Abstract
Objective
Cardiac chamber dimensions are race and anthropometry dependent. We determined the age and gender specific 3-Dimensional echocardiographic (3DE) reference values for dimensions and function of left ventricle (LV) and left atrium (LA) in normal Indian adults.
Methods
This single center prospective study enrolled 133 adult Indians free of heart disease and/or hypertensions, subjecting them to 3DE measurements of left atrial (LA) & left ventricular (LV) volumes, function and left ventricular mass (LVM). The higher limits of normal cut-offs were determined for these parameters and their dependency on age, gender and anthropometry were analyzed.
Results
The body surface area (BSA) corrected higher limit cut-offs were: 59.37 ml/m2 for LV end diastolic volume (59.19 ml/m2 and 59.61 ml/m2 for men and women, respectively; P = NS); 23.48 ml/m2 for LV end systolic volume (23.27 ml/m2 and 23.11 ml/m2 for men and women, P = NS). Mean LVEF was 64.79% ± 7.26 (62.99% ± 6.51 and 67.05% ± 7.58 in men and women, P = NS). Men had higher LVM than women (119.79 g±23.95 vs. 103.26 g±23.76, P < 0.001), this difference disappeared after BSA indexing. The higher limit cut-offs for normal LA volumes were 20.49 ml for minimum volume (21.18 ml and 19.46 ml for men and women, P = NS) and 39.76 ml for maximum volume (39.60 ml and 40.03 ml in men and women, P = NS). The parameters were smaller compared to western populations but the differences attenuated after BSA indexing.
Conclusions
The study reports normal 3DE parameters of size and function of left heart chambers in Indians.
Keywords: Three-dimensional echocardiography, Left atrial volume, Left ventricular end diastolic volume, Left ventricular end systolic volume, Left atrial emptying fraction
1. Introduction
Evaluation of ventricular and atrial volumes and function is probably the most promising application of three-dimensional echocardiography (3DE) because of its ability to assess the whole chamber simultaneously. Cardiac chamber volumes and functions are major indicators of disease severity and prognosis in presence of various acquired1 as well as congenital2 structural heart diseases. Dimensions of cardiac chambers are known to be affected by racial and anthropometric factors.3, 4, 5 Although ventriculography using cardiac catheterization or cardiac magnetic resonance (CMR) are gold standards for assessing left ventricle (LV) in terms of dimensions and function, 3DE has strong potential for routine use because it is more cost effective, does not need contrast exposure and has superior accuracy compared to two-dimensional echocardiography (2DE) by virtue of its better ability to interrogate the actual chamber geometry. Other than operator experience, one of the major factors limiting its wide spread use is relative lack of data on normal parameters. Although some studies have defined and validated RT3DE derived normal ventricular parameters in western4 or other Asian3 populations, there is scarcity of such data in Indian subjects; moreover, there is no published Indian report on 3DE determined volumes or function of left atrium (LA).
In this study, we investigated the: (a) 3DE derived values of LV and LA volumes, left ventricular ejection fraction (LVEF), LV mass (LVM) and left atrial emptying fraction (LAEF) in healthy Indian adults and (b) the effect of age, gender and anthropometric factors on 3DE derived LA and LV volumetric and functional parameters.
2. Methods
2.1. Study design and subjects
This was a single center prospective study wherein 133 adult Indians aged 18 years or above, free of overt heart disease and/or hypertension, were enrolled. Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg at the time of recruitment in the study or history of current or previous intake of anti-hypertensive drugs. Heart disease was excluded by history, clinical examination, 12-lead electrocardiogram (ECG) and 2DE; however, subjects having mild isolated LV diastolic dysfunction were not excluded from the study. Hospital employees, students and patients’ attendants served as subjects. Written informed consent was obtained from them.
Baseline characteristics including age, gender, height, weight, history of diabetes mellitus, heart rate (HR), SBP and DBP were noted. Body surface area (BSA) was calculated by entering values of weight and height into software using Du Bois method.6 This was followed by 3DE recording of full volume loops including LV and LA, which were later analyzed as described below. Individuals with sub-optimal 3D images were not included in the study.
2.2. 3D-echocardiography
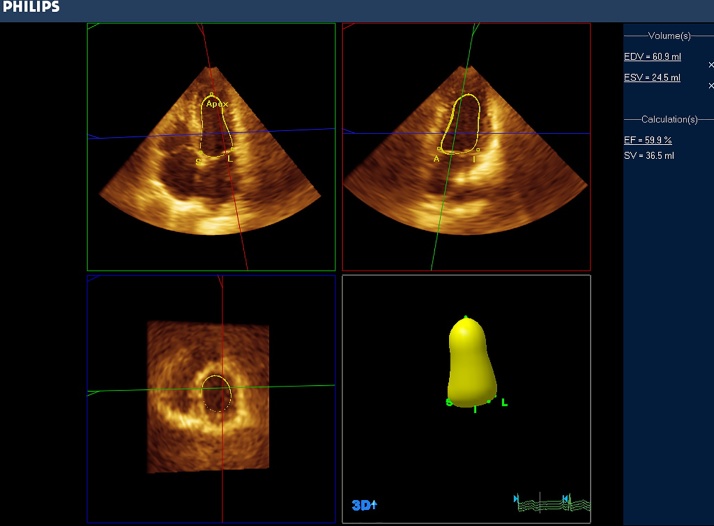
All subjects underwent ECG gated 3DE imaging in apical 4 chamber view, recording LV and LA full volume loops on commercial iE33 equipment (Philips Medical Systems, Andover, MA, USA) using X5-1Matrix-array transducer. The sector width, speed and depth were optimized to obtain maximum possible volume rate (average ∼22 volumes per second). Lateral width was adjusted to include whole LV including epicardial borders so that LV mass could also be assessed. Whole LA was included in the loops by optimizing depth. Gain settings were adjusted to obtain best possible endocardial definition. Since it has been observed that single beat full volume acquisition under-estimates LVEF due to lower temporal resolution, while 4-beat acquisitions result in more stitching artifacts7, we used 2-beat RT3DE for recording full volume loops in all patients. All recordings were analyzed off-line, using Q-Lab software, by a single cardiologist having ≥10 years’ experience in echocardiography, having done about 7000 2DE (trans-thoracic and trans-esophageal) and 250 3DE. After selecting end diastolic and end systolic frames, appropriate points i.e. septal, lateral, anterior, inferior and apical, were marked in order to obtain LV volumes and ejection fraction by a semi-automated analysis (Fig. 1). The software automatically tracked cavity-endocardium interface which was confirmed in short axis view and manually edited whenever needed. The papillary muscles were included in the LV cavity. Following this, in LV end diastolic frame, the same points were edited and placed on epicardial surface to obtain epicardial LV volume. LV myocardial volume was calculated by subtracting left ventricular end diastolic volume (LVEDV) from LV epicardial volume i.e. volume obtained by tracing epicardial borders. LVM was calculated as product of myocardial volume and myocardial tissue density i.e. 1.05 g/ml.
Fig. 1.
3D-echocardiographic determination of left ventricle volumes and function. 4-chamber (top left), 2-chamber (top right) and short axis (bottom left) planes showing semi-automatic tracing of endocardial borders and resultant 3D cast of the LV cavity (bottom right).
The minimum LA volume (LAV-min) and maximum LA volume (LAV-max) were assessed in end diastolic and end systolic frames respectively. LA volumes were determined by marking septal, lateral, anterior and inferior points on mitral annulus and fifth point at roof of LA wall–cavity border. Manual editing was done to exclude LA appendage and pulmonary veins. As a measure of LA function, LAEF, was calculated as difference of LAV-max and LAV-min divided by LAV-max and multiplied by 100, as described by other investigators.8 Hence, the full volume loops were analyzed to assess following parameters: LVEDV, left ventricular end systolic volume (LVESV), LVEF, LVM, LAV-min, LAV-max and LAEF. BSA indexed values for volumes and mass were obtained after dividing the respective parameter by BSA (referred to in this article with suffix “i” added to the respective parameter e.g. LVEDVi, LVESVi, LVMi, LAVi-min and LAVi-max). Finally, the data were analyzed for influence of age, gender and other baseline characters. The effect of age was studied by dividing the subjects into two age groups, 18–39 years and ≥ 40 years.
2.3. Statistical methods
Categorical variables were summarized as frequencies and percentages; continuous variables were summarized using mean ± standard deviation (SD). Paired Student’s t-tests were performed to test for significant differences between continuous variables. Pearson’s correlation and Spearman’s rank correlation were applied to find out the correlation between studied 3DE parameters and baseline characteristics. Multivariate linear regression was performed wherever correlation coefficient was ≥0.2 for anthropometric variables.
We examined the degree of agreement between 3D echo parameters measured by same observer at two different points in time (intra-observer variability) using Pearson’s correlations and Bland-Altman analysis. This was done in 21 randomly selected subjects.
Statistical analysis was performed using SPSS version 15.0 for Windows (SPSS, Chicago, IL) and Medcalc Statistical 17.4 (Acacialaan Belgium), the latter used for Bland Altman analysis only. P value of <0.05 was considered statistically significant. The cut-off values for higher limits of normal volumetric LA and LV parameters were determined as mean + 2SD. This was based on standard method that comprises of estimation of 95% range for any parameter in the index population, defined as mean ± 1.96 (rounded-up to 2).
3. Results
After screening, 133 eligible subjects with mean age 38.73 ± 12.96 years (range 18–70 years), including 74 (55.64%) men and 59 (44.36%) women, were included in this study. Their gender classified anthropometric, clinical and echocardiographic findings are summarized in Table 1. Men were taller, heavier, and had higher BSA than women. Women had comparatively higher HR.
Table 1.
Anthropometric, clinical & 3D-echocardiographic features.
| All (n = 133) | Female (n = 59) | Male (n = 74) | P value | |
|---|---|---|---|---|
| Age (y) | 38.73 ± 12.96 | 38.79 ± 14.51 | 38.67 ± 11.69 | 0.959 |
| Weight (kg) | 60.65 ± 11.06 | 55.88 ± 10.01 | 64.46 ± 10.42 | <0.001 |
| Height (cm) | 160.97 ± 9.59 | 154 ± 7.08 | 166.53 ± 7.47 | <0.001 |
| BSA (m2) | 1.64 ± 0.19 | 1.54 ± 0.16 | 1.72 ± 0.17 | <0.001 |
| HR (bpm) | 76.15 ± 12.06 | 79.3 ± 11.34 | 73.63 ± 12.11 | 0.007 |
| SBP (mmHg) | 117.95 ± 11.04 | 116.95 ± 10.98 | 118.74 ± 11.1 | 0.354 |
| DBP (mmHg) | 76.78 ± 7.81 | 76.54 ± 7.91 | 76.97 ± 7.78 | 0.753 |
| DM, n (%) | 8 (6.1%) | 5 (8.5%) | 3 (4.1%) | 0.465 |
| DD, n (%) | 34 (25.6%) | 19 (32.2%) | 15 (20.3%) | 0.117 |
| LVEDV(ml) | 69.49 ± 16.34 | 64.01 ± 15.41 | 73.86 ± 15.82 | <0.001 |
| LVESV(ml) | 24.58 ± 7.84 | 21.25 ± 7.89 | 27.24 ± 6.76 | <0.001 |
| LVEDVi (ml/m2)* | 42.47 ± 8.45 | 41.85 ± 8.88 | 42.97 ± 8.11 | 0.447 |
| LVESVi (ml/m2)* | 14.94 ± 4.27 | 13.79 ± 4.66 | 15.85 ± 3.71 | 0.005 |
| LVEF (%) | 64.79 ± 7.26 | 67.05 ± 7.58 | 62.99 ± 6.51 | 0.001 |
| Myocardial Volume (ml) | 107.11 ± 23.96 | 98.35 ± 22.62 | 114.09 ± 22.8 | <0.001 |
| LVM (g) | 112.46 ± 25.16 | 103.26 ± 23.76 | 119.79 ± 23.95 | <0.001 |
| LVMi (g/m2)* | 68.83 ± 13.53 | 67.39 ± 12.81 | 69.97 ± 14.06 | 0.276 |
| LV Mass/volume ratio (g/ml) | 1.67 ± 0.47 | 1.67 ± 0.5 | 1.67 ± 0.44 | 0.982 |
| LAV-min (ml) | 12.77 ± 3.86 | 12.12 ± 3.67 | 13.28 ± 3.95 | 0.085 |
| LAV-max (ml) | 25.24 ± 7.26 | 24.85 ± 7.59 | 25.54 ± 7.03 | 0.585 |
| LAVi-min (ml/m2)* | 7.81 ± 2.3 | 7.89 ± 2.26 | 7.74 ± 2.36 | 0.715 |
| LAVi-max (ml/m2)* | 15.49 ± 4.4 | 16.21 ± 4.72 | 14.91 ± 4.07 | 0.090 |
| LAEF (%) | 48.99 ± 12.34 | 50.09 ± 11.53 | 48.12 ± 12.96 | 0.361 |
Data presented as mean ± SD. BSA, body surface area; HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; DM, diabetes mellitus; DD, diastolic dysfunction LV, left ventricle; EDV, end diastolic volume; ESV, end systolic volume; EF, ejection fraction; LVM, LV mass; LAV-min, minimum left atrial volume and LAV-max, maximum left arterial volume. *parameters indexed for BSA (suffix “I” indicates indexed).
3.1. LV parameters
Table 1 summarizes the 3DE parameters observed in the study group. Mean LVEDV was 69.49 ml ± 16.34 (73.86 ml ± 15.82 in men and 64.01 ± 15.41 in women, P < 0.001). Mean LVESV was 24.58 ml ± 7.84 (27.24 ml ± 6.76 and 21.25 ml ± 7.89 in men and women respectively, P < 0.001). In the overall population, the cut-off values for higher limits of normal LV parameters were: 102.17 ml for LVEDV (105.46 ml and 94.83 ml for men and women respectively; P < 0.001); and 40.26 ml for LVESV (40.76 ml and 37.03 ml for men and women respectively; P < 0.001). When corrected for BSA, the cut-off values for over-all population were 59.37 ml/m2 for LVEDVi (59.19 ml/m2 and 59.61 ml/m2 for men and women respectively; P = NS); and 23.48 ml/m2 for LVESVi (23.27 ml/m2 and 23.11 ml/m2 for men and women respectively; P = 0.005). Mean LVEF was 64.79% ± 7.26 in over-all population (62.99% ± 6.51 and 67.05% ± 7.58 in men and women respectively, P = 0.001).
Men had significantly higher LVM than women (119.79 g ± 23.95 vs. 103.26 g ± 23.76, P < 0.001) and LVM in over-all population was112.46 g ± 25.16. However, the gender difference in LVM was not seen after correction for BSA (68.83 g/m2 ± 13.53 in over-all population; 69.97 g/m2 ± 14.06 and 67.39 g/m2 ± 12.81 in men and women respectively, P = NS). The LVM to volume ratio (LVM/LVEDV) was also comparable in men and women (1.67 g/ml ± 0.44 and 1.67 g/ml ± 0.50 respectively, P = NS).
3.2. LA parameters
The cut-off values for higher limit of normal LA volumes were 20.49 ml for LAV-min in over-all population (21.18 ml for men and 19.46 ml for women, P = NS). Similarly, the higher cut-off for LAV-max was 39.76 ml in the population as a whole (39.60 ml and 40.03 ml in men and women respectively, P = NS). The corresponding cut-offs for LAVi-min and LAVi-max were 15.62 ml/m2 and 24.29 ml/m2 respectively. When corrected for BSA, no gender differences were found in LAVi-max and LAVi-min. LAEF was similar in both men and women (48.99% ± 12.34 over-all; and 48.12% ± 12.96 in men and 50.09% ± 11.53 in women; P = NS).
3.3. Effect of age, gender, anthropometric and baseline physiological variables on LV and LA parameters
Table 2 summarizes the effect of age and gender on all studied parameters. It can be seen that females in ≥40 years age group had significantly smaller LV volumes than those in 18–39 years’ age group, even when the parameters were adjusted for BSA; while, age did not affect LA parameters significantly. BSA indexed parameters were not influenced by age in men.
Table 2.
3D Echocardiographic parameters classified by age groups and gender.
| FEMALE |
MALE |
|||||
|---|---|---|---|---|---|---|
| <40 years (26.43 y ± 5.22) (n = 30) | ≥40 years (51.59 y ± 8.65) (n = 29) | P value | <40 years (30.26 y ± 5.93) (n = 43) | ≥40 years (50.35 y ± 6.36) (n = 31) | P value | |
| LVEDV(ml) | 68.73 ± 11.48 | 59.14 ± 17.53 | 0.016 | 77.57 ± 15.36 | 68.71 ± 15.2 | 0.016 |
| LVESV(ml) | 23.81 ± 5.67 | 18.61 ± 9.03 | 0.010 | 27.81 ± 6.35 | 26.46 ± 7.31 | 0.400 |
| LVEDVi (ml/m2)* | 44.67 ± 6.44 | 38.93 ± 10.16 | 0.012 | 44.48 ± 7.7 | 40.88 ± 8.31 | 0.059 |
| LVESVi (ml/m2)* | 15.51 ± 3.4 | 12.01 ± 5.16 | 0.003 | 15.92 ± 3.24 | 15.76 ± 4.35 | 0.858 |
| LVEF (%) | 65.1 ± 6.27 | 69.1 ± 8.34 | 0.039 | 63.93 ± 6.54 | 61.69 ± 6.35 | 0.147 |
| LVM (g) | 101.22 ± 19.37 | 105.37 ± 27.75 | 0.507 | 120.31 ± 21.48 | 119.06 ± 27.37 | 0.827 |
| LVM (g/m2) | 65.75 ± 11.15 | 69.09 ± 14.33 | 0.322 | 69.06 ± 11.27 | 71.24 ± 17.34 | 0.544 |
| LAV-min (ml) | 12.11 ± 3.82 | 12.14 ± 3.57 | 0.974 | 13.27 ± 3.87 | 13.3 ± 4.11 | 0.970 |
| LAV-max (ml) | 26.74 ± 8.14 | 22.89 ± 6.55 | 0.050 | 25.49 ± 7.79 | 25.62 ± 5.93 | 0.942 |
| LAVi-min (ml/m2)* | 7.86 ± 2.29 | 7.93 ± 2.27 | 0.909 | 7.54 ± 1.97 | 8.03 ± 2.82 | 0.414 |
| LAVi-max (ml/m2)* | 17.41 ± 4.97 | 14.97 ± 4.19 | 0.047 | 14.61 ± 4.32 | 15.33 ± 3.72 | 0.459 |
| LAEF (%) | 54.2 ± 8.65 | 45.85 ± 12.7 | 0.004 | 46.62 ± 11.43 | 50.2 ± 14.77 | 0.243 |
LV, left ventricle; EDV, end diastolic volume; ESV, end systolic volume, EF, ejection fraction; LVM, left ventricular mass, LAV-min, minimum left atrial volume; LAV-max, maximum left atrial volume; LAEF, left atrial emptying fraction. *parameters indexed for BSA (suffix “I” indicates indexed).
On correlation analysis (Table 3), weight, height and BSA revealed highly significant correlation with LVEDV, LVESV and LVM; however, after indexing for BSA, this correlation either became insignificant (LVEDVi and LVMi) or relatively weaker (LVESVi). Similar observations were seen in relation to LA volumetric parameters before and after BSA correction.
Table 3.
Correlation between 3D-echocardiographic parameters & baseline characteristics.
| Age (y) |
Weight (kg) |
Height (cm) |
BSA (m[2]) |
HR (bpm) |
SBP (mmHg) |
DBP (mmHg) |
DD |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r | P | r | P | r | P | r | P | r | P | r | P | r | P | r | P | |
| LVEDV(ml) | −0.267a | 0.002 | 0.408a | <0.001 | 0.485a | <0.001 | 0.478a | <0.001 | −0.163 | 0.060 | −0.069 | 0.433 | 0.025 | 0.778 | −0.297a | 0.001 |
| LVESV(ml) | −0.222b | 0.010 | 0.382a | <0.001 | 0.519a | <0.001 | 0.464a | <0.001 | −0.143 | 0.102 | −0.021 | 0.814 | 0.039 | 0.659 | −0.238a | 0.006 |
| LVEDVi (ml/m2)# | −0.246a | 0.004 | −0.063 | 0.468 | 0.105 | 0.228 | −0.014 | 0.870 | −0.134 | 0.124 | −0.184b | 0.034 | −0.069 | 0.433 | −0.279a | 0.001 |
| LVESVi (ml/m2)# | −0.218b | 0.012 | 0.062 | 0.476 | 0.279a | 0.001 | 0.133 | 0.127 | −0.132 | 0.129 | −0.092 | 0.291 | −0.032 | 0.715 | −0.233a | 0.007 |
| LVEF (%) | 0.092 | 0.292 | −0.149 | 0.088 | −0.269a | 0.002 | −0.197b | 0.023 | 0.042 | 0.634 | −0.026 | 0.770 | −0.017 | 0.846 | 0.050 | 0.565 |
| LVM (g) | 0.036 | 0.678 | 0.438a | <0.001 | 0.421a | <0.001 | 0.467a | <0.001 | −0.191b | 0.028 | −0.039 | 0.659 | −0.003 | 0.969 | −0.002 | 0.977 |
| LVMi (g/m2)# | 0.120 | 0.169 | −0.044 | 0.613 | 0.034 | 0.698 | −0.035 | 0.693 | −0.167 | 0.055 | −0.109 | 0.213 | −0.054 | 0.535 | 0.076 | 0.385 |
| LAV-min (ml) | 0.081 | 0.356 | 0.217b | 0.012 | 0.237a | 0.006 | 0.244a | 0.005 | −0.110 | 0.206 | 0.062 | 0.475 | 0.146 | 0.094 | 0.016 | 0.859 |
| LAV-max (ml) | −0.071 | 0.420 | 0.174b | 0.046 | 0.277a | 0.001 | 0.221b | 0.011 | −0.066 | 0.449 | −0.008 | 0.926 | 0.085 | 0.329 | −0.139 | 0.110 |
| LAVi-min (ml/m2)# | 0.142 | 0.104 | −0.127 | 0.144 | −0.038 | 0.661 | −0.118 | 0.177 | −0.084 | 0.338 | 0.016 | 0.851 | 0.107 | 0.221 | 0.069 | 0.431 |
| LAVi-max (ml/m2)# | −0.026 | 0.765 | −0.205b | 0.018 | −0.019 | 0.826 | −0.174b | 0.045 | −0.043 | 0.624 | −0.071 | 0.414 | 0.021 | 0.807 | −0.094 | 0.282 |
| LAEF (%) | −0.140 | 0.107 | −0.074 | 0.397 | 0.005 | 0.953 | −0.061 | 0.482 | 0.111 | 0.205 | −0.016 | 0.853 | −0.015 | 0.868 | −0.092 | 0.292 |
BSA, body surface area; HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; DM, diabetes mellitus; DD, diastolic dysfunction; LV, left ventricle; EDV, end diastolic volume; ESV, end systolic volume; EF, ejection fraction; LVM, left ventricular mass; LAV-min, minimum left atrial volume; LAV-max, maximum left atrial volume. #parameters indexed for BSA (suffix “I” indicates indexed).
Correlation is significant at the 0.01 level (2-tailed).
Correlation is significant at the 0.05 level (2-tailed).
To study the independent effect of baseline anthropometric variables on LV volumes, LV mass and LA volumes, Multivariate linear regression was performed with parameters having correlation coefficients ≥0.2 (i.e. weight, height and BSA). We found that the individual variables did not have any significant effect on measured parameters.
In relation to physiological variables, the BSA indexed LV or LA parameters did not show any correlation with HR or DBP (Table 3) except LVEDVi which indicated weak negative correlation with SBP.
3.4. Effect of LV diastolic dysfunction
Grade one diastolic dysfunction was seen as incidental finding in 25.6% subjects (32.2% women and 20.3% men). It did not show correlation with LA volumes or BSA corrected LA volume indices.
3.5. Reproducibility of 3DE parameters
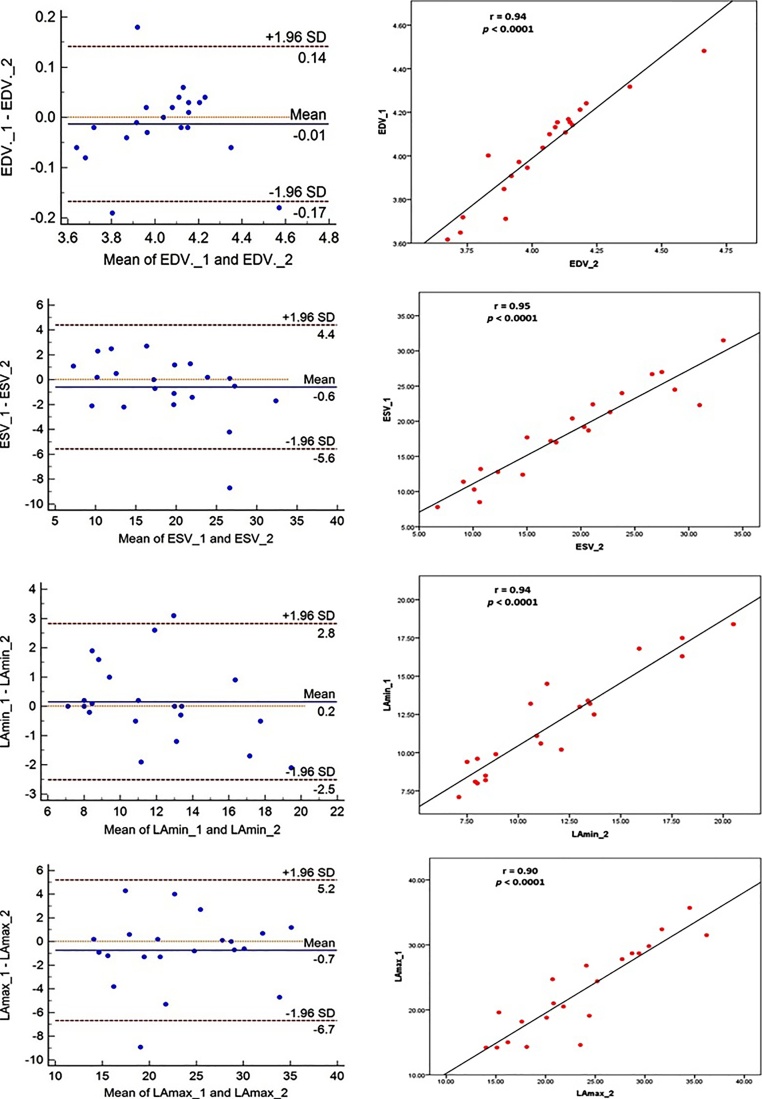
As evident in Table 4 and Fig. 2, the intra-observer variability assessment showed excellent reproducibility in the form of high correlation coefficients and low bias in Bland Altman analysis.
Table 4.
Intra-observer variability for measured LV and LA parameters.
| Parameter | Correlation coefficienta | Mean bias ± SD |
|---|---|---|
| LVEDV | 0.94 | −0.01 ± 0.07 |
| LVESV | 0.95 | −0.60 ± 2.54 |
| LVM | 0.87 | −2.83 ± 11.27 |
| LAV-min | 0.94 | 0.15 ± 1.36 |
| LAV-max | 0.90 | −0.74 ± 3.03 |
LVEDV, left ventricular end diastolic volume; LVESV, left ventricular end systolic volume; LVM, LV mass; LAV-min, minimum left atrial volume and LAV-max, maximum left arterial volume.
All correlations are significant at 0.001 level.
Fig. 2.
Intra-observer variability in assessment of LV and LA parameters as analyzed by Bland Altman method (left) and Pearson’s correlation method (right).
4. Discussion
The current study reports normal 3DE values of volumetric, mass and functional parameters of LV and LA in healthy Indian adults.
4.1. Advantages of 3DE over other imaging modalities
Although CMR is gold standard for determining volumetric and functional parameters of cardiac chambers, 3DE, due to its wider availability and lower cost, can serve as quicker and still accurate guide providing quantitative determinants of prognosis and treatment results during follow-up in cardiac disease. Role of 2DE in volumetric quantifications of cardiac chambers, and thereby cardiac function, has some limitations because, (a) the method depends upon geometric shape assumptions and (b) the presumably perpendicular planes obtained by 2DE are actually imperfectly perpendicular. These facts are especially important in patients with ischemic or non-ischemic LV dysfunctions that influence chamber geometry by remodeling, resulting in erroneous observations with poor reproducibility.9 Similar observations have been reported about LV mass quantification by 2DE.10
2DE based evaluations of LAV are even more likely to be fallacious as computed tomography based studies suggest that LA free wall has an irregular ellipsoid shape and inter-atrial septum is obliquely oriented.11
These factors are evidenced by reports of higher observer variability seen during evaluation of cardiac chamber volumes by 2DE compared to that seen with 3DE.12, 13 The accuracy of 3DE in determining cardiac volumes has been already validated against CMR14,15 and values obtained from 3DE have been found closer to CMR compared to those obtained from 2DE.16
4.2. LV parameters in indians compared to other populations
Investigators from western countries have reported larger LV volumes compared to our study; e.g. mean LVEDV values in Norwegian men and women were 136 ml and 104 ml respectively17 which are grossly larger than the values observed in our population i.e. 73.8 ml ± 15.8 and 64.0 ± 15.4 ml in men and women respectively. However, when indexed for BSA, the differences became less prominent as the LVEDVi reported by these authors were 66 ± 10 ml/m2 and 58 ± 8 ml/m2 in men and women; our comparable values were 42.9 ± 8.1 ml/m2 and 41.8 ± 8.8 ml/m2. Moreover, our parameters were closer to those reported in Japanese population wherein the observed LVEDVi was 50 ml/m2 ± 12 and 46 ml/m2 ± 9 in men and women respectively.3 Another similarly conducted study reported LVEDVi values of 55 ± 7 ml/m2 in men and 49 ± 6 ml/m2 in women18 but the age range of studied subjects was 1–88 years.
We also determined the cut-off values for higher limits of normal parameters and our data was very close to that observed in a study conducted in Europeans and Indian Asians living in London.19 They reported the upper limit of normal reference values (i.e. mean + 2SD) for LVEDVi as 59 ml/m2 and 55 ml/m2 in men and women respectively against our corresponding values of 59.19 ml/m2 in men and 59.61 ml/m2 in women. Similarly, their LVESVi values were 26 ml/m2 and 23 ml/m2 in men and women respectively, quite closely resembling our corresponding values of 23.27 ml/m2 and 23.11 ml/m2 for men and women respectively. The updated guidelines on recommendations for cardiac chamber quantification by echocardiography, published jointly by American Society of Echocardiography and European Association of Cardiovascular Imaging,20 have reported upper limits of normal LVEDVi as 79 ml/m2 and 71 ml/m2 (men and women respectively) and LVESVi as 32 ml/m2 and 28 ml/m2 (men and women respectively). They reported these values by taking weighted averages of the corresponding parameters observed from 3 studies.3, 17, 21 These values are higher than the corresponding values observed by us, which may be because, while reporting averaged LV parameters, the authors did not include data from the study29 that involved subjects of Indian descent also. However, the authors of guidelines have also recognized the need for a study involving diverse populations for establishing normal 3DE parameters.20
LVMi seen in our study was 68.83 g/m2 ± 13.53, quite comparable to 64 g/m2 ± 12 reported in Japanese population.3
4.3. Role of LA volume and function in cardiac diseases
Left atrial remodeling correlates with the severity and duration of the cardiac disease.22 2DE measured LA volume has been shown to predict adverse cardiac events.23 While earlier studies revealed that LAVi-max was a strong and independent predictor of mortality in heart failure patients,24 relatively recent data indicates stronger correlation between LAVi-min and cardiac events.25 Of all the volume indices derived using different echocardiographic methods, 3DE determined LAVi-min has shown strongest correlation with MACE.25 LAVi-min also correlates better with new onset atrial fibrillation compared to LAVi-max.26 In addition, 3D LAVi-min has also shown predictive value for cardiac death, not shown by LAVi-max.25 Biplane 2DE may be inaccurate in determining LA volume due to variability in LA shape and geometry. 3DE overcomes this issue and provides more accurate volumes.12 In addition to LA volumes, strong correlation has been seen between LAEF and sub-clinical cerebral infarcts.8 Although normal values of 3DE derived LAVi-min, LAVi-max and LAEF have been determined in other populations,25, 8 to our knowledge, this is the first study to assess these parameters in Indian population.
4.4. LA parameters in indians compared to other populations
On comparing LA parameters, the LAVi-max and LAVi-min in our study were 15.49 ml/m2 ± 4.4 and 7.81 ml/m2 ± 2.3, respectively which were smaller than those reported in other populations i.e. 23 ml/m2 ± 6 and 10 ml/m2 ± 3.3 These differences could be because of factors like coexisting diastolic dysfunction (seen in 25.6% of our subjects and not commented upon in the other study). The LAEF observed in our study was 48.99 ± 12.34, which was quite close to the value of 47.0% ± 11.9 seen in disease free subjects in another study.8 However, Japanese investigators reported LAEF of 58% ± 6 in normal population.3
4.5. Effect of age and gender on 3DE parameters
Our study revealed smaller LV volumes in women above 40 years’ age compared to younger adult women even after correction for BSA. Similar trends were not seen in men. Men had higher values of LV volumes and mass but differences either disappeared (LVEDV and LVM) or became less significant when the parameters were indexed for BSA. Women had higher LVEF. We did not find any gender dependency of LA volumes indexed for BSA; the same was observed by other investigators.25
5. Conclusions
Compared to other imaging modalities, 3DE has a stronger potential for faster and more accurate determinations of cardiac volumes, function,10 and mass.27 However, to include it into routine practice, it is necessary to know the reference values of normal parameters. One may argue that when CMR reference values are available for normal individuals, what is the need for 3DE values; however, it has to be realized that CMR assessed dimensions are reportedly larger than those obtained from 3DE, making it necessary to know the normal values for two imaging modalities independently so that the observations can be accurately interpreted. Variability in cardiac chamber dimensions as a function of race has been already reported5,28, 29, 30 and need for reference values for different races has been emphasized.31 There have been reports showing association of cardiac chamber dimensions with demographic and anthropometric variables.32
This study determined the 3DE volumes, mass and functions of left heart chambers in Indian adults free of cardiac disease and/or systemic hypertension, comparing the normative values for two age groups (18–39 years and ≥40 years), different anthropometrics as well as for male and female genders.
6. Limitations
Lack of validation of reference values against CMR seems to be a limitation of our study but cost and ethical issues related to conducting CMR in normal individuals are inhibitory and cannot be justified. Although, the sample size in our study was adequate as per the Clinical and Laboratory Standards Institute (CLSI) guidelines on establishing reference ranges for any population,33 the fact that Indian population is characterized by diversity, may require that the normative values be compared/confirmed in different ethnic groups in the country.
References
- 1.Juillière Y., Barbier G., Feldmann L. Additional predictive value of both left and right ventricular ejection fractions on long-term survival in idiopathic dilated cardiomyopathy. Eur Heart J. 1997;18:276–280. doi: 10.1093/oxfordjournals.eurheartj.a015231. [DOI] [PubMed] [Google Scholar]
- 2.Knauth A.L., Gauvreau K., Powell A.J. Ventricular size and function assessed by cardiac MRI predict major adverse clinical outcomes late after tetralogy of Fallot repair. Heart. 2008;94:211–216. doi: 10.1136/hrt.2006.104745. [DOI] [PubMed] [Google Scholar]
- 3.Fukuda S., Watanabe H., Daimon M. Normal values of real-time 3-dimensional echocardiographic parameters in a healthy Japanese population: the JAMP-3D Study. Circ J. 2012;76(5):1177–1181. doi: 10.1253/circj.cj-11-1256. [DOI] [PubMed] [Google Scholar]
- 4.Maffessanti F., Muraru D., Esposito R. Age-, body size-, and sex-specific reference values for right ventricular volumes and ejection fraction by three-dimensional echocardiography: a multicenter echocardiographic study in 507 healthy volunteers. Circ Cardiovasc Imaging. 2013;6(September (5)):700–710. doi: 10.1161/CIRCIMAGING.113.000706. [DOI] [PubMed] [Google Scholar]
- 5.Hinderliter A.L., Light K.C., Willis P.W., 4th Racial differences in left ventricular structure in healthy young adults. Am J Cardiol. 1992;69:1196–1199. doi: 10.1016/0002-9149(92)90935-r. [DOI] [PubMed] [Google Scholar]
- 6.Dubois D., Dubois E.F. A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med. 1916;17:863–871. [Google Scholar]
- 7.Macron Laurent, Lim Pascal, Bensaid Alexandre. Single-Beat Versus Multibeat Real-Time 3D Echocardiography for Assessing Left Ventricular Volumes and Ejection Fraction: A Comparison Study With Cardiac Magnetic Resonance. Circ Cardiovasc Imaging. 2010;3:450–455. doi: 10.1161/CIRCIMAGING.109.925966. [DOI] [PubMed] [Google Scholar]
- 8.Russo C., Jin Z., Liu R. LA volumes and reservoir function are associated with subclinical cerebrovascular disease: the CABL (Cardiovascular Abnormalities and Brain Lesions) study. JACC Cardiovasc Imaging. 2013;6:313–323. doi: 10.1016/j.jcmg.2012.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lang R.M., Bierig M., Devereux R.B. Recommendations for chamber quantification: a report from the American society of Echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European association of Echocardiography, a branch of the European society of cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Jenkins C., Bricknell K., Hanekom L. Reproducibility and accuracy of echocardiographic measurements of left ventricular parameters using real-time three-dimensional echocardiography. JAm Coll Cardiol. 2004;44:878–886. doi: 10.1016/j.jacc.2004.05.050. [DOI] [PubMed] [Google Scholar]
- 11.O’Brien J.P., Srichai M.B., Hecht E.M. Anatomy of the heart at multidetector CT: what the radiologist needs to know. Radiographics. 2007;27:1569–1582. doi: 10.1148/rg.276065747. [DOI] [PubMed] [Google Scholar]
- 12.Iwataki M., Takeuchi M., Otani K. Measurement of left atrial volume from transthoracic threedimensional echocardiographic datasets using the biplane Simpson’s technique. J Am Soc Echocardiogr. 2012;25:1319–1326. doi: 10.1016/j.echo.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 13.Miyasaka Y., Tsujimoto S., Maeba H. Left atrial volume by real-time three-dimensional echocardiography: validation by 64-slice multidetector computed tomography. J Am Soc Echocardiogr. 2011;24:680–686. doi: 10.1016/j.echo.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Shimada Y.J., Shiota M., Siegel R.J. Accuracy of right ventricular volumes and function determined by three-dimensional echocardiography in comparison with magnetic resonance imaging: a meta-analysis study. J Am Soc Echocardiogr. 2010;23:943–953. doi: 10.1016/j.echo.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 15.Mor-Avi V., Yodwut C., Jenkins C. Real-time 3D echocardiographic quantification of left atrial volume: multicenter study for validation with CMR. J Am Coll Cardiol Img. 2012;5:769–777. doi: 10.1016/j.jcmg.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 16.Jenkins C., Moir S., Chan J. Left ventricular volume measurement with echocardiography: a comparison of left ventricular opacification, threedimensional echocardiography, or both with magnetic resonance imaging. Eur Heart J. 2009;30:98–106. doi: 10.1093/eurheartj/ehn484. [DOI] [PubMed] [Google Scholar]
- 17.Aune E., Baekkevar M., Rodevand O. Reference values for left ventricular volumes with real-time 3-dimensional echocardiography. Scand Cardiovasc J. 2010;44:24–30. doi: 10.3109/14017430903114446. [DOI] [PubMed] [Google Scholar]
- 18.Kaku K., Takeuchi M., Otani K. Age- and gender-dependency of left ventricular geometry assessed with real-time three-dimensional transthoracic echocardiography. J Am Soc Echocardiogr. 2011;24:541–547. doi: 10.1016/j.echo.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 19.Chahal N.S., Lim T.K., Jain P. Population-based reference values for 3D echocardiographic LV volumes and ejection fraction. JACC Cardiovasc Imaging. 2012;5(December (12)):1191–1197. doi: 10.1016/j.jcmg.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 20.Lang R.M., Badano L.P., Mor-Avi V. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Muraru D., Badano L.P., Peluso D. Comprehensive analysis of left ventricular geometry and function by three-dimensional echocardiography in healthy adults. J Am Soc Echocardiogr. 2013;26:618–628. doi: 10.1016/j.echo.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 22.Abhayaratna W.P., Seward J.B., Appleton C.P. Left atrial size: physiologic determinants and clinical applications. J Am Coll Cardiol. 2006;47:2357–2363. doi: 10.1016/j.jacc.2006.02.048. [DOI] [PubMed] [Google Scholar]
- 23.Moller J.E., Hillis G.S., Oh J.K. Left atrial volume: a powerful predictor of survival after acute myocardial infarction. Circulation. 2003;107:2207–2212. doi: 10.1161/01.CIR.0000066318.21784.43. [DOI] [PubMed] [Google Scholar]
- 24.Lim T.K., Dwivedi G., Hayat S. Independent value of left atrial volume index for the prediction of mortality in patients with suspected heart failure referred from the community. Heart. 2009;95:1172–1178. doi: 10.1136/hrt.2008.151043. [DOI] [PubMed] [Google Scholar]
- 25.Wu V.C., Takeuchi M., Kuwaki H. Prognostic value of LA volumes assessed by transthoracic 3D echocardiography. JACC Cardiovasc Imaging. 2013 Oct;6(10):1025–1035. doi: 10.1016/j.jcmg.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Fatema K., Barnes M.E., Bailey K.R. Minimum vs: maximum left atrial volume for prediction of first atrial fibrillation or flutter in an elderly cohort: a prospective study. Eur J Cardiol. 2009;10:282–286. doi: 10.1093/ejechocard/jen235. [DOI] [PubMed] [Google Scholar]
- 27.Mor-Avi V., Sugeng L., Weinert L. Fast measurement of left ventricular mass with real-time threedimensional echocardiography: comparison with magnetic resonance imaging. Circulation. 2004;110:1814–1818. doi: 10.1161/01.CIR.0000142670.65971.5F. [DOI] [PubMed] [Google Scholar]
- 28.Harshfield G.A., Koelsch D.W., Pulliam D.A. Racial differences in the age-related increase in left ventricular mass in youths. Hypertension. 1994;24:747–751. doi: 10.1161/01.hyp.24.6.747. [DOI] [PubMed] [Google Scholar]
- 29.Schieken R.M., Schwartz P.F., Goble M.M. Tracking of left ventricular mass in children: race and sex comparisons: the MCV twin study: medical College of Virginia. Circulation. 1998;97:1901–1906. doi: 10.1161/01.cir.97.19.1901. [DOI] [PubMed] [Google Scholar]
- 30.Lang R.M., Badano L.P., Tsang W. EAE/ASE recommendations for image acquisition and display using three dimensional echocardiography. J Am Soc Echocardiogr. 2012;25:3–46. doi: 10.1016/j.echo.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 31.Chahal N.S., Lim T.K., Jain P. Ethnicity-related differences in left ventricular function, structure and geometry: a population study of UK Indian Asian and European white subjects. Heart. 2010;96:466 4–71. doi: 10.1136/hrt.2009.173153. [DOI] [PubMed] [Google Scholar]
- 32.D’Oronzio U., Senn O., Biaggi P. Right heart assessment by echocardiography: gender and body size matters. J Am Soc Echocardiogr. 2012;25:1251–1258. doi: 10.1016/j.echo.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 33.Horowitz Gary L., Altaie Sousan, Boyd James C. 3rd ed. CLSI; Wayne, PA: 2008. Defining, Establishing, and Verifying Reference Intervals in the Clinical Laboratory; Approved Guideline.https://clsi.org/media/1421/ep28a3c_sample.pdf [Google Scholar]