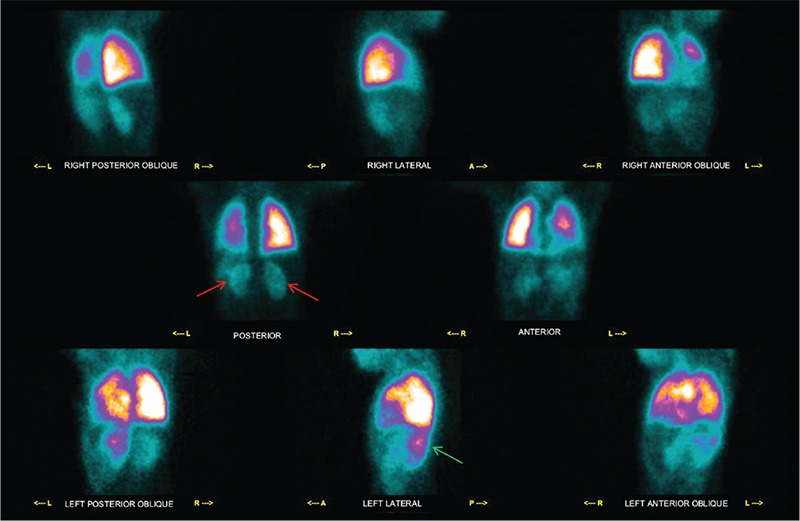
Figure 1. Congenital Heart diseases (CHD), such as tetralogy of fallot (TOF), are the most common human birth anomalies with severity depending on the anatomical defect with subsequent different clinical impact and management (1). CHD may be associated with pulmonary hemodynamic defects so it is important to know lung perfusion status, since its asymmetry is a predictor of exercise capacity and outcome (2). Lung perfusion scintigraphy (LPS) is the gold standard for qualitative and semi-quantitative evaluation of pulmonary perfusion in patients with CHD (3). We report a case of a 10-year-old female patient with cyanotic spells, hypoxia and squatting episodes since birth that progressively increased during the years. A computed tomography angiography performed with a presumptive diagnosis of CHD revealed a cardiac anatomy as in TOF and the patient was admitted to pediatric cardiac surgery clinic according to the European Society of Cardiology guidelines. Her post-operative second year follow-up physical examination revealed clubbing and hypoxia as well as continuous murmur over the chest. Her abdomen was soft with normal bowel sounds and no organ enlargement. The chest X-ray suggested lung inflammatory interstitial disease without focal lesions, pleural effusion or cardiomegaly, her blood work-up revealed Hb: 10.5 gr/dL (normal values 11-13 g/dL), Htc: 36.8% (normal values 35-42%), and fibrinogen protein: 630 mg/dL (normal values 150-400 mg/dL). The patient underwent LPS by intravenous injection of 111 MBq Tc-99m-macroaggregated albumin to evaluate pulmonary hemodynamics and impairment. This figure depicts images of the thorax-abdomen acquired in all the 8 executable planar projections (i.e. right posterior oblique, right lateral, right anterior oblique, posterior, anterior, left posterior oblique, left lateral, left anterior oblique). LPS showed 80% radiopharmaceutical uptake in the lungs and the remnant 20% in the kidneys (red arrows) and spleen (green arrows). This finding supported the presence of a right-to-left shunt, and the patient was kept in close follow-up to be scheduled for further cardiac surgery.