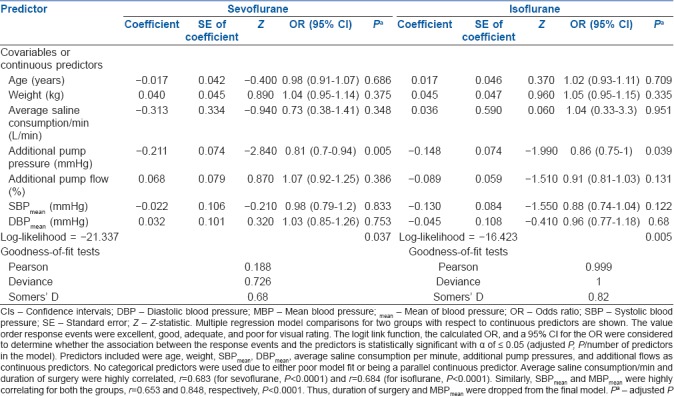
An ordinal logistic regression analysis was used to find out the associations between visual grading and predictors influencing arthroscopic vision for both agents, separately. Predictors included were age, weight, SBPmean, DBPmean, average saline consumption per minute, additional PPs, and additional flows. All primary and secondary outcomes were compared using a conventional α level of 0.05.
RESULTS
Of 63 patients who underwent shoulder arthroscopic surgeries, 1 patient who refused interscalene block on operative table did not meet the inclusion criteria. Five patients who had a different operating team were excluded prior to randomisation. The remaining 57 were analysed as per protocol.
The groups did not differ by age, sex, weight, and preinduction opioid use. Baseline vitals were comparable. Both groups received similar anaesthetic techniques with respect to regional or general anaesthesia. Surgical details with respect to type of surgical procedures, induction–incision time, surgical duration, initial PPs, and flows were comparable between the groups [Table 1].
Table 1.
Comparison of patient characteristics between the groups
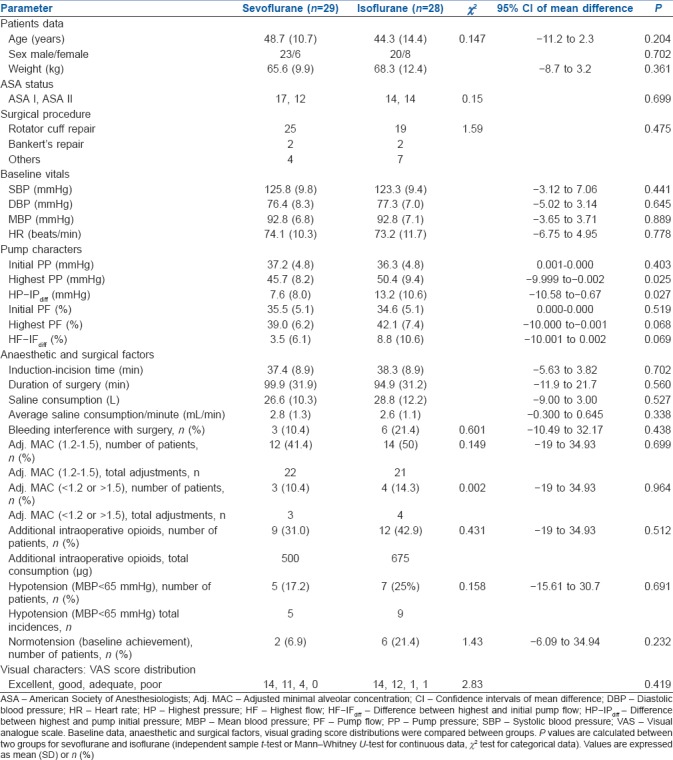
The primary independent variable was the SBP and covariables were DBP and MBP. The means of mean SBP, DBP, MBP, and HR recorded (for sevoflurane and isoflurane) were not different between the groups [Table 2]. The comprehensive list of maximum and minimum blood pressure and HR averages is included in Table 2.
Table 2.
Haemodynamic and arthroscopic pump characteristics comparisons

While analysing whether sevoflurane was equivalent to isoflurane in achieving haemodynamic status, two-sample equivalency test confirmed that both were equivalent for mean SBP (P = 0.017, for limits of 10 mmHg; P = 0.000, for limits of 5 mmHg; mean difference of −0.79, 95% CI of mean difference, −4.01 to 2.44). The equivalency test, P < 0.05, allowed the rejection of null hypothesis of ‘difference ≤ −10 mmHg or difference ≥10 mmHg’ and accepting an alternative hypothesis of ‘−10 mmHg < difference <10 mmHg’. This indicated equivalency between the groups. The test was repeated for limits of 5 mmHg, and rejection of null hypothesis was still possible. Similarly, mean MBPs and DBPs were found equivalent between the groups (limits 5 mmHg, CI: −2.18 to 2.95, P = 0.002 for MBP and limits 5 mmHg, CI: −1.147 to 4.492, P = 0.027 for DBP).
In contrast to blood pressures, we observed statistically significant higher HRmax averages in isoflurane subjects (CI: −12.4 to −0.7; P = 0.028, independent sample t test). MAC adjustments, opioid usage, and episodes of haemodynamic instabilities were found comparable between the groups. However, interestingly we noticed requirement of higher PPs and higher differences between initial and highest PPs for optimal vision in isoflurane subjects [CI: −9.99 to −0.002; P = 0.025 and CI: −10.58 to −0.67; P = 0.027, respectively, Table 1]. We found no difference between the groups for other pump parameters.
Since the data for PCI analysis were found as non-normal, a best fit three-parameter Weibull was considered based on the goodness-of-fit tests with lowest likelihood ratio test P values. After data transformation, the PCIs were derived for each group. The derived PCIs show subtle differences of Pp and Ppk of SBP and MBP recordings at predefined USLs and LSLs, between the groups [Table 2 and Figures 2, 3]. This suggested that the blood pressure readings of a larger number of isoflurane subjects had fallen above USLs. With respect to PPs, better PCI values suggested a consistent uniform intraoperative use of PPs in sevoflurane subjects.
Figure 2.
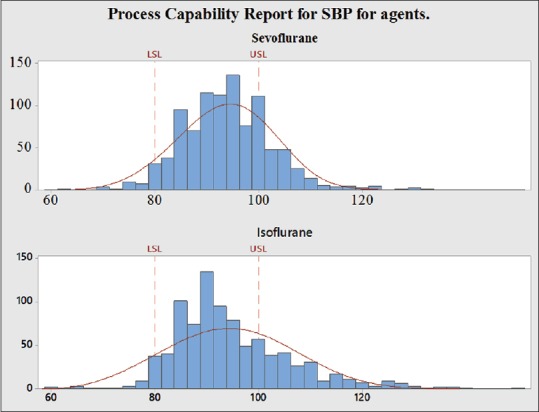
Process capability report for SBPs. Process capability report for SBPs of both groups, for overall processes for SLs (LSL and USL). The assembly fit data PCI values are shown for original (nontransformed) data. Data were transformed prior to derivation of PCIs. X-axis represents the systolic blood pressure readings. LSL (80 mmHg) and USL (100 mmHg) were considered for PCI evaluation. PCI, process capability index; SBP – Systolic blood pressure; LSL – Lower specification limit; USL – Upper specification limit
Figure 3.
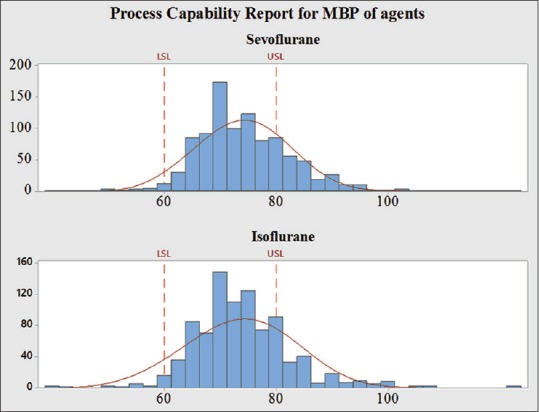
Process capability report for MBP. Process capability report for MBPs of both groups, for overall processes for SLs (LSL and USL). The assembly fit PCI data values are shown for original (nontransformed) data. Data were transformed prior to derivation of PCIs. X-axis represents the mean blood pressure readings. LSL (60 mmHg) and USL (80 mmHg) were considered for PCI evaluation. MBP – Mean blood pressure; LSL – Lower specification limit; PCI – Process capability index; USL – Upper specification limit
Logistic regression multivariable analysis revealed no continuous predictor was able to predict the quality of vision except additional pump flow requirement factor for each group [Table 3]. No other differences were noted between the groups with respect to any particular predictor. No perioperative major complications were noted.
Table 3.
Multiple regression model comparisons for two groups
DISCUSSION
During the trial, we attempted to study the haemodynamic parameters as they are directly linked to PPs, intra-articular bleeds, and clarity of vision during shoulder arthroscopy. A few previous studies did focus on comparing haemodynamic effects of different anaesthetic agents, but in the LDP.[11,12] In contrast to previous findings, we observed equivalent SBPs, MBPs, and HRmeans with both agents in BCP arthroscopy. While rejecting the null hypothesis, we also checked whether sevoflurane could achieve haemodynamic status equivalent with isoflurane.
Cardiovascular effects specific to sevoflurane and isoflurane have been described and compared in multiple studies on animals,[15] human volunteers,[7] and ASA I patients.[6] Decrease in arterial pressure for isoflurane and sevoflurane occurs as a consequence of reduction in left ventricular afterload. BCP augments this effect leading to further reductions. Concomitant administration of N2O may blunt the hypotensive effects.[7] Our study groups were comparable since N2O was used in all along with complete ISBB which created a pain-free status. A dose-dependent hypotensive effect for both the inhalational agents at 1–2 MAC has been established, each however having a different attributed mechanism of action.[16] Isoflurane causes increase in HR at 1.5–2 MAC anaesthesia probably in response to simultaneous decrease in arterial pressure, and this was reflected by higher HRmax values.[7] The influence of BCP on HR in the presence of an inhalational agent may be at variance with that observed with LDP.[17] Researchers have demonstrated sevoflurane's superiority over isoflurane in preserving baroreceptor reflexes[18,19] during 1–2 MAC anaesthesia, but this has, however, not been specifically related to BCP.
PCI evaluation demonstrated miniscule difference in the distribution of blood pressure patterns especially with SBP. Overall performance of sevoflurane in preserving SBPs between 80 and 100 mmHg was better. This possibly important clinical difference was not highlighted on conventional statistical analysis.
An interesting observation was the increased number of demands for higher PPs by the surgeon during isoflurane anaesthesia, clearly supported by lower PCI values. With the contingent surgeon's blinding for inhalational agent and blood pressures, the PPs were adjusted based only on visual factor. In the absence of literature evidences supporting this finding, we surmise a few factors that could be responsible for this. First, the surgical and anaesthetic factors listed out in the tables between the groups might collectively lead to higher PP requirements. Second but more important, isoflurane can produce more intense arteriolar dilatations in areas such as bones and joints which are richly vascularised, and this may create a self-perpetuating ooze hampering vision. Corroborative evidence to this effect is provided by a study demonstrating increased microvascular flow index and perfused vessel proportions in the sublingual microcirculation during coronary artery bypass grafting under isoflurane anaesthesia (compared with sevoflurane and desflurane).[20] Many other studies[21,22] claim similar effects with increased microcirculatory flows in animal organs though some are contradictory.[23] Tanaka et al.[24] explained isoflurane's mechanism of vasodilatation through protein kinases. Irrespective of these extrapolations, another factor influencing intraoperative intra-articular bleed could be the underlying pathology to begin with. A real-time in vivo laser Doppler study demonstrated higher microvascular blood flow in shoulders with normal rotator cuffs vis-a-vis pathological ones.[25] Our study had approximately 70% individuals with shoulder pathologies and the numbers were comparable between the groups.
It is uncertain whether the observed difference has resulted in clinically important changes in patient management. Low PPs reduce saline consumption, absorption, and swelling, allow easy surgical handling, and reduce postoperative pain and hospital stay. Model comparisons could identify no factor other than PPs that influenced visual scores. This is not to be confused with our finding of higher number of demands for increased PP during isoflurane anaesthesia. The final grading of visualisation aimed for is always 3 or higher for any arthroscopy to ensure smooth conduct of the procedure.
Where ischaemic brain damage related to BCP is a concern,[3] the ability of a specific inhalational agent to prevent this assumes importance. Although no single agent has yet emerged as a superior neuroprotective one,[26] few studies have shown some differences between sevoflurane and isoflurane. The superiority of sevoflurane over isoflurane in preserving dynamic cerebral autoregulation as measured by transcranial Doppler (TCD) of the middle cerebral artery blood velocity has been demonstrated.[27] Middle cerebral artery flow velocity when studied through TCD revealed least effects with sevoflurane compared with isoflurane.[9] The true instances of cerebral desaturation as detected by noninvasive near-infrared spectroscopic cerebral oximetry[28] had higher margin of safety with sevoflurane-N2O-based anaesthesia over other techniques.[29] Relatively lower PP requirements along with the neuroprotection advantage could make sevoflurane the logically preferred inhalational agent.
Our study has its limitations. The haemodynamic effects of MAC may be different for iso-MAC values and will be affected by use of additional opioids. Increased PPs may be demanded by surgeon at regular intervals, but the converse for a ‘decreased’ demand is less likely. Use of surgical shavers and radiofrequency devices may significantly amend the bleeding. Subjective scorings of visual grade are considered for the entire period, whereas bleeding episodes are sporadic. Bleeding during arthroscopy may depend on underlying shoulder pathology. Secondary outcome analysis may be underpowered. The sample size was a concern when the ordinal logistic regression analysis was used to analyse the visual grading, although the minimum sample size is not yet defined for such an analysis.
CONCLUSION
We conclude that both isoflurane and sevoflurane produced equivalent haemodynamic effects. We observed increased pump requirements with isoflurane anaesthesia. In this context, a future study with a larger sample size may confirm the superiority of one inhalational agent over the other.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors sincerely acknowledge Dr. Rajani Kadri, M.S., Associate Professor, Department of Opthalmology, A J I M S & Research Centre, Mangalore, for her excellent support, contribution, and cooperation during the preparation of article. They also thank Mr. Naveen Mishra for the kind help during article preperation.
REFERENCES
- 1.Janssen H, Stosch RV, Pöschl R, Büttner B, Bauer M, Hinz JM, et al. Blood pressure response to combined general anaesthesia/interscalene brachial plexus block for outpatient shoulder arthroscopy. BMC Anesthesiol. 2014;14:50. doi: 10.1186/1471-2253-14-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aguirre JA, Märzendorfer O, Brada M, Saporito A, Borgeat A, Bühler P, et al. Cerebral oxygenation in the beach chair position for shoulder surgery in regional anesthesia: Impact on cerebral blood flow and neurobehavioral outcome. J Clin Anesth. 2016;35:456–64. doi: 10.1016/j.jclinane.2016.08.035. [DOI] [PubMed] [Google Scholar]
- 3.Laflam A, Joshi B, Brady K, Yenokyan G, Brown C, Everett A, et al. Shoulder surgery in the beach chair position is associated with diminished cerebral autoregulation but no differences in postoperative cognition or brain injury biomarker levels compared with supine positioning: The anesthesia patient safety foundation beach chair study. Anesth Analg. 2015;120:176–85. doi: 10.1213/ANE.0000000000000455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takamura T, Sakamoto A, Ogawa R. Bupivacaine combined with isoflurane synergistically depressed myocardial contractility in rat working heart preparation. Nihon Ika Daigaku Zasshi. 1997;64:292–7. doi: 10.1272/jnms1923.64.292. [DOI] [PubMed] [Google Scholar]
- 5.Copeland SE, Ladd LA, Gu XQ, Mather LE. The effects of general anesthesia on whole body and regional pharmacokinetics of local anesthetics at toxic doses. Anesth Analg. 2008;106:1440–9. doi: 10.1213/ane.0b013e31816ba541. [DOI] [PubMed] [Google Scholar]
- 6.Frink EJ, Jr, Malan TP, Atlas M, Dominguez LM, DiNardo JA, Brown BR, Jr, et al. Clinical comparison of sevoflurane and isoflurane in healthy patients. Anesth Analg. 1992;74:241–5. doi: 10.1213/00000539-199202000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Malan TP, Jr, DiNardo JA, Isner RJ, Frink EJ, Jr, Goldberg M, Fenster PE, et al. Cardiovascular effects of sevoflurane compared with those of isoflurane in volunteers. Anesthesiology. 1995;83:918–28. doi: 10.1097/00000542-199511000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Morrison DS, Schaefer RK, Friedman RL. The relationship between subacromial space pressure, blood pressure, and visual clarity during arthroscopic subacromial decompression. Arthroscopy. 1995;11:557–60. doi: 10.1016/0749-8063(95)90131-0. [DOI] [PubMed] [Google Scholar]
- 9.Moppett IK, Mahajan RP. Transcranial Doppler ultrasonography in anaesthesia and intensive care. Br J Anaesth. 2004;93:710–24. doi: 10.1093/bja/aeh205. [DOI] [PubMed] [Google Scholar]
- 10.Nickalls RW, Mapleson WW. Age-related iso-MAC charts for isoflurane, sevoflurane and desflurane in man. Br J Anaesth. 2003;91:170–4. doi: 10.1093/bja/aeg132. [DOI] [PubMed] [Google Scholar]
- 11.Tantry TP, Karanth H, Shenoy SP, Ayya SV, Shetty PK, Adappa KK. Isoflurane versus sevoflurane with interscalene block for shoulder arthroscopic procedures: Value of process capability indices as an additional tool for data analysis. Indian J Anaesth. 2016;60:939–47. doi: 10.4103/0019-5049.195488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tantry TP, Muralishankar B, Adappa KK, Bhandary S, Shetty P, Shenoy SP. Target-controlled infusion (Propofol) versus inhaled anaesthetic (Sevoflurane) in patients undergoing shoulder arthroscopic surgery. Indian J Anaesth. 2013;57:35–40. doi: 10.4103/0019-5049.108559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henshaw DS, Jaffe JD, Reynolds JW, Dobson S, Russell GB, Weller RS, et al. An evaluation of ultrasound-guided adductor canal blockade for postoperative analgesia after medial unicondylar knee arthroplasty. Anesth Analg. 2016;122:1192–201. doi: 10.1213/ANE.0000000000001162. [DOI] [PubMed] [Google Scholar]
- 14.Senvar O, Tozan H. Fuerstner I, editor. Process capability and six sigma methodology including fuzzy and lean approaches. Products and Services; from R and D to Final Solutions. 2010. [Last accessed on 2018 Feb 01]. pp. 153–78. Available from: http://www.intechopen.com/books/products-and-services-from-r-d-to-finalsolutions/process-capability-and-six-sigma-methodology-including-fuzzy-and-lean-approaches .
- 15.Raisis AL, Blissitt KJ, Henley W, Rogers K, Adams V, Young LE, et al. The effects of halothane and isoflurane on cardiovascular function in laterally recumbent horses. Br J Anaesth. 2005;95:317–25. doi: 10.1093/bja/aei180. [DOI] [PubMed] [Google Scholar]
- 16.Eger EI. Inhaled anesthetics: Uptake and distribution. In: Miller RD, editor. Miller's Anaesthesia. Philadelphia: Churchill Livingstone; 2010. pp. 531–59. [Google Scholar]
- 17.Rains DD, Rooke GA, Wahl CJ. Pathomechanisms and complications related to patient positioning and anesthesia during shoulder arthroscopy. Arthroscopy. 2011;27:532–41. doi: 10.1016/j.arthro.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 18.Adachi H. Sevoflurane anesthesia maintains reflex tachycardia on position change from supine recumbent to head-up tilt. J Anesth. 1996;10:129–32. doi: 10.1007/BF02483349. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka M, Nishikawa T. Sevoflurane speeds recovery of baroreflex control of heart rate after minor surgical procedures compared with isoflurane. Anesth Analg. 1999;89:284–9. doi: 10.1097/00000539-199908000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Özarslan NG, Ayhan B, Kanbak M, Çelebioğlu B, Demircin M, Ince C, et al. Comparison of the effects of sevoflurane, isoflurane, and desflurane on microcirculation in coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2012;26:791–8. doi: 10.1053/j.jvca.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 21.Schumacher J, Pörksen M, Klotz KF. Effects of isoflurane, enflurane, and halothane on skeletal muscle microcirculation in the endotoxemic rat. J Crit Care. 2001;16:1–7. doi: 10.1053/jcrc.2001.21790. [DOI] [PubMed] [Google Scholar]
- 22.Hartman JC, Pagel PS, Proctor LT, Kampine JP, Schmeling WT, Warltier DC, et al. Influence of desflurane, isoflurane and halothane on regional tissue perfusion in dogs. Can J Anaesth. 1992;39:877–87. doi: 10.1007/BF03008300. [DOI] [PubMed] [Google Scholar]
- 23.O'Riordan J, O'Beirne HA, Young Y, Bellamy MC. Effects of desflurane and isoflurane on splanchnic microcirculation during major surgery. Br J Anaesth. 1997;78:95–6. doi: 10.1093/bja/78.1.95. [DOI] [PubMed] [Google Scholar]
- 24.Tanaka K, Kawano T, Nakamura A, Nazari H, Kawahito S, Oshita S, et al. Isoflurane activates sarcolemmal adenosine triphosphate-sensitive potassium channels in vascular smooth muscle cells: A role for protein kinase A. Anesthesiology. 2007;106:984–91. doi: 10.1097/01.anes.0000265158.47556.73. [DOI] [PubMed] [Google Scholar]
- 25.Karthikeyan S, Griffin DR, Parsons N, Lawrence TM, Modi CS, Drew SJ, et al. Microvascular blood flow in normal and pathologic rotator cuffs. J Shoulder Elbow Surg. 2015;24:1954–60. doi: 10.1016/j.jse.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 26.Matchett GA, Allard MW, Martin RD, Zhang JH. Neuroprotective effect of volatile anesthetic agents: Molecular mechanisms. Neurol Res. 2009;31:128–34. doi: 10.1179/174313209X393546. [DOI] [PubMed] [Google Scholar]
- 27.Summors AC, Gupta AK, Matta BF. Dynamic cerebral autoregulation during sevoflurane anesthesia: A comparison with isoflurane. Anesth Analg. 1999;88:341–5. doi: 10.1097/00000539-199902000-00022. [DOI] [PubMed] [Google Scholar]
- 28.Murphy GS, Szokol JW, Marymont JH, Greenberg SB, Avram MJ, Vender JS, et al. Cerebral oxygen desaturation events assessed by near-infrared spectroscopy during shoulder arthroscopy in the beach chair and lateral decubitus positions. Anesth Analg. 2010;111:496–505. doi: 10.1213/ANE.0b013e3181e33bd9. [DOI] [PubMed] [Google Scholar]
- 29.Jeong H, Jeong S, Lim HJ, Lee J, Yoo KY. Cerebral oxygen saturation measured by near-infrared spectroscopy and jugular venous bulb oxygen saturation during arthroscopic shoulder surgery in beach chair position under sevoflurane-nitrous oxide or propofol-remifentanil anesthesia. Anesthesiology. 2012;116:1047–56. doi: 10.1097/ALN.0b013e31825154d2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Anaesthetic maintenance management protocol. The minimum difference between the SBP and arthroscopic PP to begin the arthroscopy was 49 mmHg ensured. End-tidal inhalational agent concentration was adjusted to achieve 1.2-1.5 iso-MAC values for the respective agent during maintenance of anaesthesia. Additional opioids and iso-MAC of inhaled agent were adjusted as shown. We intended to keep MBP above 65 mmHg. If two successive readings of MBP were recorded less than 65 mmHg, then a vasopressor would be considered. Opioid included fentanyl and vasopressor was ephedrine. Higher or lower iso-MAC would be considered for higher or lower SBP readings, accordingly. MAC - Minimal alveolar concentration, MBP - Mean blood pressure, SBP - Systolic blood pressure
Data analysis methods. 1. Mean (SD) of mean vitals for both groups, mean of maximum and minimum vitals, initial and highest PPs and flows, and its differences between the groups were compared. 2. Since SDs of individual patients were not considered during conventional evaluations, PCIs were used as additional method to evaluate an individual patient’s vitals’ fluctuations. 3. The two-sample equivalence independent tests were necessary since statistically proving ‘not being different’ is not as same as the ‘equivalent’. 4. Finally, an ordinal logistic regression analysis was used to find out the associations between visual grading and predictors influencing arthroscopic vision for both agents, separately. DBP - Diastolic blood pressure; HR - Heart rate; HP - Highest pressure; HF - Highest flow; HF - IFdiff - Difference between highest and initial pump flow; HP - IPdiff - Difference between highest and pump initial pressure; iso - Isoflurane; MBP - Mean blood pressure; max - Mean of maximum blood pressure or heart rate recorded for individual subject; mean - Mean of mean blood pressure or heart rate of individual subject; min - Mean of minimum blood pressure or heart rate recorded for individual subject; PCI - Process capability index; Pp and Ppk - Representation for process capability indices; SBP - Systolic blood pressure; SD - Standard deviation; sevo - Sevoflurane