Abstract
Context:
Research has revealed racial disparities in advance care planning and intensity of end-of-life care. Studies of the relationship between advance care planning and sadness and anxiety at the end-of-life are inconclusive.
Objective:
To determine the extent to which the relationship between advance care planning and sadness and anxiety at the end-of-life differs by race.
Methods:
Study analyzes data from 315 Medicare beneficiaries from the 2011–2016 National Health and Aging Trends Study. Caregiver-assessed sadness/anxiety at decedent’s end of life was categorized as none, managed needs, and unmanaged needs. We used multinomial logistic regression and calculated relative risk and predicted probability of reporting sadness/anxiety by race and advance care planning status, controlling for demographic and health characteristics.
Results:
Among non-Hispanic black/African-Americans who died, end-of-life discussions and having a healthcare proxy increased the predicted probability of caregivers reporting unmanaged needs related to sadness/anxiety by factors of 2.6 and 3.5, respectively (discussions: from 15% to 39%, p=.03; healthcare proxy: from 12% to 42% p=.008). In contrast, among non-Hispanic white decedents, end-of-life discussions and naming a healthcare proxy was not associated with caregivers reporting unmanaged needs related to sadness/anxiety.
Conclusion:
Advance care planning may not work the same way for black and white individuals. End-of-life discussions and naming a healthcare proxy are potentially harmful to dying black patients’ mental health. This finding suggests a need for additional research to understand why caregivers report unmanaged sadness/anxiety for dying black patients who engaged in advance care planning, and increased attention to these patients’ mental health at the end-of-life.
Keywords: end-of-life, advance care planning, racial disparities, psychological distress, sadness/anxiety
Introduction
In the case of end-of-life (EoL) care, physicians’ mandate to avoid harming their patients, physically and psychologically,1,2 is not always accomplished,1,3 and is differentially experienced based on patients’ race. Dying patients tend to receive aggressive, burdensome, and potentially futile care, as evidenced by the fact that over 40% of hospitalized patients are admitted to an intensive care unit during their last six months of life.4 This trend is disproportionately borne out among black patients, who consistently receive more aggressive, burdensome, and potentially futile care than white patients.4,5 Advance care planning (ACP) can help reduce aggressive and potentially futile care at EoL6–9 and help patients obtain care that is consistent with their values and preferences.10 However, the benefits of ACP do not apply evenly to black and white patients. Even when ACP is in place, black patients are still at higher risk of aggressive and burdensome care.5
While treatment of physical symptoms at EoL is documented, as are racial disparities in the potentially mitigating effect of ACP, much less is known about mental health of dying patients. Psychological distress is increasingly common among older adults at EoL,11 yet mental health services are underutilized by the Medicare population.12,13 Moreover, although ACP has been shown to help dying patients prepare mentally for death,14,15 the potential for ACP to mitigate psychological distress at EoL is not well understood. Research suggests ACP has no relationship to8,9,16–20 or is associated with a decrease in19,21,22 mental health symptoms among dying patients. However, previous studies tend to focus on a specific disease population, such as patients with cancer or early stage-dementia,9,19,21,22 involve small samples,19–21 or do not account for respondents’ race.8,19–21 We cannot presume the neutral or beneficial effect of ACP on mental health at EoL observed for white patients extends to black patients. Moreover, given documented racial disparities in patterns of EoL care with respect to physical symptoms and potential benefits of ACP in mitigating those symptoms, we need to be aware of and attend to the possibility that similar racial disparities are present with respect to black patients’ psychological distress at EoL.
We know of no studies that explore potential racial differences in the relationship between ACP and sadness/anxiety at EoL. This lack of attention is surprising, given how important mental health is at EoL, documented racial disparities in aggressive and burdensome EoL care, and differential impact of ACP in mitigating disparities in EoL treatments. Seriously ill individuals, bereaved family members, and EoL healthcare providers identify anxiety as an important factor at EoL.14 Studies of EoL care quality ask respondents about sadness and anxiety as indicators of psychological distress.23 This study uses longitudinal, population-based survey data to answer the question: Do the effects of ACP on caregiver reports of dying individuals’ sadness and anxiety differ by their race?
Methods
Study Sample
Data are from six rounds of the National Health and Aging Trends Study (NHATS), a longitudinal population-based survey of older adults. The NHATS is comprised of a random sample of 8,245 noninstitutionalized Medicare enrollees age 65 and over in the contiguous United States in 2011 and oversampled black persons and those age 90 and older. Others have described sampling and weighting strategies in detail.24,25 This analysis includes 315 participants who: 1) were randomly selected to answer the EoL plans and care module in round two (2012), 2) died in rounds three to six (2013–2016), 3) identified as black or white, and 4) had no missing values on outcome or predictor measures. The Johns Hopkins Institutional Review Board approved the protocol for the NHATS data collection. The Weill Cornell Medicine Institutional Review Board deemed this study exempt from needing approval and informed patient consent.
Measures
EoL sadness/anxiety was measured by survey responses from individuals familiar with the decedent’s EoL care, most often a family member (“caregivers”). Caregivers answered questions about whether the decedent experienced sadness/anxiety in their last month of life, whether they received help for their sadness/anxiety, and whether it was the right amount if help. These questions are validated elsewhere23 and were part of the Family Evaluation of Hospice Care survey.26 Our resulting outcome measure had three categories for decedent sadness/anxiety: none, managed and unmanaged.
The NHATS decedents self-reported their race and ACP completion in survey waves prior to their deaths. We limited the analysis to black and white decedents and used three measures of ACP: end-of-life discussions, healthcare proxy (HCP), and living will. Our analyses also adjusted for self-reported decedent demographic, health, and death data linked to sadness/anxiety, race, and/or ACP: sex,27,28 education,29,30 age,31 importance of attending religious services,32,33 number of serious diagnoses34 that are also leading causes of death among older adults (heart disease, cancer, diabetes, stroke, lung problems, dementia),35 number of recent hospitalizations,36 home death,37 and hospice involvement in the last month of life.9 We control for these variables because previous research shows they have been linked higher rates of mood disorders such as anxiety and depression and poorer mental health9,27,28,33,34,36, race,30,31 and/or ACP completion.9,29,32,37
Statistical Analysis
We applied analytic survey weights to adjust for differences in nonresponse based on respondent race and age and county and census-level tract data.25 Descriptive statistics reflect national estimates for the overall sample analyzed, as well as for black and white respondents (Table 1). We calculated multinomial logistic regression models for each type of ACP (discussions, HCP, living will) to determine the relationship between race, ACP, and the interaction of race and ACP on caregiver assessments of the decedent’s sadness/anxiety at EoL (to test moderation effects), after controlling for the decedent demographic and health characteristics listed in the previous paragraph. We used analytic survey weights to adjust all analyses for complex survey design. All analyses were conducted using statistical software (STATA, version MP15; StataCorp LP).
Table 1.
Weighted descriptive statistics for NHATS respondents representing 1,126,644 Medicare enrollees age 65 and older (unweighted n=315)
| All respondents | Non-Hispanic white | Non-Hispanic black / African-American | P valuea | ||||
|---|---|---|---|---|---|---|---|
| Proportion or means | Proportion or means | Proportion or means | |||||
| (SD) | LSE | (SD) | LSE | (SD) | LSE | ||
| Outcomes (last month of life) | |||||||
| Sadness/Anxiety | 0.22 | ||||||
| Unmanaged needs | 0.27 | 0.030 | 0.27 | 0.034 | 0.27 | 0.052 | |
| Managed needs | 0.38 | 0.031 | 0.39 | 0.035 | 0.27 | 0.063 | |
| None | 0.36 | 0.029 | 0.35 | 0.033 | 0.46 | 0.058 | |
| Predictors | |||||||
| Non-Hispanic white | 0.90 | 0.013 | |||||
| EOL discussions | 0.66 | 0.029 | 0.691 | 0.035 | 0.398 | 0.052 | 0.0002 |
| Health care proxy | 0.65 | 0.030 | 0.672 | 0.034 | 0.442 | 0.049 | 0.0005 |
| Living will | 0.64 | 0.030 | 0.679 | 0.035 | 0.339 | 0.042 | 0.000 |
| Covariates | |||||||
| Male | 0.44 | 0.034 | 0.43 | 0.038 | 0.46 | 0.065 | 0.77 |
| More than high school education | 0.48 | 0.035 | 0.49 | 0.0391 | 0.35 | 0.0587 | 0.055 |
| Agec | 4.13 (0.09) | 0.09 | 4.19 (1.27) | 0.095 | 3.63 (2.15) | 0.176 | 0.005b |
| 65–69 | 0.01 | 0.009 | 0.01 | 0.010 | 0.02 | 0.022 | 0.068 |
| 70–74 | 0.14 | 0.027 | 0.13 | 0.028 | 0.26 | 0.058 | |
| 75–79 | 0.19 | 0.032 | 0.19 | 0.034 | 0.18 | 0.044 | |
| 80–84 | 0.21 | 0.030 | 0.20 | 0.034 | 0.29 | 0.039 | |
| 85–89 | 0.22 | 0.032 | 0.23 | 0.034 | 0.14 | 0.037 | |
| 90+ | 0.22 | 0.026 | 0.23 | 0.029 | 0.12 | 0.030 | |
| Religious attendance very important | 0.41 | 0.035 | 0.39 | 0.038 | 0.54 | 0.060 | 0.029 |
| Number of serious diagnosesd | 1.98 (0.10) | 0.10 | 1.97 (1.08) | 0.106 | 2.10 (1.90) | 0.127 | 0.41b |
| 0 | 0.09 | 0.017 | 0.09 | 0.019 | 0.12 | 0.031 | 0.0797 |
| 1 | 0.28 | 0.035 | 0.29 | 0.038 | 0.20 | 0.042 | |
| 2 | 0.33 | 0.033 | 0.34 | 0.037 | 0.28 | 0.059 | |
| 3 | 0.14 | 0.027 | 0.13 | 0.030 | 0.27 | 0.059 | |
| 4+ | 0.15 | 0.024 | 0.15 | 0.027 | 0.13 | 0.036 | |
| 0 or 1 hospital stay in year before death (ref=2 or more stays) | 0.79 | 0.027 | 0.80 | 0.030 | 0.70 | 0.043 | 0.047 |
| Home death | 0.40 | 0.039 | 0.40 | 0.043 | 0.35 | 0.051 | 0.43 |
| Hospice involved in last month of life | 0.58 | 0.041 | 0.58 | 0.045 | 0.54 | 0.050 | 0.54 |
NHATS, National Health and Aging Trends Study; SD, standard deviation; LSE, linearized standard error. Analysis pools data from 2011–2016 annual surveys. Estimates adjusted for complex survey design to reflect population of 2011 Medicare enrollees over 65. Estimates based on sample size of 315 NATS respondents who answered the 2012 module on end-of-life planning, subsequently died (2013–2016), for whom a caregiver answered questions about sadness/anxiety in the last month of life, and who are not missing on any other covariates.
Except where noted, p value comparing white and black is based on Pearson’s chi square calculated from F statistic adjusted for complex survey design.
p value based on adjusted Wald test of difference of means.
Average ages for each group are: sample=80–84, white=80–84, black=75–79
Diagnoses: heart disease, diabetes, stroke, lung problems, kidney problems, and probable dementia.
Results
Table 1 provides weighted descriptive statistics for the analyzed sample (n=315), which represents 1,126,644 black and white Medicare recipients age 65 and older. Of these, 89.7% were white, 43.7% male, and 47.6% had more than a high school education. On average, decedents were 80–84 years old when they died, although white decedents were significantly older than black decedents at death (white: 80–84 years old; black: 75–79 years old). Caregivers reported no, managed needs, or unmanaged needs related to decedents’ sadness/anxiety in relatively equal proportions (35.8%, 37.6%, and 26.6%, respectively), and there were no differences between reports for black and white decedents (p=.22). White decedents were more likely than black decedents to have reported having EoL discussions (69.1% vs 39.8%, p=.0002), HCPs (67.2% vs 44.2%, p=.0006), and living wills (67.9% vs 33.9% (p=.0000).38
Multinomial logistic regression models adjusted for decedent sociodemographic, health, and death information found that when black decedents reported EOL discussions or naming an HCP, caregivers were more likely to report the dying individual experienced unmanaged needs related to sadness or anxiety at EOL than if no ACP were reported. There was no relationship between ACP and sadness or anxiety for white decedents or for living wills for either race (Table 2). For EoL discussions, interaction and main effects were significant for none versus unmanaged needs related to sadness/anxiety (race: ARR=0.20, 95% CI: 0.06–0.64; discussions: ARR=0.19, 95% CI: 0.06–0.61; race* discussion: ARR=9.37, 95% CI: 2.64–33.26). Similar patterns were observed for HCPs (race: ARR=0.24, 95% CI: 0.07–0.80; HCP: ARR=0.14, 95% CI: 0.04–0.52, race* HCP: ARR=6.42, 95% CI: 1.33–33.10). Interaction, but not main effects were significant for met versus unmanaged needs related to sadness/anxiety (race*discussion: ARR=5.19, 95% CI: 1.21–22.28; race*HCP: ARR=7.96, 95% CI: 1.19–53.14). Main and interaction effects were not significant for living wills.
Table 2.
Adjusted risk ratios and 95% confidence intervals for multinomial logistic regression of caregiver reported sadness or anxiety in NHATS decedent’s last month of life for three types of advance care planning
| Unmanaged needs (reference) | Unmanaged needs vs Managed needs | Unmanaged needs vs None | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ARR | ARR | 95% CI | p value | ARR | 95% CI | p value | |||
| End-of-Life Discussions | |||||||||
| White | 1.00 | 0.55 | 0.17 | 1.83 | 0.32 | 0.20 | 0.06 | 0.64 | 0.01 |
| Discussions | 1.00 | 0.38 | 0.10 | 1.39 | 0.14 | 0.19 | 0.06 | 0.61 | 0.01 |
| White * discussions | 1.00 | 5.19 | 1.21 | 22.28 | 0.03 | 9.37 | 2.64 | 33.26 | 0.00 |
| Health Care Proxy | |||||||||
| White | 1.00 | 0.43 | 0.09 | 1.96 | 0.27 | 0.24 | 0.07 | 0.80 | 0.02 |
| Health care proxy | 1.00 | 0.19 | 0.03 | 1.13 | 0.07 | 0.14 | 0.04 | 0.52 | 0.00 |
| White * health care proxy | 1.00 | 7.96 | 1.19 | 53.14 | 0.03 | 6.42 | 1.33 | 31.10 | 0.02 |
| Living Will | |||||||||
| White | 1.00 | 1.62 | 0.53 | 5.00 | 0.39 | 0.45 | 0.14 | 1.52 | 0.19 |
| Living will | 1.00 | 1.54 | 0.51 | 4.67 | 0.43 | 0.78 | 0.20 | 3.02 | 0.72 |
| White * living will | 1.00 | 0.66 | 0.16 | 2.70 | 0.56 | 1.79 | 0.32 | 10.03 | 0.50 |
NHATS, National Health and Aging Trends Study; ARR, adjusted risk ratio; 95% CI, 95% confidence interval; ACP, advance care planning. Analysis pools data from 2011–2016 annual surveys. Models adjust for decedent sex, education, age, religiosity, number of serious diagnoses, number of recent hospitalizations, home death, and hospice involvement at end of life. Estimates adjusted for complex survey design to reflect population of 2011 Medicare enrollees over 65.
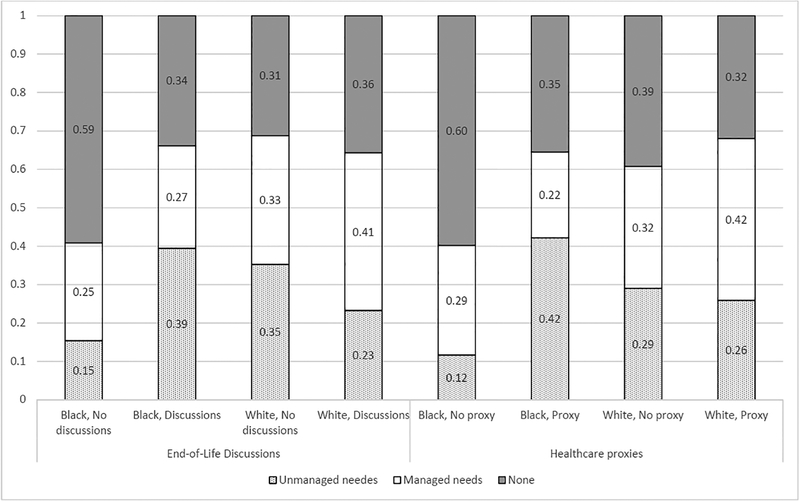
Because interpreting coefficients and relative risk ratios for main and interaction effects in multinomial logistic regression models is cumbersome and unintuitive, we calculated predicted probabilities of none, managed needs, and unmanaged needs related to sadness/anxiety at EoL by decedent race and ACP completion, holding all other variables at their means. Figure 1 graphs predicted probabilities for EoL discussions and HCPs for four groups: black decedents with no ACP, black decedents with ACP, white decedents with no ACP, and white decedents with ACP. We excluded living wills because there were no significant differences by race and ACP in that analysis.
Figure 1. Predicted probabilities of sadness/anxiety at end of life by race and advance care planning.
Data pooled from 2011–2016 National Health and Aging Trends Study. Estimates adjusted for complex survey design to reflect population of 2011 Medicare enrollees over 65 and for covariates listed in Table 1. All covariates held at their means.
Three patterns emerge from the data. First, as reported by caregivers, black decedents with no ACP had the highest predicted probability of no sadness/anxiety at EoL of any group, and in some cases, nearly double that for other groups. For example, black decedents with no ACP had a 59% predicted probability of no sadness/anxiety at EoL compared to 31% for white decedents with no ACP. Second, among black decedents, EoL discussions and having a HCP increase the predicted probability of unmanaged needs related to sadness/anxiety by factors of 2.6 and 3.5, respectively (discussions: from 15% to 39%, p=.03; healthcare proxy: from 12% to 42% p=.008). In contrast, there was no relationship between ACP and unmanaged needs related to sadness/anxiety among white decedents (discussions: from 35% to 23%, p=.08; healthcare proxy: from 29% to 26% p=.66). Third, predicted probabilities of caregivers reporting decedents’ needs related to sadness/anxiety at EoL were met are relatively similar across groups.
Discussion
We found that black decedents who complete ACP were more likely to have unaddressed mental health needs than those who did not complete ACP. This result held only for black decedents: there was no relationship between ACP completion and caregiver reported anxiety or sadness among white decedents. Consistent with previous research,8,9,16,19,20 we found no significant relationship between ACP and sadness/anxiety at EoL for white decedents. In contrast, we find that EoL discussions and having a HCP are associated with negative outcomes for black decedents, reducing the predicted probability of no caregiver reported sadness/anxiety by over 40%, while increasing the predicted probability of unmanaged needs related to sadness/anxiety by a factor of 2.6 and 3.5, respectively. Moreover, results suggested that completing ACP resulted in black decedents not having any sadness/anxiety at EoL to experiencing sadness/anxiety and not receiving adequate help with those symptoms.
One possible explanation for the observed differences in unmanaged needs related to sadness/anxiety among black decedents could be that there is something psychosocially distinctive about black individuals who complete ACP that leads to psychological distress at EoL. However, supplementary analyses do not support this explanation in these data. Supplementary analyses indicate these patterns persist regardless of decedent education, religiosity, and recent hospitalizations (which were all significant in adjusted multinomial logistic regression models). Nor was the difference attributable to higher levels of depression and anxiety among black decedents who complete ACP, as black decedents had reported similar levels of depression and anxiety in the survey interview prior to their deaths regardless of whether they completed ACP and as white decedents.
The difference in caregiver assessments of black decedents’ psychological distress at EoL based on ACP completion may be the result of something about the ACP process for black individuals that leads to distress at EoL, underscoring the need for culturally sensitive, tailored approaches to ACP and EoL care1,39 that focus on building rapport with black patients. The difference in assessments may also be attributed to something that happens through the course of EoL care to black patients who complete ACP. Consistent with the original intent of ACP, black patients desiring less aggressive care may complete ACP, but still receive aggressive care at EoL,7 resulting in increased psychological distress. Although these data do not track actual treatment received, supplementary analyses do not support this idea. Rather, in these data, caregivers report black decedents received unwanted care at similar, low rates, regardless of ACP completion and as white decedents. In contrast, black patients may desire more aggressive care at EoL1,40 and complete ACP to that effect. Failing to receive care consistent with their preferences may cause increased psychological distress. These data do not allow us to examine the content of ACP or whether individuals failed to receive treatment they would have wanted. In either scenario, psychological distress at EoL is more probable and not addressed adequately for black individuals who complete ACP.
Additional research is needed to understand why caregivers for black decedents who complete ACP are predicted to report unmanaged needs related to sadness/anxiety, and at such higher levels than black decedents who do not complete ACP. This study also suggests a need for ACP completion processes tailored to the needs of older black individuals. Clinicians should be particularly attentive at EoL to the psychological well-being and needs of their black patients who report completing ACP, perhaps by working with caregivers to detect, determine the sources of, and address psychological distress.
While the patterns described above are consistent for EoL discussions and HCPs, we found no differences based on completion of a living will. This could be due to a lack of statistical power, given that only 27 black decedents in the unweighted sample had previously reported a living will. However, there may be greater barriers associated with completing a living will compared to discussing EoL or naming a HCP.41
This study has limitations. The data focus on Medicare enrollees over 65, and different relationships between race, ACP and sadness/anxiety at EoL may exist among younger or middle-aged adults or among older adults who do not receive Medicare. However, adults over 65 comprise nearly three-quarters of all annual deaths in the US,31 and Medicare coverage extends to 93% of these,42 so understanding patterns among these individuals is important. This study is a secondary analysis of existing data, and so we relied on measures that were available in the data. We are not able to use assessments of sadness or anxiety at EOL obtained directly from the NHATS respondent. However, all other measures were obtained prospectively, and obtaining information about EoL retrospectively from individuals familiar with care is a recognized43,44 and commonly used mechanism11,45,46 in EoL research, particularly given the ethical considerations of collecting direct reports from dying individuals in their final month.44 Moreover, doing so is not feasible in a study of this scale and for which the study design allows for data collection only during certain months of the year.
Conclusion
Advance care planning may not work the same way for black and white individuals. Namely, ACP is associated with increased risk of negative mental health outcomes at EoL for black individuals, but not for white individuals. Our findings underscore an urgent need for additional research to understand why caregivers report unmanaged sadness/anxiety for dying black patients who completed advance care planning, so that we can better understand why a tool intended to improve EoL care is associated with increased and unaddressed distress among older black adults. Our findings also highlight a need for clinicians to pay increased attention to and work with caregivers to address these patients’ mental health as life draws to a close.
Acknowledgements
This research was supported in part by the National Institute on Aging (T32AG049666) (EAL) and the National Cancer Institute (CA197730) (HGP).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
Dr. Luth has nothing to disclose.
Dr. Prigerson has nothing to disclose.
References
- 1.Institute of Medicine. Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, DC: The National Academies Press;2014. [PubMed] [Google Scholar]
- 2.National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care, Third Edition. Pittsburgh, PA: 2013. [Google Scholar]
- 3.Solano JP, Gomes B, Higginson IJ. A Comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Sympt Manage 2006;31(1):58–69. [DOI] [PubMed] [Google Scholar]
- 4.Dartmouht Atlas of Healthcare. Percent of medicare decedents hospitalized at least once during the last six months of life, by race and level of care intensity. National Average, 1996–2014. 2018. http://www.dartmouthatlas.org/. Accessed June 6, 2018.
- 5.Loggers ET, Maciejewski PK, Paulk E, et al. Racial differences in predictors of intensive end-of-life care in patients with advanced cancer. J Clin Oncol 2009;27(33):5559–5564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nicholas L, Langa KM, Iwashyna TJ, Weir DR. Regional variation in the association between advance directives and end-of-life medicare expenditures. JAMA 2011;306(13):1447–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mack JW, Paulk M, Viswanath K, Prigerson HG. Racial disparities in the outcomes of communication on medical care received near death. Arch Intern Med 2010;170(17):1533–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: A national study. J Am Geriatr Soc 2007;55(2):189–194. [DOI] [PubMed] [Google Scholar]
- 9.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008;300(14):1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010;340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teno JM, Freedman VA, Kasper JD, Gozalo P, Mor V. Is care for the dying improving in the United States? J Palliat Med 2015;18(8):662–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bartels SJ, Naslund JA. The underside of the silver tsunami — Older adults and mental health care. New Eng J Med. 2013;368(6):493–496. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine. The mental health and substance use workforce for older adults: In whose hands? Washington, DC: The National Academmies Press;2012. [PubMed] [Google Scholar]
- 14.Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 2000;284(10):2476–2481. [DOI] [PubMed] [Google Scholar]
- 15.Martin DK, Thiel EC, Singer PA. A new model of advance care planning: Observations from people with HIV. Arch Intern Med 1999;159(1):86–92. [DOI] [PubMed] [Google Scholar]
- 16.Houben CHM, Spruit MA, Groenen MTJ, Wouters EFM, Janssen DJA. Efficacy of advance care planning: A systematic review and meta-analysis. J Am Med Dir Assn 2014;15(7):477–489. [DOI] [PubMed] [Google Scholar]
- 17.Schneiderman LJ, Kronick R, Kaplan RM, Anderson JP, Langer RD. Effects of offering advance directives on medical treatments and costs. Annals Intern Med 1992;117(7):599–606. [DOI] [PubMed] [Google Scholar]
- 18.Vandervoort A, van den Block L, van der Steen JT, Vander Stichele R, Bilsen J, Deliens L. Advance directives and physicians’ orders in nursing home residents with dementia in Flanders, Belgium: prevalence and associated outcomes. Internat Psychogeriatr 2012;24(7):1133–1143. [DOI] [PubMed] [Google Scholar]
- 19.Pautex S, Herrmann F, Zulian G. Role of advance directives in palliative care units: a prospective study. Palliat Med 2008;22(7):835–841. [DOI] [PubMed] [Google Scholar]
- 20.Jones L, Harrington J, Barlow CA, et al. Advance care planning in advanced cancer: Can it be achieved? An exploratory randomized patient preference trial of a care planning discussion. Palliat Support Care 2011;9(1):3–13. [DOI] [PubMed] [Google Scholar]
- 21.Hilgeman MM, Allen RS, Snow AL, Durkin DW, DeCoster J, Burgio L. Preserving Identity and Planning for Advance Care (PIPAC): preliminary outcomes from a patient-centered intervention for individuals with mild dementia. Aging & Mental Health 2014;18(4):411–424. [DOI] [PubMed] [Google Scholar]
- 22.Mack JW, Weeks JC, Wright AA, Block SD, Prigerson HG. End-of-life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. J Clinic Oncol 2010;28(7):1203–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Teno JM, Clarridge B, Casey V, Edgman-Levitan S, Fowler J. Validation of toolkit after-death bereaved family member interview. J Pain Sympt Manage 2001;22(3):752–758. [DOI] [PubMed] [Google Scholar]
- 24.Montaquila J, Freedman VA, Edwards B, Kasper JD. National Health and Aging Trends Study Round 1 Sample Design and Selection. NHATS Technical Paper #1. Baltimore: 2012. [Google Scholar]
- 25.DeMatteis JM, Freedman VA, Kasper JD. National Health and Aging Trends Study Development of Round 6 Survey Weights. NHATS Technical Paper #18. Baltimore: 2017. [Google Scholar]
- 26.Connor SR, Teno J, Spence C, Smith N. Family evaluation of hospice care: Results from voluntary submission of data via website. J Pain Sympt Manage. 2005;30(1):9–17. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC. Gender differences in the prevalence and correlates of mood disorders in the general population. Mood disorders in women. 2000:15–33. [Google Scholar]
- 28.Kessler RC. Epidemiology of women and depression. J Affective Disorders. 2003;74(1):5–13. [DOI] [PubMed] [Google Scholar]
- 29.Carr D The social stratification of older adults’ preparations for end-of-life health care. J Health Soc Behav. 2012;53(3):297–312. [DOI] [PubMed] [Google Scholar]
- 30.Shapiro TM. The Hidden Cost of Being African American: How Wealth Perpetuates Inequality. Oxford: Oxford University Press; 2005. [Google Scholar]
- 31.Murphy S, Xu J, Kochanek K, Curtin S, Arias E. Deaths: Final data for 2015. Hyatsville, MD: 2017. [PubMed] [Google Scholar]
- 32.Garrido MM, Idler EL, Leventhal H, Carr D. Pathways from religion to advance care planning: beliefs about control over length of life and end-of-life values. Gerontolog 2013;53(5):801–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Balboni TA, Balboni M, Enzinger AC, et al. Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Intern Med 2013;173(12):1109–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Evans DL, Charney DS, Lewis L, et al. Mood disorders in the medically ill: Scientific review and recommendations. Biolog Psyc 2005;58(3):175–189. [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control National Center for Health Statistics. Underlying Causes of Death, 1999–2016 on CDC WONDER Online Database. In: Centers for Disease Control National Center for Health Statistics, 2017. [Google Scholar]
- 36.Ciro CA, Ottenbacher KJ, Graham JE, Fisher S, Berges I, Ostir GV. Patterns and correlates of depression in hospitalized older adults. Arch Gerontol Geriatric 2012;54(1):202–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Degenholtz HB, Rhee Y, Arnold RM. Brief communication: The relationship between having a living will and dying in place. Annals Intern Med 2004;141(2):113–117. [DOI] [PubMed] [Google Scholar]
- 38.Carr D Racial differences in end-of-life planning: Why don’t Blacks and Latinos prepare for the inevitable? Omega: J Death Dying 2011;63(1):1–20. [DOI] [PubMed] [Google Scholar]
- 39.Ferrell B, Connor SR, Cordes A, et al. The National Agenda for Quality Palliative Care: The National Consensus Project and the National Quality Forum. J Pain Sympt Manage 2007;33(6):737–744. [DOI] [PubMed] [Google Scholar]
- 40.Degenholtz HB, Thomas SB, Miller MJ. Race and the intensive care unit: disparities and preferences for end-of-life care. Crit Care Med 2003;31(5):S373–S378. [DOI] [PubMed] [Google Scholar]
- 41.Carr DS, Luth EA. End-of-life planning and health care In: George LK, Ferraro KF, eds. Handbook of Aging and the Social Sciences, 8th Edition London: Elsevier; 2016:375–396. [Google Scholar]
- 42.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2010. Washington, D.C.2011. [Google Scholar]
- 43.Teno JM. Measuring end-of-life care outcomes retrospectively J Palliat Med 2005;8(Supp 1):S42–S49. [DOI] [PubMed] [Google Scholar]
- 44.George LK. Research design in end-of-life research. Gerontolog 2002;42(Supplement 3):86–98. [DOI] [PubMed] [Google Scholar]
- 45.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA 2004;291(1):88-93-88-93. [DOI] [PubMed] [Google Scholar]
- 46.Teno JM, Mor V, Ward N, et al. Bereaved family member perceptions of quality of end-of-life care in U.S. regions with high and low usage of intensive care unit care. J Am Geriatr Soc 2005;53(11):1905–1911. [DOI] [PubMed] [Google Scholar]