Introduction
In the United States, 23.4 million adults have physician‐diagnosed diabetes mellitus (DM),1 81.6 million have prediabetes, and ≈18 000 people under age 20 years are diagnosed with type 1 DM each year.2 Approximately 90% to 95% of all adult DM cases are type 2.2 As such, data mentioned throughout will primarily comprise patients with type 2 DM. Patients with DM are 2 to 4 times more likely to die of cardiovascular disease (CVD) than patients without DM. The prevalence of patients living with DM and prediabetes continues to increase, putting these individuals at greater risk of having a heart attack or stroke. Often patients with DM have multiple other health problems and must also manage other cardiometabolic health risk factors such as obesity, hypertension, and high cholesterol.
Because of the direct impact DM and related cardiometabolic disorders have on CVD, the American Heart Association (AHA) is building a multifaceted initiative to (1) unite the primary care, cardiology, endocrinology, and other specialty care provider communities in a comprehensive approach to caring for and treating patients with cardiometabolic conditions such as DM; (2) educate and empower people living with cardiometabolic disorders and DM to better self‐manage their condition(s) and improve their cardiovascular health.
By expanding AHA's efforts to include initiatives and programs to reduce the prevalence and impact of cardiometabolic risk factors (such as prediabetes) and conditions (such as DM), the AHA will progress toward its mission of building healthier lives, free of cardiovascular diseases and stroke.
To launch this new initiative, AHA held its first Cardiometabolic Health and Diabetes Summit on December 5, 2017, in Dallas, Texas. The objective was to identify and prioritize opportunities to improve cardiometabolic health and DM care in the United States (Figure 1).
Figure 1.
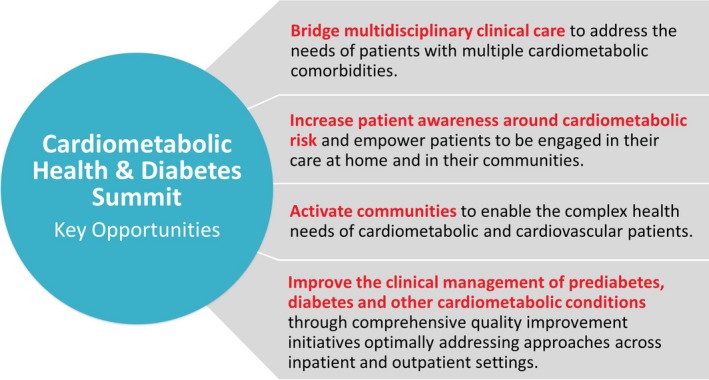
American Heart Association Summit key opportunities.
The AHA is a leader in developing quality clinical care programs; cardiovascular population‐based health programs; and public awareness, education, and empowerment campaigns that focus on undertreated populations. The AHA brought together experts from leading US healthcare, patient, professional, government, and public organizations to discuss a comprehensive approach for reducing cardiometabolic risk and improving comprehensive DM care. Twenty‐one organizations were represented by more than 100 attendees.
Summit structure
The Summit format included keynote speakers from the Centers for Disease Control and Prevention (CDC) and the National Hispanic Medical Association. Subject matter experts participated in panel discussions focusing on healthcare systems and quality improvement; patient and community awareness and empowerment; and leveraging technology to advance patient care. Presenters addressed these issues from the perspective of the clinician, patient, community, and public health. Small‐group breakout sessions generated a priority list of activities addressing gaps and needs for the AHA and its collaborators to address over the short and long term. Many participants and organizations provided poster presentations and breakouts to inform current research and programs. To end the summit, participants further narrowed recommended solutions through an electronic voting process considering impact, effort, and resources needed.
Opening Address by AHA's Chief Executive Officer
Nancy Brown, the AHA's Chief Executive Officer, started the summit by describing the AHA's engagement in DM care. She emphasized the importance of addressing cardiometabolic health and DM in advancing the AHA 2020 Health Impact Goal of improving the cardiovascular health of all Americans. Eduardo Sanchez, MD, MPH, the AHA's Chief Medical Officer for Prevention, further detailed the increasing prevalence of hypertension, DM, prediabetes, and cholesterol in the United States, as well as the increasing percentage of patients who have 2 or more of these conditions. Recognizing this increasing impact, AHA leadership framed the importance of a comprehensive approach to the treatment and management of patients with DM and prediabetes to optimize cardiometabolic risk factors, and ultimately lower cardiovascular risk. Figure 2 is adapted to illustrate the interplay between what the AHA calls “Life's Simple 7” and cardiometabolic risk factors that affect a person's likelihood of developing CVD.3 (Life's Simple 7 is the name for the factors and behaviors proven to build toward ideal cardiovascular health: stop smoking, eat better, get active, maintain a healthy weight, manage blood pressure, control cholesterol, and control blood glucose).
Figure 2.
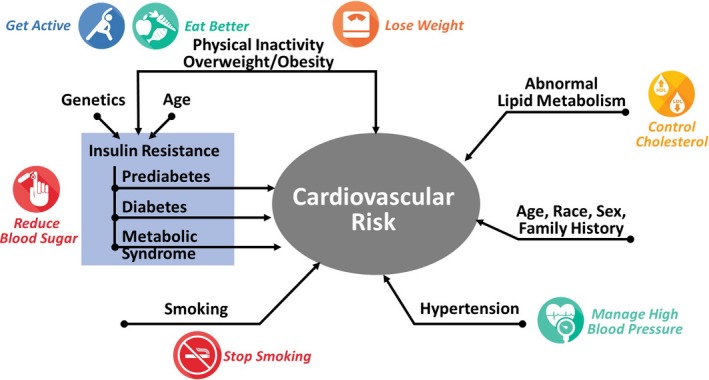
Contributions of Life's Simple 7 health behaviors and factors to cardiometabolic risk. Reprinted from Brunzell et al3 with permission. Copyright ©2008, Elsevier.
Plenary Session Summary: Addressing US Health Disparities in DM Care
The CDC has been at the forefront of evidence‐based interventions for the US healthcare and public health systems to help reduce the incidence and complications of DM and CVD. Almost 40% of all Americans have obesity, which translates to ≈1.5 million new cases of DM each year.1 The annual medical cost of obesity was estimated to be $147 billion in 2008 in the United States. There are dramatic disparities in the prevalence of DM across racial and ethnic groups. DM prevalence is highest among American Indians, Alaska Natives, Hispanics, and non‐Hispanic blacks. In contrast, Asian and white non‐Hispanic prevalence rates are 50% lower than those for other racial and ethnic groups. The CDC's approach focuses on health equity, lifestyle change, scaling up effective programs to increase access, working with advocacy partners, and using a systems‐based approach.
The CDC's Diabetes strategic plan for 2017–2021 includes 3 major goals and the corresponding strategies for each goal:
-
GOAL 1: Prevent type 2 DM
Conduct surveillance and research of DM and sharing with key stakeholders.
Raise awareness of prediabetes.
Conduct applied research and execute a translation agenda to disseminate findings.
Scale and support the National Diabetes Prevention Program (DPP). The DPP intervention is a yearlong program that includes a lifestyle coach, group support, and DM education. This evidence‐based program has been successful in reducing the risk of developing DM by 58%, and is even more effective in older populations (>60 years old), reducing the risk of DM by 71%.4 A key strategy is to continue to recruit and enroll people into this program, and to work through insurers to increase coverage and reimbursement.
-
GOAL 2: Prevent complications through improved approaches to care
Conduct surveillance and effectiveness research on DM care to share with stakeholders.
Support the expansion and implementation of the Diabetes Self‐Care Management Education and Support. The Diabetes Self‐Care Management Education and Support program is designed to help prevent complications from DM by teaching participants how to manage medications, improve nutrition, and increase physical activity. Only a small number of patients have access to this program.
Conduct applied research and execute a translation agenda to disseminate findings.
-
GOAL 3: Reduce differences in health that impact people affected by DM
Conduct disparities‐focused surveillance and research.
Targeted implementation of core DM prevention and management programs.
Dr Samuel Arce, from the National Hispanic Medical Association, discussed what was and was not working in the detection and management of cardiometabolic diseases and DM across the population. As the demographics change in the United States, it is projected that by 2050 nearly 25% of the population will be Hispanic. A 2006 estimate from the CDC projects that 1 in 3 Americans will have DM by 2050, including 1 in 3 African‐Americans and 1 in 2 Hispanic Americans.5 The vast majority of DM care is overseen by primary care physicians who may also be treating these patients for high cholesterol, hypertension, and other chronic conditions.6 There are also many community risk factors for developing these cardiometabolic conditions, such as poor diet, physical inactivity, excessive alcohol use, smoking, lower socioeconomic status, access to nutritious foods, and education level. Some of the biggest barriers to managing these disease conditions are age; genetics; cultural bias (on the part of both patient and provider); social determinants and environmental factors; lack of access to healthy options; improperly addressed prediabetes; access to quality health care; cost of medicine; and the need for major lifestyle changes. Factors shown to reduce the risk of developing these diseases are smoking cessation, cultural competency training, increasing education, affordable health care, and lifestyle changes.
As demographics change in the United States, the population is projected to be 29% Hispanic by 2060.7 Thus, future public health professionals will need to place a larger emphasis on primary and secondary prevention through culturally sensitive approaches. For example, they should emphasize the DASH diet and the AHA Recommended Dietary Guidelines without dismissing traditional foods. Healthcare providers must overcome stereotypes about populations while also encouraging intake of fresh vegetables, whole grains, lean poultry, fish, and fruit. Health professionals will also need to focus on improving access to health care—again while addressing stereotypes. Strategies include engaging primary care providers, addressing physiological and social factors, improving access to quality care, addressing social determinants of health, making small changes, and meeting people “where they are.”
Key Factors and Potential Strategies to Improve DM Diagnosis, Treatment, and Management
From the panel presentations and small‐group breakout discussions, potential factors and key strategies to improve DM diagnosis, treatment, and management were further identified and summarized (Table 1). Each breakout session also focused on a series of solutions to address potential barriers.
Table 1.
Key Factors and Potential Strategies Identified in the Diabetes Summit
| Key Factors | Strategies Proposed and Prioritized |
|---|---|
| Community | Support public education and awareness campaigns to help patients understand the links between prediabetes, diabetes mellitus, cardiometabolic risk factors, and CVD |
| Meet people where they live, work, and worship | |
| Support community/clinical partnerships with integration of services/data | |
| Social determinants of health | Address barriers to access to care and access to healthy, affordable food |
| Improve walkability and transportation to and from appointments | |
| Facilitate community involvement, and work together to address issues related to low income, educational attainment, literacy rates, and access to information | |
| Healthcare team | Need to simplify (and better systematize) the approach to caring for patients with cardiometabolic risk factors and diabetes mellitus |
| Identify ways to provide cultural competency training to providers | |
| Work with professional associations to create easier‐to‐implement care plans for patients | |
| Use a multidisciplinary approach to patient care and provide tools to support the collaboration | |
| Better education for providers on how to motivate behavior change in patients | |
| Develop culturally and linguistically sensitive programming and tools | |
| Family/youth | Must be involved in the diagnosis, treatment, management, and prevention of diabetes mellitus |
| Youth‐based programming in schools may be an important way to reach families | |
| Successful interventions for behavior change must include the family | |
| Advocacy and payers | Need to advocate at state and national levels for policies to improve social determinants of health |
| Pay for programs that have been shown to work (eg, DPP, DSMES) | |
| Systems of care | Better integrate inpatient, outpatient, and community‐based settings where patients may receive care |
| Identify and disseminate best practices from other quality improvement programs that have been shown to improve care for these populations | |
| Embed tools and resources within electronic health records or explore other ways to help providers collaborate and discuss care with patients | |
| Research | Support more studies to understand use of medications in patients with prediabetes |
| Provide clearer guidance of how, when, and why to use newer medications to decrease cardiovascular risk in patients with diabetes mellitus | |
| Better understand the role of genetics, race, ethnicity, and sex in cardiometabolic risk | |
| Standardize definitions in screening/diagnosis for prediabetes, diabetes mellitus, and cardiometabolic risk | |
| Technology | Standardize how mobile health application tools are created, certified for content, and integrated into systems of care |
| Support expanded use of telehealth services to provide care where patients live | |
| Develop wearables and applications designed to improve “health techquity” (simple technology solutions designed to alleviate health disparities) or address medication compliance and lifestyle management |
CVD indicates cardiovascular disease; DPP, Diabetes Prevention Program; DSMES, Diabetes Self‐Care Management Education and Support.
Panel 1: Understanding the Role of the Healthcare System in Quality Improvement in Supporting People With Cardiometabolic Disorders
Role of Medications in Decreasing Cardiovascular Risk
An expansive portfolio of drug therapies is available for the treatment of DM and prediabetes. DM treatment is rapidly evolving. Some medications show favorable effects on cardiovascular outcomes in patients with DM and CVD; promising results have been recorded in cardiovascular death, heart attack, stroke, renal disease, and heart failure. The evidence base for favorable cardiovascular outcomes for these DM medications is growing. However, many additional questions still need to be addressed before evidence‐based recommendations can be implemented and widespread adoption can occur. Providers and specialists are still trying to understand how to interpret these clinical trial results, and to determine which patients are the best candidates for certain types of medications. Among the clinical questions are the following:
Which medications, if any, should be given to patients with prediabetes?
Who should make the treatment decisions and monitor for safety and side effects—the primary care physician, healthcare provider, endocrinologist, or the diabetologist?
What are the implications of these medications on healthcare costs?
Many of these questions must be addressed before current guidelines and reimbursement models can change, and before providers are likely to change their behavior.
Barriers to Clinical Management of DM Along the Lifespan
Individuals with type 1 DM have unique challenges to diagnosis and treatment. The diagnosis can be confusing, as >40% of patients are diagnosed after age 30 years.8 Individualized treatment plans with specialists are paramount to avoid severe complications of hyper‐ and hypoglycemia. There is not much evidence on what role, if any, the newer drug classes may have on CVD outcomes, and there is a substantial cost to caring for a patient with type 1 DM .
Similarly, there are many barriers in the diagnosis and treatment of individuals with type 2 diabetes mellitus (T2DM). There is confusion among healthcare professionals on which test is best to screen for and to diagnose T2DM (eg, hemoglobin A1c, oral glucose tolerance test, or fasting blood glucose). When does the relationship between impaired glucose metabolism and CVD risk begin? Weight loss is central to decreasing DM and prediabetes. However, it is very challenging for most patients. The treatment for T2DM is complex and changing quickly as additional clinical trials report on results. Clinical confusion exists on what should be first‐, second‐, and third‐line agents for these patients. Also, the cost of newer drugs makes choices more limited for many. There is a need for better guidance for providers on when to use these medications.
DM Prevention, Diagnosis, and Treatment Using a Population Systems Approach
Kaiser Permanente is a large healthcare organization that uses a systems‐based approach for prevention, diagnosis, and treatment of patients with DM. First, Kaiser's approach set a few simple, measurable treatment targets and continually monitors these measures. Second, treatment intensification of every patient was encouraged where possible. This is accomplished using a team‐based accountability model, developing a single treatment algorithm that covers ≈80% of patients with T2DM and allowing the provider some level of treatment personalization and intensification (through titration, initiation, and adherence). The last step is to measure, give providers feedback, and correct treatments until all targets are met.
The simplified treatment algorithm approach to prevent CVD has been successful. In 2004–2005, ≈70 000 patients with T2DM or CVD were treated using this algorithm and followed for 2 years. Their outcomes were compared with 170 000 control patients whose providers did not use the treatment algorithm during a similar time period. The study showed a 60% reduction in heart attacks and strokes in the low‐adherence to treatment algorithm group and an 80% reduction in these same outcomes in the high‐adherence to treatment algorithm group.9 Glycemic control has been more challenging to implement, but again the simplified treatment algorithm approach has been successful in helping to manage patients with T2DM.
Kaiser also screens all patients 45 years or older for DM every 3 years, and uses hemoglobin A1c as the screening tool. In addition, patients have the option to enroll in the DPP and/or a weight‐loss program for patients with prediabetes.
Table 2 outlines key solutions for healthcare systems and quality improvement identified during the breakout discussions.
Table 2.
Solutions for Healthcare Systems and Quality Improvement
| Key Solutions for Healthcare Systems and Quality Improvement | |
|---|---|
| Aggregate information for stakeholders | Help patients and providers better recognize the spectrum of CVD and cardiometabolic disorders using culturally sensitive, relevant, and tailored approaches |
| Bring together all interested partners and organizations to develop and champion 1 simple message about diabetes mellitus and prediabetes | |
| Simplify screening, prevention, and diagnosis | Create quick assessment tools for screening for diabetes mellitus, health knowledge and behaviors, and family history |
| Develop simple, succinct algorithms with the PCP as primary target, based on comprehensive guidelines for treatment/management of clusters of cardiometabolic health diseases (diabetes mellitus, blood pressure, lipids) | |
| Within algorithms, elevate the role of team‐based care, defining new models for the “optimal healthcare team” and ensuring inclusion and buy‐in with an emphasis on patient education and engagement | |
| Identify and promulgate systematic, simplified approaches for identification and treatment of patients with diabetes mellitus and lifestyle interventions using the full continuum of care and care transitions (eg, take the Kaiser model to federally qualified health centers with customized approach, emergency department–based episodic care to PCPs’ offices) | |
| Team‐based care approaches | Develop a team‐based approach with multidisciplinary providers such as primary healthcare providers, physician specialists, nurses, dietitians, pharmacists, community, health workers, etc |
| Encourage healthcare systems to drive patients to enroll in evidence‐based, cost‐effective programs (eg, DPP, DSMES, weight loss) | |
| Leverage technology | Utilize innovative technology to help care for patients where they are (eg, telemedicine, e‐monitoring, text messaging) |
| Explore ways to link electronic health records to pharmacy data to better measure medication adherence | |
| Improve communication between electronic health record systems to clinics to ensure coordination of care | |
| Training for healthcare providers | Focus on cultural competency training to support healthcare providers and systems to better understand the communities they serve and leverage these insights to deliver care in meaningful ways for the community |
| Advocacy | Advocate for better reimbursement on programs that work (eg, DPP, DSMES) |
| Continue policy systems and environmental change strategies working with industry (eg, changes to the food supply, control of prescription drug costs) | |
| Engage employers and payers in all aspects of AHA initiative to drive business case for new models of care delivery and management | |
| Science and research | Invest in more research on community health interventions, quality improvement, and population health approaches to diabetes mellitus |
| Create a comprehensive cardiometabolic health guideline that incorporates all risk factors into 1 centralized resource (eg, obesity, hypertension, dyslipidemia, diabetes mellitus) and that focuses on reducing CVD risk | |
| Quality improvement programs | Leverage successes from the AHA's Target: BP program to create a similar outpatient recognition and improvement program for diabetes mellitus care |
| Leverage the AHA's Get With The Guidelines capabilities to support patients with diabetes mellitus and cardiometabolic disorders | |
AHA indicates the American Heart Association; BP, blood pressure; CVD, cardiovascular disease; DPP, Diabetes Prevention Program; DSMES, Diabetes Self‐Care Management Education and Support; PCP, primary care provider.
Panel 2: Prevention Through Increasing Patient Awareness Around Cardiometabolic Risk and Empowering Individuals to be Engaged in Their Care
Complex Needs of Patients Living With Cardiometabolic Disorders
Patients face many challenges in managing DM. Patient noncompliance with treatment is a major issue; Barriers to treatment include the following:
Difficulty consistently taking and adhering to medications because of the high cost of medications and glucose‐testing supplies (eg, testing strips, lancets), addiction to drugs and alcohol, physical impairment, and blindness.
Socioeconomic issues can have a significant impact on lifestyle and compliance with treatment when they are deprioritized because of factors such as low household income, inadequate family support, lack of trust in the medical community, and lack of resources (including mental health, transportation) are more immediate concerns.
Food deserts limit access to fresh fruits and vegetables and encourage unhealthy food selection (eg “junk food”) at “corner store”‐type retailers. Lack of available food choices can also lead to higher consumption of fast food, which may not be as nutritious as fresh food choices and can lead to obesity.
Poor health literacy and limited access to health education programs (eg, DPP, Diabetes Self‐Care Management Education and Support, heart‐health education classes).
One strategy is to find ways to empower patients to take ownership of their health care. Encouraging cultural sensitivity and meeting people where they are, and in their preferred language, are also crucial to making a lasting impact in patient engagement. It is important to consider different models for success in DM and heart‐health management, and to consider nontraditional places for education, prevention, and care (eg, places of worship). There are also numerous free local and federal government outreach programs that are available to educate patients about DM. Finally, nurses and other healthcare providers are integral to the care process for these patients and can provide many of these key solutions for patients in their homes, in the language with which they are comfortable, and in a culturally sensitive and relevant way.
Challenges in Identifying Individuals With Prediabetes and Those at Risk in Adults and Children
Lack of clarity for the role of screening and treatment guidelines for prediabetes and DM may be sources of confusion in the DM clinical care community. Summit participants discussed the differing definitions for prediabetes, DM, and screening test thresholds. The AHA and American Diabetes Association define prediabetes at either a hemoglobin A1c level between 5.7% and 6.4%, fasting blood glucose between 100 and 125 mg/dL, or an oral glucose tolerance test 2‐hour blood glucose between 140 and 199 mg/dL. Additionally, the AHA and American Diabetes Association classify DM as a hemoglobin A1c ≥6.5%, fasting blood glucose ≥126 mg/dL, or oral glucose tolerance test 2‐hour blood glucose ≥200 mg/dL. Conversely, the World Health Organization primarily uses impaired fasting glucose and impaired glucose tolerance and does not have a category for people with prediabetes. It is possible to have discordant results between these 3 tests, which leaves the patient and provider to determine whether the patient would be considered to have prediabetes.
Within the pediatric community, another controversy exists around screening test thresholds and which factors should be included. A recent study showed that hemoglobin A1c alone is a poor discriminator of prediabetes in obese and overweight youth.10 There is uncertainty surrounding the best predictors for prediabetes in this population.
There are also differences in how providers treat and address people with prediabetes and DM. Experts questioned when to add medications to a treatment regimen. In many cases, for patients with prediabetes, the focus should be on lifestyle change. There is also a need to shift the conversation from defining patients with prediabetes to a focus on their “higher risk for diabetes mellitus,” which may create greater urgency around lifestyle and treatment changes if required. In addition, simple interventions that remind and empower patients to advocate for their care (and parents to ask their child's provider about their child's health) are also very important.
Challenges and Opportunities in Supporting Undertreated Audiences in Risk Management
African‐Americans, Hispanics, and American Indians/Alaskan Natives are disproportionately affected by DM.2 These racial and ethnic groups face unique challenges with diet, lifestyle, racism, and self‐management. Opportunities for combatting these issues include culturally sensitive and culturally tailored programming, using certified DM educators who can communicate in a patient's native language where needed, incorporating the family unit into the education process, and promoting family‐based learning about health conditions. It is a combined approach of prevention (eg, publicizing advantages of exercise, calorie restriction, blood pressure control), protection (eg, need for safe housing, food, travel, and water), and partnerships (eg, government agencies, providers, public/private corporations, pharmaceutical manufacturers, and community organizations).
Effective Strategies to Motivate Lifestyle Changes, Evaluation, and Counseling
To effectively motivate patients’ lifestyle changes, it is important to uncover individual motivators (eg, competition, major events in life) and demotivators (eg, depression, financial stress). Providers who can engage in a meaningful conversation with the patient can help that individual develop a meaningful treatment plan. Some questions providers should consider when discussing DM with patients are the following:
What are your barriers to success? (eg, food insecurity, change in routine, cultural beliefs).
What is considered success for you? (eg, pounds lost, clothing size, better decisions, tracking food intake).
What are the risks and benefits to making this change? (eg, cost, time commitment).
Providers who can counsel patients will help support successful outcomes and compliance. Those dialogues could include sharing successes, mitigating patient expectations, being realistic about goals, and including cut points throughout the process to ensure patients remain on track.
Complications From DM in Addition to CVD and Stroke
While CVD is the leading cause of mortality for individuals with DM, amputations are a significant complication of poorly controlled DM. Simple no‐cost and low‐cost interventions have been shown to make positive differences in outcomes. Education and communication materials such as fliers in provider offices that promote daily foot checks and good footwear can be made readily available. Having patients come to providers’ offices for toenail clipping, along with foot exams, has also been shown to be effective.
Table 3 outlines key solutions for patient education, engagement, and empowerment identified during the breakout discussions.
Table 3.
Solutions for Patient Education, Engagement, and Empowerment
| Key Solutions for Patient Education, Engagement, and Empowerment | |
|---|---|
| Information | Marketing/awareness campaign regarding prediabetes and T2DM and CVD risk |
| Develop different ways to reach patients identified with prediabetes or who are at risk for DM; providing them the right information at the right time | |
| Tools for patient conversations with healthcare providers/systems | |
| Curated sources of valid patient/community resources | |
| Develop simple and culturally tailored and sensitive messaging from a trusted source that can be shared broadly across multiple organizations | |
| Meet patients where they are through community‐based solutions | |
| Cost and reimbursement information available at point of care, discussion of lifetime costs of noncompliance | |
| Amputation‐prevention information in providers’ offices | |
| Youth‐based activities | School education, health technology, and games to increase engagement around cardiometabolic conditions |
| Teaching through lifespan, starting with children and young adults, patient‐focused awareness, and tools to support | |
| Support school‐based strategy to promote physical activity and healthy eating that promotes cardiometabolic health and prevents obesity | |
| School‐based strategies that incorporate the family to reinforce healthy habits at home | |
| Involve the family | Develop family‐based solutions that include each family member (decision makers, cook, grocery shopper, and children) |
| Screen patients and their family for multiple cardiometabolic diseases | |
| Systems‐based solutions | Codify prediabetes screening/prevention in EHRs |
| Embed patient/provider discussion tools and scripts in EHRs | |
| Share best practices | Facilitate successful multidisciplinary care models that include liaisons, healthcare providers, and community health workers |
| Knowing that every market has different needs, provide online platform to consolidate multiple solutions (toolkit or repository) for local/community‐based resources | |
| Highlight creative approaches in programming such as innovative incentives (ie, free manicures and pedicures, Uber credits for healthcare provider visits) | |
| Research | Involve patients in research; special focus to include minority and underserved populations |
| Develop a better understanding of what motivates patients for behavior change and adherence, how to meet people where they are, and how to create more effective education on DM | |
| Better understanding of patient incentives, motivators, and demotivators | |
| Develop more community worker resources | |
| Provider training and education | Create educational curriculum and training tools for all healthcare providers (eg, physicians, nurses, physician assistants, DM educators) on behavior change, motivational interviewing, shared decision‐making, and listening to their patients |
| Develop talking points and educational resources for providers on out‐of‐pocket costs for long‐term DM care | |
| Better equip and position healthcare providers to counsel on behavior change techniques from a family‐focused vs individual approach, and provide simple pathways for referral to other members of the team with this expertise | |
| Encourage providers to ask about diet, activity, and social determinants of health, and provide skill development with small, attainable goals | |
| Provide more training on team approaches to care | |
| Partnerships | Bolster patient support groups across professional societies |
| Better engage and incorporate the “patient” voice in professional and advocacy organizations | |
| Support expansion of wellness programs in workplaces, communities, and other locations | |
| Elevate existing strength of DSMES programs to combat lack of funding and support | |
| Collaborate with vascular specialists regarding microvascular/podiatry issues | |
| Work with insurance companies to invest in prevention | |
| Advocacy | Drive incremental shifts in culture to create healthier environments and mindsets, learning lessons from incremental decreases in sodium, marketing tactics that shift perceptions (eg, light vs low sodium) |
| Advocate for covered benefits for counseling/services beyond the “medical box” with a focus on employers; this requires investment in making clear case for return on investment | |
| Encourage organizations to develop a better relationship with the Centers for Medicare and Medicaid Services | |
| Advocate for innovative Medicaid‐focused programs in “Stroke Belt” states | |
| Technology | Seek expansion and better utilization of telehealth |
| Provide a central repository for communities that address underserved populations and needs | |
| Create technology‐based programs (using social media, gamification, mobile technology) to educate patients (eg, during downtime for a PCP visit, emergency department waiting room) using the principles of prevention, personalization, and precision | |
CVD indicates cardiovascular disease; DM, diabetes mellitus; DSMES, Diabetes Self‐Care Management Education and Support; EHR, electronic health records; PCP, primary care provider; T2DM, type 2 diabetes mellitus.
Panel 3: Activating Communities and Leveraging Technology to Advance the Complex Health Needs of People Living With Cardiometabolic and CVDs
Educating and Mobilizing Provider Communities to Improve Multidisciplinary Team Communication and Increase Clinical Best Practices Across the Spectrum of Care
Barriers to health for some patients with cardiometabolic conditions include lower income, disparities in care, cultural insensitivity, literacy levels, lack of social support, pill burden, medication and diabetic supply costs, no access to regular care, difficulty getting to appointments, lack of sidewalks, lack of access to grocery stores, and multiple job and family responsibilities. Utilizing a team of healthcare providers such as nurses or DM educators may present a viable solution to addressing some of these barriers. There are more than 2.85 million nurses across the United States who could be activated to educate patients about DM, prediabetes, and metabolic syndrome through a variety of venues and audiences.11 In addition, there are certificate programs available through organizations such as the Preventative Cardiovascular Nurses Association to help train providers in behavior change. This certification includes information on how to perform cardiovascular risk assessments using individualized tools and high‐risk communication strategies, and develops an introduction to motivational interviewing and coaching. This includes how to select and implement behavior change strategies with patients including developing goals, planning for behavior change, and evaluating goal completion. Ultimately, all providers must be able to effectively identify and assess CVD risk factors, implement treatment plans, and incorporate lifestyle and pharmacologic therapy for their patients.
Advancing Cardiometabolic Health Through Community‐Based Programs
The National DPP, Diabetes Self‐Care Management Education and Support, and the Chronic Disease Self‐Management Program, among others, have been effective in helping patients prevent, treat, and manage their DM or prediabetes.12 Building community–clinic linkages are increasingly important in achieving desired health outcomes and supporting those with DM and cardiometabolic disorders. This can move traditional hospital‐based programs to the community and make use of community‐based health workers to implement them. This may allow physicians to offer services where their patients reside, work, or worship; and this aligns with value‐based healthcare trends; potentially increases insurance coverage to offset patient expenses; and might help achieve the aims of better access to care, better outcomes, and lower costs. Community‐based organizations also are seeing the value in partnering with healthcare organizations by using established programs (eg, National DPP), data collection mechanisms, and reporting for recognition/certification as well as increased reimbursement. The major barriers to these linkages are lack of provider awareness of these programs and lack of information provided by community partners on the care and outcomes achieved from these programs. These barriers can be overcome through increased communication between partners.
The Role of Health‐Tech in Cardiometabolic Health
There are more than 250 000 health mobile applications available in the marketplace; however, there are no specific standards on what information is collected, how these data are stored and used, and the potential uses of applications. The AHA's Center for Health Technology and Innovation is working to overcome barriers in the adoption of technology. These barriers can be divided into 3 groups:
Patients (when to use the apps/wearables, which is the right product, validation and reliability, how to interpret and apply the data).
Digital device and app companies (defining the use case, understanding patient/provider needs, incorporating into clinical care).
Clinicians, insurers, health systems, and pharmaceutical manufacturers (inertia/sharing control, need for evidence, incorporating the health tech data collected into workflows, IT implementation, and reimbursement issues).
It is important to align the science with the products and build care plans that can be used with a wide range of technologies. The AHA is using its core statements and guidelines to create care plans, algorithms, and health education content items for health technology companies. Better understanding of what technology patients can access and how to connect these technologies to the health record will help AHA and others support viable solutions. The concept of “health techquity” was introduced: the intersection between better screening for DM and finding the simplest available technology to better serve people with DM and prediabetes. This is in effect looking to use the cheapest, most scalable technologies rather than trying to implement an expensive, difficult‐to‐access solution.
Table 4 outlines key solutions for community‐based interventions and health technology identified during the breakout discussions.
Table 4.
Solutions for Community‐Based Interventions and Health Technology
| Key Solutions for Community‐Based Interventions and Health Technology | |
|---|---|
| Systems‐based issues of technology use | Leverage the healthcare system to focus on readmission rates and enable community/tech‐based programming within the “30‐d window” |
| Incorporate training on integration of consumer health tech and community‐based care in teaching for the next generation of healthcare providers | |
| Multidisciplinary connections, particularly pharmacist, community, health/social workers, and patient navigators | |
| Integrate community program data into EHRs | |
| Technology solutions and audiences | Tool/app that supports patient needs with capabilities of lifestyle management, medication management, goals that link to providers, and support of evidence‐based programs (eg, DPP) |
| Crowdsource ideas from patients about what would be transformative in their communities for DM care | |
| Engage schools for healthy behaviors/health education | |
| Text messaging program to deliver health messaging, policy, and advocacy | |
| Continuous glucose monitoring for patients with T2DM in remote or underserved populations (tech translation) | |
| Technology solutions and audiences | Engage people with obesity to prevent development of other cardiometabolic conditions |
| “Consumerize” and/or gamify patient portals | |
| Adapt technology based on populations | |
| Mobilizing faith‐based communities | |
| Certification/standardization of technology | Develop validation/certification for wearables/apps/online programs (eg, use AHA's Heart Check Certification Program for food as a template) |
| Identify criteria and filters for high‐quality technology. Develop recommendations for how data are protected, stored, and shared | |
| Public awareness | Create a campaign (with public personas or celebrities) including simplified messaging around DM, obesity, high blood pressure, cholesterol, and their links to CVD |
| Encourage middle school and high school students to get into healthcare professions | |
| Development of audience‐specific messages, focusing on end users such as oldest and youngest | |
| Getting patients to use technology | Using behavioral economics principles, develop and test incentive programs |
| Combine health tech features within already popular non‐health‐focused apps (ie, fashion, news, social networking, and celebrity gossip) | |
| Scale existing/new apps for positive reinforcement | |
| Research | Pilot programs in smaller or underserved communities to understand and prioritize what actions and programs to implement |
| Engage universities and researchers on novel mechanisms to reach vulnerable populations | |
| Recruit American Indian/Alaska Native populations and other underserved or disproportionately affected race/ethnicity populations into genome‐sequencing studies | |
| Partnerships | Create strategic partnerships with nontraditional partners and industries to increase awareness of and better treat people with prediabetes and DM |
| Engage trusted leaders in the community to deliver health education (eg, clergy, barbers, community health workers) | |
| Evidence‐based employee wellness and promotion of healthy workplaces | |
| Advocacy | Reimbursement strategies to drive scale for devices/technology, community programs, and healthcare provider time‐to‐use data for care |
| Better reimbursement for telehealth, DPP, Medicaid, and food programs | |
| Having alternate, reimbursable forms of communication between patients and providers | |
| Promote DM programming to be used for hospitals’ “community benefit dollars,” which are required by the Affordable Care Act for hospitals to invest in their communities | |
AHA indicates American Heart Association; CVD, cardiovascular disease; DM, diabetes mellitus; DPP, Diabetes Prevention Program; EHRs, electronic health records; T2DM, type 2 diabetes mellitus.
Discussion
Through an electronic voting process for attendees, the key factors and proposed solutions in the 3 panels were further prioritized for AHA to consider after the Cardiometabolic Health and Diabetes Summit (Table 1).
The solutions presented throughout the Cardiometabolic Health and Diabetes Summit fall within each of these categories. Each “puzzle” piece has its own potential barriers that need to be addressed to efficiently and effectively help patients and families manage cardiometabolic risk factors and prevent CVD.
Figure 3 shows the interplay between the different solutions that have been presented to help advance the care of people with prediabetes, DM, and cardiometabolic disorders. The patient is the central piece of the “puzzle” as we work to better manage CVD and cardiometabolic risk. The 4 central factors that directly impact the patient and his/her health outcomes are as follows: community in which he/she lives; social determinants of health that impact the patient's life; family members (who are integral to the diet/lifestyle and genetic predisposition); and the healthcare team that helps the patient manage risk factors. Secondary factors that play an important role in the patient managing cardiometabolic risk factors and health outcomes are as follows: advocacy and payers; systems of care; approaches from the inpatient and outpatient settings; and health technology and science/research. Ultimately, there is much more work that will need to be done in this area to complete the puzzle and align these factors together to transform the way in which patients with DM and cardiometabolic risk factors are diagnosed, treated, and managed in the United States.
Figure 3.
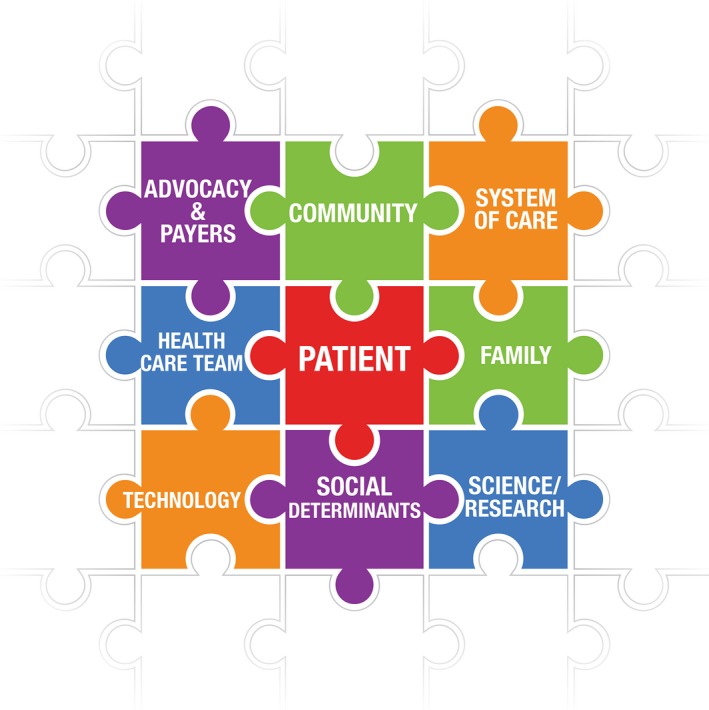
Unlocking the puzzle of caring for the patient with diabetes mellitus/cardiometabolic health conditions.
Conclusion
The multidisciplinary group of professionals, providers, patients, and organizations at the Cardiometabolic Health and Diabetes Summit has set the stage for a new initiative that will begin to pull these disparate puzzle pieces together and to generate a cohesive vision and strategy for the future. As further research is conducted in the basic, clinical, and population health spaces, the link between DM, cardiometabolic risk, and CVD becomes strengthened and the need for a comprehensive approach to identification, treatment, management, and prevention is more apparent. In order to change the trajectory of the ever‐growing numbers of people who will develop DM and other cardiometabolic conditions, AHA along with the DM community can and must solve this “complex puzzle” in order to tackle this national issue and decrease mortality from DM and CVD.
Sources of Funding
AstraZeneca, Boehringer Ingelheim & Eli Lilly and Company, and the Pfizer‐Merck Alliance are the National Supporters of American Heart Association's Cardiometabolic Health and Diabetes Summit. The summit was also supported by an educational grant from Novo Nordisk, Inc.
Disclosures
The following authors have disclosures and receive funding: Dr Carson: Amgen; Dr Eckel:Novo Nordisk, Sanofi; Dr Wang: AstraZeneca, Merck, Pfizer, and Eli Lilly. The remaining authors have no disclosures to report.
Acknowledgments
We thank our distinguished speakers and breakout session facilitators: Samuel Arce, MD; Nancy Brown, AHA CEO; Doris Browne, MD; Shannon Christen, RD; Jim Dudl, MD; Goutham Rao, MD; Gregory Schwartz, MD, PhD; Bryce Smith, PhD; Anne Sumner, MD; and Patrick Wayte.
J Am Heart Assoc. 2018;7:e009271 DOI: 10.1161/JAHA.118.009271.
References
- 1. Centers for Disease Control and Prevention . National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2017. [Google Scholar]
- 2. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jimenez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brunzell JD, Davidson M, Furberg CD, Goldberg RB, Howard BV, Stein JH, Witztum JL. Lipoprotein management in patients with cardiometabolic risk: consensus conference report from the American Diabetes Association and the American College of Cardiology Foundation. J Am Coll Cardiol. 2008;51:1512–1524. [DOI] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention . National Center for Chronic Disease Prevention and Health Promotion, Division of Diabetes Translation, 2018. Available at: https://www.cdc.gov/diabetes/prevention/index.html. Accessed July 23, 2018.
- 5. Narayan KMV, Boyle JP, Geiss LS, Saaddine JB, Thompson TJ. Impact of recent increase in incidence on future diabetes burden. Diabetes Care. 2006;29:2114. [DOI] [PubMed] [Google Scholar]
- 6. Sharma MA, Cheng N, Moore M, Coffman M, Bazemore AW. Patients with high‐cost chronic conditions rely heavily on primary care physicians. J Am Board Fam Med. 2014;27:11–12. [DOI] [PubMed] [Google Scholar]
- 7. Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014 to 2060. Curr Popul Rep. 2014;P25–P1143. [Google Scholar]
- 8. Thomas NJ, Jones SE, Weedon MN, Shields BM, Oram RA, Hattersley AT. Frequency and phenotype of type 1 diabetes in the first six decades of life: a cross‐sectional, genetically stratified survival analysis from UK Biobank. Lancet Diabetes Endocrinol. 2018;6:122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dudl RJ, Wang MC, Wong M, Bellows J. Preventing myocardial infarction and stroke with a simplified bundle of cardioprotective medications. Am J Manag Care. 2009;15:e88–e94. [PubMed] [Google Scholar]
- 10. Khokhar A, Naraparaju G, Friedman M, Perez‐Colon S, Umpaichitra V, Chin VL. Comparison of A1C to oral glucose tolerance test for the diagnosis of prediabetes in overweight and obese youth. Clin Diabetes. 2017;35:133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Statistics BoL . Occupational employment statistics. 2016.
- 12. Brown CA, Lilford RJ. The stepped wedge trial design: a systematic review. BMC Med Res Methodol. 2006;6:54. [DOI] [PMC free article] [PubMed] [Google Scholar]


