Abstract
Introduction:
Serum neuron-specific enolase (NSE) levels have been shown to correlate with neurologic outcome in comatose survivors of cardiac arrest but use of absolute NSE thresholds is limited. This study describes and evaluates a novel approach to analyzing NSE, the NSE ratio, and evaluates the prognostic utility of NSE absolute value thresholds and trends over time.
Methods:
100 consecutive adult comatose cardiac arrest survivors were prospectively enrolled. NSE levels were assessed at 24, 48, and 72 hours post-arrest. Primary outcome was the Glasgow Outcome Score (GOS) at 6 months post-arrest; good outcome was defined as GOS 3-5. Absolute and relative NSE values (i.e. the NSE ratio), peak values, and the trend in NSE over 72 hours were analyzed.
Results:
98 patients were included. 42 (43%) had a good outcome. Five good outcome patients had peak NSE >33 μg/L (34.9 – 46.4 μg/L), NSE trends between 24 and 48 hours differed between outcome groups (decrease by 3.0 μg/L (0.9–7.0 μg/L) vs. increase by 13.4 μg/L (−3.7 – 69.4 μg/L), good vs. poor, p=0.004). The 48:24 hour NSE ratio differed between the good and poor outcome groups (0.8 (0.6–0.9) vs. 1.4 (0.8–2.5), p=0.001), and a 48:24 hour ratio of ≥1.7 was 100% specific for poor outcome.
Conclusions:
The NSE ratio is a unique method to quantify NSE changes over time. Values greater than 1.0 indicate increasing NSE and may be reflective of ongoing neuronal injury. The NSE ratio obviates the need for an absolute value cut-off.
Keywords: therapeutic hypothermia, anoxic brain injury, prognostication, neuron specific enolase, cardiac arrest
Introduction
Over 500,000 cardiac arrests occur in the United States each year,1 and only a minority of patients recover with good neurologic outcome.2 In comatose survivors of cardiac arrest, targeted temperature management (TTM), which includes therapeutic hypothermia (TH), improves neurologic outcomes.3-6 With widespread implementation of TTM and resultant altered clearance of sedative medication, accurate prognostication of functional outcomes is unreliable, especially in the early period after injury.7-10 The ethical and economic implications of inaccurate prognostication are vast; clinicians must balance inappropriately pessimistic prognostication which may lead to self-fulfilling prophecies of poor outcome with prolonged care for patients who never recover meaningful neurologic function. 11, 12 Better outcome prediction tools are needed that maintain specificity in patients treated with TTM.
Neuron-specific enolase (NSE) is an intracellular glycolytic enzyme, mainly expressed by neurons, which becomes detectable in serum and CSF after neuronal injury.13, 14 NSE levels are a marker of brain injury severity in comatose cardiac arrest survivors, and the NSE level in the first 72 hours after cardiac arrest has historically been recommended as a prognostic variable.15 An NSE level >33 μg/L obtained within 72 hours after cardiac arrest was previously reported as 100% specific for predicting poor outcome defined as death or a persistent vegetative state.16 However, the data were based largely on one prospective cohort study performed prior to the widespread implementation of TTM.16 More recent studies performed in the era of TTM have reported false positives rate as high as 29.3% when the 33 μg/L threshold was used,10 and other studies have reported varying threshold levels for predicting poor outcome with 100% specificity.17-22 Adding to the confusion, recent work from our group showed that serum NSE levels of comatose cardiac arrest patient differ between laboratories, though reassuringly TTM did not affect the relationship.23 All of this highlights the importance of developing a better NSE metric that is not based on absolute value thresholds and not susceptible to laboratory and analytical method variation.
Serial measurements of NSE may improve its diagnostic utility over using absolute values at single time-points. Additional studies have suggested that NSE kinetics were predictive of outcome, with increases in NSE over the first days after cardiac arrest correlating with poor outcome with a higher specificity than absolute values.20,24-26 A sub-analysis of over 900 patients from a large, prospective trial of targeted temperature management also suggested that increasing NSE between two time-points after cardiac arrest was associated with poor outcome.27 However, the optimal timing of repeat NSE measurements is unknown.
We hypothesized that serial NSE measurements would improve the prognostic power of NSE, and assessed serum NSE levels at 24, 48, and 72 hours after cardiac arrest in a prospectively enrolled cohort. The objectives were to evaluate performance of NSE as a prognostic biomarker based on the timing of the assessment, the absolute value thresholds and changes over time, and to describe and evaluate performance of a novel NSE-based prognostic biomarker, the NSE ratio.
Methods
Consecutive adult patients (age ≥ 18 years) admitted to the intensive care units at an academic tertiary medical center after resuscitation from cardiac arrest were screened for enrollment. Patients were eligible for enrollment if they had persistent coma, defined by absence of eye opening and lack of response to verbal commands, after return of spontaneous circulation. Enrollment was not limited by cardiac arrest characteristics, and patients were eligible if the cardiac arrest occurred in-hospital or out-of-hospital. Patients with ventricular tachycardia, ventricular fibrillation, pulseless electrical activity, and asystole were all eligible for inclusion. Patients were excluded if they had: pre-existing do-not-resuscitate (DNR) orders, pregnancy, terminal or severe coexisting systemic disease limiting life expectancy, active enrollment in experimental drug therapies/procedures which could interfere with the study, or lack of a surrogate decision maker to provide informed consent. A good outcome was defined as a Glasgow Outcome Score (GOS) of 3-5 at 6 months post-arrest; poor outcome was defined as GOS 1-2. The methods for outcomes assessments have been described previously (Tong, 2016). The institutional review board approved the study, and a surrogate provided informed consent.
Serum samples were obtained at 24 ± 4, 48 ± 4, and 72 ± 4 hours after the arrest and assessed for NSE levels. Samples were stored and processed per institutional protocol and sent to ARUP Laboratories (Stanford Hospital’s referral laboratory in Salt Lake City, Utah). ARUP laboratories performed enzyme-linked immunosorbent assay using the CanAg_NSE enzyme immunoassay with reference interval 3.7–8.9 μg/L.
All comatose post-cardiac arrest patients were admitted to an intensive care unit with neurocritical care team co-management. The underlying cause of the cardiac arrest was treated per standard care. Patients who qualified were treated with therapeutic hypothermia to a target temperature of 33 ± 0.5 °C degrees Celsius for 24 hours, re-warmed in a controlled manner over the subsequent 24 hours, and maintained with controlled normothermia for an additional 24 hours. Contraindications to therapeutic hypothermia were active bleeding, refractory hypotension (requiring >3 vasopressors to maintain adequate blood pressure), and time >24 hours since cardiac arrest.
The neurocritical care team treated all cardiac arrest patients maximally for at least 72 hours after the cardiac arrest, unless goals of care were changed for non-neurologic reasons (i.e. recurrent cardiac arrest, multi-organ failure, previously expressed wishes, etc). After 72 hours post-arrest and after at least 24 hours of normothermia, the overall clinical picture and available prognostic markers including the clinical exam, NSE, SSEPs, and MRI were assessed and prognosis was discussed with family. Historic predictors of prognosis were combined with additional clinical information such as MRI and NSE and a multi-modal approach to prognostication was used. Historic predictors of poor neurologic prognosis were considered any of the following: a motor score on the Glasgow Coma Scale ≤2, no pupillary reflexes, no corneal reflexes, or absent N20 cortical response on SSEPs. If prognosis was indeterminate, then care was recommended to continue and was re-assessed daily thereafter. The NSE values were available to the treatment team, though the NSE ratio was not calculated during the clinical study period and therefore was not used by the clinical teams.
Data were analyzed using Microsoft Excel 2010 (Redmond, WA, USA) and IBM SPSS version 22 (SPSS, Chicago, IL, USA). Descriptive parameters are presented as counts and percentages (%) for categorical data, mean ± standard deviation (SD) or median (inter-quartile range, IQR) for continuous data. Absolute and relative NSE values, peak values, and the trends in NSE values over 72 hours were correlated with outcome. The association between NSE parameters and dichotomized neurologic outcome was assessed with the Mann-Whitney U test. The NSE ratio is the ratio between NSE levels at two time-points, with values ≥ 1.0 representing stable (if ratio=1.0) or increasing (if ratio >1.0) NSE levels between two time-points. By comparing the 48 or 72 hour NSE value to the 24 hour NSE value, the ratio negates the need to standardize absolute values. The 48:24 hours NSE ratios were analyzed with Youdens Index to identify optimal sensitivity and specificity. Logistic regression and receiver operating curve (ROC) analysis were performed to assess the performance of NSE metrics in predicting neurologic outcome.
Results
100 subjects were enrolled from October 2008 to January 2014. One patient withdrew consent and one patient was subsequently deemed to have not had a cardiac arrest, leaving 98 subjects for the analysis. 42 patients (43%) had favorable 6 month outcomes (Table 1). 61 (62%) patients had out of hospital cardiac arrest, and the most common initial rhythm encountered was pulseless electrical activity (n=43, 44%) followed by ventricular fibrillation or pulseless ventricular tachycardia (n=36, 36%). Mean duration of cardiac arrest until return of spontaneous circulation (ROSC) was 20 (IQR 12-30) minutes, with no significant difference between favorable and poor outcome groups (p=0.68). 79 (81%) patients were treated with TH. Reasons for not undergoing TH were resolution of coma prior to initiation of TH, hemodynamic instability requiring ≥ 3 vasopressors, or active bleeding. Additional demographic and clinical data are presented in Table 1.
Table 1.
Clinical Characteristics
| Outcome | p-value | |||
|---|---|---|---|---|
| Overall | Good | Poor | ||
| N=98 | N=42 | N=55 | ||
| Mean age±SD, yr | 57±18 | 58±18 | 61±17 | 0.009 |
| Female sex, n (%) | 39 (40) | 18 (43) | 20 (36) | 0.52 |
| Diabetes mellitus, n (%) | 22 (22) | 7 (17) | 15 (27) | 0.22 |
| Hypertension, n (%) | 46 (47) | 19 (45) | 27 (49) | 0.71 |
| Coronary artery disease, n (%) | 22 (22) | 7 (17) | 15 (27) | 0.22 |
| Cardiac arrest duration median (IQR) (minutes) (n=38 & 53) |
20 (12-30) | 20 (10-30) | 20 (15- 25) |
0.68 |
| In-hospital cardiac arrest, n (%) | 37 (38) | 12 (29) | 25 (46) | 0.077 |
| Presenting rhythm, n (%) | 0.044 | |||
| VF/VT | 36 (37) | 21 (50) | 15 (27) | |
| PEA | 42 (43) | 13 (31) | 29 (53) | |
| Asystole | 13 (13) | 4 (10) | 9 (16) | |
| Other | 6 (6) | 4 (10) | 2 (4) | |
| Therapeutic hypothermia, n (%) | 79 (81) | 36 (86) | 42 (76) | 0.25 |
| 1 unknown | ||||
All patients in the poor outcome group died. At the time of death, three patients were deceased by neurologic criteria, 42 patients (76%) were on comfort care, and 4 patients (7.5%) died despite full ongoing support. Reasons for comfort care were untreatable medical condition (n=3) and patient or surrogate’s wishes (n=32). The presence of other historic outcome predictors and the support status at the time of death is further detailed in Table 2.
Table 2: Performance of NSE ratio in predicting outcome compared to absolute NSE threshold and historic outcome predictors.
Optimal thresholds for 48:24 and 72:24 hour NSE ratios to obtain 100% specificity were computed and their test characteristics were compared to the performance of traditional NSE cutoff of 33 μg/L and historic outcome predictors.
| Sensitivity (95% CI) | Specificity (95% CI) | AUC (95% CI) | |
|---|---|---|---|
| 48 h NSE > 33 μg/L |
0.64 (0.45-0.79) |
0.91 (0.70-0.98) |
0.88 (0.80-0.97) |
| 72 h NSE > 33 μg/L |
0.60 (0.41-0.77) |
1.0 (0.79-1.0) | 0.88 (0.78-0.98) |
| Max NSE within 72 h |
0.73 (0.54-0.87) |
0.74 (0.49-0.90) |
0.82 (0.73-0.90) |
| 48:24 ratio (1.7) |
0.39 (0.23-0.58) |
1.0 (0.82-1.0) |
0.76 (0.63-0.88) |
| 72:24 ratio (1.3) |
0.50 (0.32-0.68) |
1.0 (0.79-1.0) |
0.78 (0.65-0.91) |
| Pupil reactivity | 0.26 (0.15-0.41) |
1.0 (0.89-1.0) |
0.88 (0.80-0.97) |
| Corneal reflexes | 0.40 (0.26-0.55) |
0.92 (0.77-0.98) |
|
| Motor response | 0.72 (0.57-0.83) |
0.85 (0.70-0.94) |
|
| Any of the historic predictors |
0.80 (0.66-0.89) |
0.84 (0.68-0.93) |
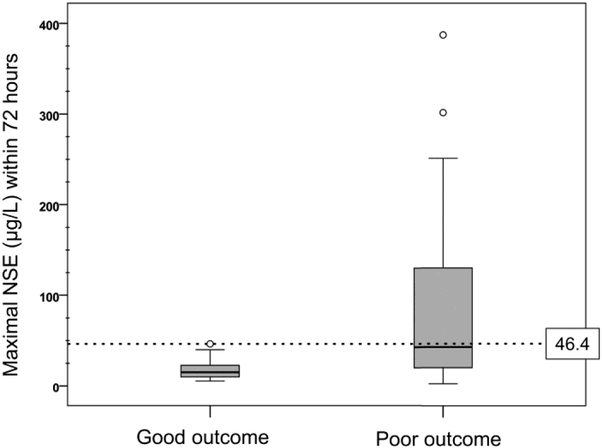
Eighty-six patients (88%) had NSE levels assessed at least once within 72 hours from cardiac arrest. The median of maximal NSE levels obtained within 72 hours was significantly different between good and poor outcome groups (15.1 μg /L, IQR 9.9–22.7 vs. 42.7 μg /L, IQR 19.9–130; good vs. poor, p<0.001) (Figure 1). Five patients (12%) with good outcome had NSE levels greater than 33.3 μg /L (range 34.9–46.4). In order to achieve 100% specificity for poor outcome, the NSE cut-off level was 41.4 mcg/L at 24 hours (41% sensitivity, AUC 0.77, 95% CI 0.66–0.88), 49.1 μg /L at 48 hours (45% sensitivity, AUC 0.82, 95% CI 0.73–0.92), and 32.6 μg /L at 72 hours (54% sensitivity, AUC 0.85, 95% CI 0.76–0.94). When maximal values of NSE obtained within 72 hours were considered, levels greater than 58.2 μg /L had 100% specificity with 47% sensitivity (AUC 0.82, 95% CI 0.73–0.90). In 44 patients who had NSE measured for all three time points, both 48 hour and 72 hour time points performed better than the 24 hour time point with thresholds of 41.4 μg /L (AUC 0.85, 95% CI 0.73–0.96), 49.1 μg /L (AUC 0.92 95% CI 0.84–0.99) and 32.6 μg/L (AUC 0.92, 95% CI 0.84-1.0), though the difference was not statistically significant. Patients with seizures had higher median 72-hour NSE levels (39.3 μg /L (20.4-129.3) vs. 19.8 μg /L (14.3-44.6), p=0.050). There was no difference in NSE levels based on TTM treatment (p=0.80) in the entire cohort or in outcome-adjusted groups (p=0.98).
Figure 1: Maximal NSE level within first 72 hours after cardiac arrest.
Maximal NSE levels in first 72 hours after cardiac arrest were significantly higher among patients with poor outcome. Two outlier values (556 and 892 μg /L) in patients with poor outcome are not shown. Dashed line: maximal NSE value within 72 hours for patients with favorable outcome
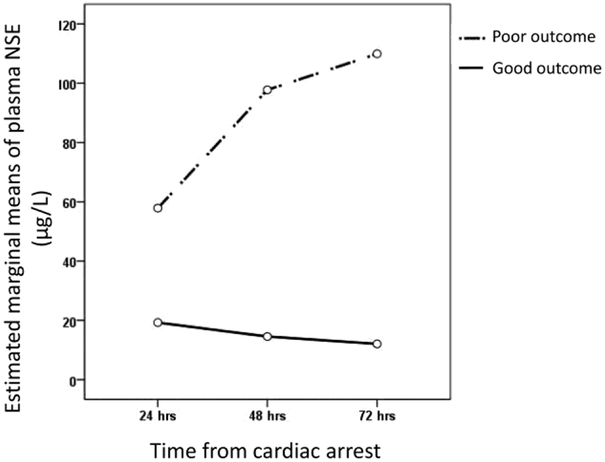
The change in NSE levels over time differed between good and poor outcome groups. Subjects with good outcomes had decreasing levels of NSE levels between 24-48 hours while patients with poor outcomes had increasing levels (decrease by 3.0 (0.9-7.0) vs. increase by 13.4 (−3.7 – 69.4) μg/L, good vs. poor, p=0.004) (Figure 2). This trend appears to continue between 48-72 hours but was not significant (decrease of 1.6 (0.3-4.3) vs. increase of 2.2 (−7.3 – 11.7), good vs. poor, p=0.219).
Figure 2: NSE trends over first 72 hours after cardiac arrest.
Patients with poor outcomes had increasing levels of NSE over first 72 hours post-arrest, while those with good outcomes had decreasing levels.
The 48:24 hour NSE ratio differed between the good and poor outcome groups (0.8 (0.6-0.9) vs. 1.4 (0.8-2.5), good vs. poor, p=0.001) (Figure 3). The 48:24 hour NSE ratio had an AUC of 0.76 (95% CI 0.63 – 0.88). We also identified the optimal 48:24 hour NSE ratio based on Youden’s Index to optimize both sensitivity and specificity, finding that a ratio of 1.0 yielded the highest Youden’s Index with a sensitivity of 64% and a specificity of 85%. We then identified 1.7 as the 48:24 hour NSE ratio that would yield 100% specificity (sensitivity 39%). Comparing the 48:24 hour NSE ratio of 1.7 to the absolute value cut-off of 33ug/L at 48 hours, the ratio had a slightly higher specificity (100% (95% CI 0.82 – 1.0) vs. 91% (95% CI 0.70 – 0.98), ratio vs. absolute value, p=0.49) with lower sensitivity (39% (95% CI 0.23 – 0.58) vs. 64% (95% CI 0.45 – 0.79), ratio vs. absolute value, p=0.08), though neither of these differences were significant (Table 2).
Figure 3: 48:24 hour and 72:24 hour NSE ratios differ between outcome groups.
The 48:24 hour (A) and 72:24 hour (B) NSE ratios were significantly higher in patients with poor outcome.
The predictive value of the 72:24 hour NSE ratio was similarly investigated. The 72:24 hour NSE ratio was significantly higher in the poor outcome group (0.6 (04. – 0.9) vs 1.6 (0.7 – 3.1), good vs. poor, p=0.001) (Figure 3), and the 72:24 hour NSE ratio had an AUC of 0.78 (95% CI 0.65 – 0.91). A 72:24 hour NSE ratio of 1.3 was 100% specific for poor outcome (with sensitivity 50% (95% CI 0.32 – 0.68)). Comparing the 72:24 hour NSE ratio of 1.3 to the absolute value cut-off of 33ug/L at 72 hours, the ratio performed equally as well (sensitivity 50% (95% CI 0.32 – 0.68) vs. 60% (95% CI 0.41 – 0.77), ratio vs. absolute value, p=0.60; specificity 100% (95% CI 0.79 – 1.0) vs. 100% (95% CI 0.79 – 1.0), ratio vs. absolute value, p=1) (Table 2).
Discussion
In this prospective cohort of comatose post-cardiac arrest patients, increasing NSE levels in the first 72 hours post-cardiac arrest were associated with poor outcome. We again showed that an absolute cut-off value for NSE was difficult to determine, the cut-off varied over different time-points post-arrest, and the previously accepted paradigm of using NSE>33 μg /L as a 100% specific cut-off value is no longer valid (with five good outcome patients in this cohort having NSE values that exceeded this threshold). We also described a novel metric to evaluate NSE, the NSE ratio. The 48:24 hour NSE ratio and the 72:24 hour NSE ratio were both predictive of poor outcome, with values ≥1.0 corresponding to increasing NSE levels over the allotted time and reflecting the pattern of increasing NSE levels in patients with poor outcome. The NSE ratio performed with good specificity and similar sensitivity to absolute value thresholds, but it provides several advantages over any NSE test that utilizes absolute values. The NSE ratio negates concerns about laboratory variability and the need to identify absolute thresholds in either total value or degree of change between two time-points. The ratio can be universally generalized and provide internal local consistency.
NSE has a biological half-life of 24 hours,17 so increasing levels over the initial days after cardiac arrest may suggest continued release of NSE, possibly reflecting ongoing secondary neurologic injury and association with poor outcome. Previous studies have shown that increases in NSE over 24 to 48 hours post-arrest correlate with poor outcome, including the data from one large multi-center trial showing NSE levels increased by 6 ng/mL between time points (24 to 48 hours and 48 to 72 hours) in the poor outcome group, while NSE levels decreased by 3-4 ng/mL in the good outcome group.20,25,27 Our results echo these findings showing that increases in NSE over time are more generalizable than absolute cut-off values, and the newly described NSE ratio quantifies these trends.
With regards to the historic use of absolute threshold values for NSE, the cut-off values in this cohort are similar to cut-offs reported in other more recent studies.20,24,27 Even higher cut-off values have been reported in other studies using a similar patient population undergoing TH, with good outcomes reported in patients with NSE levels up to 97 μg /L.28 While NSE levels did not differ in our cohort between patients treated with TH or patients who were not able to be treated, the number of patients who did not undergo TH was low. The reported effect of TH on NSE levels and the predictive value of NSE in patients treated with TH vary, with some studies reporting temperature did not affect NSE levels,27 other studies showing lower NSE levels in patients treated with TH, and still others reporting good neurologic outcomes despite higher NSE levels compared to non-TH-treated controls.17, 25, 28, 29 This further supports the idea that absolute NSE value thresholds are not generalizable.
Limitations are important to address. The relatively small sample size and single-center location may limit generalizability. Additionally, our primary outcome measure was the Glasgow Outcome Scale while many other studies use a Cerebral Performance Category (CPC) or modified Rankin Scale, though the GOS scale is virtually identical to the CPC. The primary outcome assessment at 6 months is a strength.30 NSE values may be falsely elevated with hemolysis, which may affect analysis, and we did not perform a hemolysis index on our samples. Lastly, NSE values were available to the clinicians during the study for incorporation in to prognostic assessments, although the NSE ratio was not described or computed. The clinicians did have the NSE trend available to them which could have impacted clinical decision making, though the clear prognostic algorithm described above was followed and prognostic decisions were not based on any single diagnostic test or exam finding.
As with previous guidelines that use NSE as a post-cardiac arrest biomarker, it is tempting to approach the newly described NSE ratio much in the same way and try to identify a particular ratio that can be used as a cut-off to delineate good and poor outcome groups with high sensitivity and specificity. Our intention is not necessarily to identify an absolute NSE ratio threshold, as this is unlikely feasible in the current era of critical care management for post-cardiac arrest patients with significant patient heterogeneity. Rather, our goal is to report the novel metric, show its performance in our cohort, demonstrate that it is a better measure to quantify NSE trends, and suggest that additional validation can be done in larger cohorts to better identify NSE ratio threshold(s) that can be used in multi-modal outcome prediction.31
Conclusions
Increasing serum NSE concentrations over the first 48 hours, 48:24 hour and 72:24 hour NSE ratios ≥1.0, and high absolute NSE levels correlate with poor neurological outcome in patients who are comatose after resuscitation from cardiac arrest. While the magnitude of NSE may reflect neurologic injury severity, trends in serial levels may represent evidence of ongoing injury and efficacy of neuro-protective efforts and could potentially be used to guide therapeutic interventions. Identifying an NSE cut-off value that is 100% specific for poor outcome across different patient populations and laboratories is not feasible, and the NSE ratio may be a more generalizable predictor. Outcome prediction in comatose survivors of cardiac arrest should not be based on a single parameter.
Highlights:
The NSE ratio is a unique method to quantify NSE changes over time.
NSE ratio > 1.0 indicates increasing NSE and may be reflective of ongoing neuronal injury.
A 48:24 hour NSE ratio >1.7 was 100% specific for poor outcome in this population.
Identifying an absolute value NSE cut-off value that is 100% specific for poor outcome across different patient populations and laboratories is not feasible, and thus the NSE ratio may be a more generalizable predictor.
Acknowledgments
This project was funded by the National Institute of Health (NIH), grant #5R01HL089116-04.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
All work was performed at Stanford University.
The authors have no other conflicts of interest to declare.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. January 27 2015;131(4):e29–322. [DOI] [PubMed] [Google Scholar]
- 2.McNally B, Robb R, Mehta M, et al. Out-of-hospital cardiac arrest surveillance --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010. MMWR Surveill Summ. July 29 2011;60(8):1–19. [PubMed] [Google Scholar]
- 3.Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. February 21 2002;346(8):557–563. [DOI] [PubMed] [Google Scholar]
- 4.Nielsen N, Wetterslev J, Cronberg T, et al. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N Engl J Med. December 5 2013;369(23):2197–2206. [DOI] [PubMed] [Google Scholar]
- 5.Cronberg T, Lilja G, Horn J, et al. Neurologic Function and Health-Related Quality of Life in Patients Following Targeted Temperature Management at 33 degrees C vs 36 degrees C After Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA Neurol. June 2015;72(6):634–641. [DOI] [PubMed] [Google Scholar]
- 6.Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. February 21 2002;346(8):549–556. [DOI] [PubMed] [Google Scholar]
- 7.Rossetti AO, Oddo M, Logroscino G, Kaplan PW. Prognostication after cardiac arrest and hypothermia: a prospective study. Ann Neurol. March 2010;67(3):301–307. [DOI] [PubMed] [Google Scholar]
- 8.Samaniego EA, Persoon S, Wijman CA. Prognosis after cardiac arrest and hypothermia: a new paradigm. Curr Neurol Neurosci Rep. February 2011;11(1):111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Samaniego EA, Mlynash M, Caulfield AF, Eyngorn I, Wijman CA. Sedation confounds outcome prediction in cardiac arrest survivors treated with hypothermia. Neurocrit Care. August 2011;15(1):113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fugate JE, Wijdicks EF, Mandrekar J, et al. Predictors of neurologic outcome in hypothermia after cardiac arrest. Ann Neurol. December 2010;68(6):907–914. [DOI] [PubMed] [Google Scholar]
- 11.Wilkinson D The self-fulfilling prophecy in intensive care. Theor Med Bioeth. 2009;30(6):401–410. [DOI] [PubMed] [Google Scholar]
- 12.Geocadin RG, Peberdy MA, Lazar RM. Poor survival after cardiac arrest resuscitation: a self-fulfilling prophecy or biologic destiny?*. Crit Care Med. March 2012;40(3):979–980. [DOI] [PubMed] [Google Scholar]
- 13.Schmechel D, Marangos PJ, Zis AP, Brightman M, Goodwin FK. Brain endolases as specific markers of neuronal and glial cells. Science. January 20 1978;199(4326):313–315. [DOI] [PubMed] [Google Scholar]
- 14.Marangos PJ, Schmechel DE. Neuron specific enolase, a clinically useful marker for neurons and neuroendocrine cells. Annu Rev Neurosci. 1987;10:269–295. [DOI] [PubMed] [Google Scholar]
- 15.Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. July 25 2006;67(2):203–210. [DOI] [PubMed] [Google Scholar]
- 16.Zandbergen EG, Hijdra A, Koelman JH, et al. Prediction of poor outcome within the first 3 days of postanoxic coma. Neurology. January 10 2006;66(1):62–68. [DOI] [PubMed] [Google Scholar]
- 17.Tiainen M, Roine RO, Pettila V, Takkunen O. Serum neuron-specific enolase and S-100B protein in cardiac arrest patients treated with hypothermia. Stroke. December 2003;34(12):2881–2886. [DOI] [PubMed] [Google Scholar]
- 18.Pfeifer R, Borner A, Krack A, Sigusch HH, Surber R, Figulla HR. Outcome after cardiac arrest: predictive values and limitations of the neuroproteins neuron-specific enolase and protein S-100 and the Glasgow Coma Scale. Resuscitation. April 2005;65(1):49–55. [DOI] [PubMed] [Google Scholar]
- 19.Rech TH, Vieira SR, Nagel F, Brauner JS, Scalco R. Serum neuron-specific enolase as early predictor of outcome after in-hospital cardiac arrest: a cohort study. Crit Care. 2006;10(5):R133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rundgren M, Karlsson T, Nielsen N, Cronberg T, Johnsson P, Friberg H. Neuron specific enolase and S-100B as predictors of outcome after cardiac arrest and induced hypothermia. Resuscitation. July 2009;80(7):784–789. [DOI] [PubMed] [Google Scholar]
- 21.Shinozaki K, Oda S, Sadahiro T, et al. Serum S-100B is superior to neuron-specific enolase as an early prognostic biomarker for neurological outcome following cardiopulmonary resuscitation. Resuscitation. August 2009;80(8):870–875. [DOI] [PubMed] [Google Scholar]
- 22.Wennervirta JE, Ermes MJ, Tiainen SM, et al. Hypothermia-treated cardiac arrest patients with good neurological outcome differ early in quantitative variables of EEG suppression and epileptiform activity. Crit Care Med. August 2009;37(8):2427–2435. [DOI] [PubMed] [Google Scholar]
- 23.Mlynash M, Buckwalter MS, Okada A, et al. Serum neuron-specific enolase levels from the same patients differ between laboratories: assessment of a prospective post-cardiac arrest cohort. Neurocrit Care. October 2013;19(2):161–166. [DOI] [PubMed] [Google Scholar]
- 24.Oksanen T, Tiainen M, Skrifvars MB, et al. Predictive power of serum NSE and OHCA score regarding 6-month neurologic outcome after out-of-hospital ventricular fibrillation and therapeutic hypothermia. Resuscitation. February 2009;80(2):165–170. [DOI] [PubMed] [Google Scholar]
- 25.Storm C, Nee J, Jorres A, Leithner C, Hasper D, Ploner CJ. Serial measurement of neuron specific enolase improves prognostication in cardiac arrest patients treated with hypothermia: a prospective study. Scand J Trauma Resusc Emerg Med. 2012;20:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huntgeburth M, Adler C, Rosenkranz S, et al. Changes in neuron-specific enolase are more suitable than its absolute serum levels for the prediction of neurologic outcome in hypothermia-treated patients with out-of-hospital cardiac arrest. Neurocrit Care. June 2014;20(3):358–366. [DOI] [PubMed] [Google Scholar]
- 27.Stammet P, Collignon O, Hassager C, et al. Neuron-Specific Enolase as a Predictor of Death or Poor Neurological Outcome After Out-of-Hospital Cardiac Arrest and Targeted Temperature Management at 33 degrees C and 36 degrees C. J Am Coll Cardiol. May 19 2015;65(19):2104–2114. [DOI] [PubMed] [Google Scholar]
- 28.Daubin C, Quentin C, Allouche S, et al. Serum neuron-specific enolase as predictor of outcome in comatose cardiac-arrest survivors: a prospective cohort study. BMC Cardiovasc Disord. 2011;11:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steffen IG, Hasper D, Ploner CJ, et al. Mild therapeutic hypothermia alters neuron specific enolase as an outcome predictor after resuscitation: 97 prospective hypothermia patients compared to 133 historical non-hypothermia patients. Crit Care. 2010;14(2):R69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tong JT, Eyngorn I, Mlynash M, Albers GW, Hirsch KG. Functional Neurologic Outcomes Change Over the First 6 Months After Cardiac Arrest. Crit Care Med. August 5 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ben-Hamouda N, Taccone FS, Rossetti AO, Oddo M. Contemporary approach to neurologic prognostication of coma after cardiac arrest. Chest. November 2014;146(5):1375–1386. [DOI] [PubMed] [Google Scholar]