Abstract
Noise exposure modifies the function of multiple organs and systems. Acute noise exposure — both in laboratory settings where traffic noise is simulated and in real-life working environments — can cause increases in blood pressure, heart rate and cardiac output. This review examines the effects of noise pollution on the cardiovascular system, with a particular focus on non-auditory effects such as noise-induced arterial hypertension.
Keywords: Transportation noise, vascular function, hypertension
The health burden of environmental noise has recently been quantified in a report of the WHO in terms of disability-adjusted life years (DALYs; i.e., the number of years lost because of disability or death — a measure that combines both morbidity and mortality). The WHO estimates that — in western Europeans — each year 45,000 DALYs are lost because of noise-induced cognitive impairment in children, 903,000 because of noise-induced sleep disturbance, 61,000 because of noise-induced cardiovascular disease, and 22,000 because of tinnitus. Additionally, while not being a disease per se, noise-induced annoyance decreases quality-of-life and thus also causes disability, quantified as 654,000 DALYs lost in the western European population.[1]
Pathophysiology of Noise-induced Increases in Blood Pressure
According to the noise reaction scheme by Babisch, noise may induce damage through a direct pathway — for instance by causing hearing loss — and indirect pathways, reflecting disturbances of sleep, communication and daily activities, with or without noise-induced annoyance (see Figure 1).[2] Chronic annoyance causes stress characterised by increased levels of stress hormones such as cortisol and catecholamines. Chronic stress may in turn cause a number of pathophysiological adaptations, such as increased blood pressure, increases in heart rate and cardiac output, increases in blood lipids (cholesterol, triglycerides, free fatty acids, phosphatides) and carbohydrates (glucose) as well as the activation of blood coagulation.[3] This may ultimately manifest as cardiovascular diseases such as arterial hypertension, coronary artery disease and stroke (see Figure 1).
Figure 1: Simplified Scheme Showing Progress to Cardiovascular Diseases in Response to Noise-induced Stress Reactions.
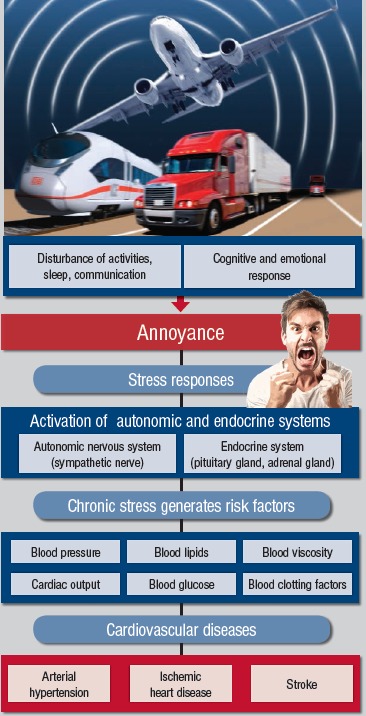
Source: Münzel, et al.[2], © 2014.Reproduced with permission of the author under Creative Commons.
Noise Affects Vascular Function
Two recently published field studies examined the effect of nocturnal aircraft noise exposure played-back with loudspeakers in subjects’ bedrooms. It was shown to dose-dependently affect parameters of vascular (endothelial) function in healthy subjects and in patients with established coronary artery disease, including endothelial function as measured by flow-dependent dilation of the brachial artery.[4,5]
Although these studies were limited to single-night exposures, a priming effect of noise was detected, i.e. the adverse effects of noise on vascular function were clearly more pronounced if the subject had previously been exposed to noise.[5] Thus, in response to repeated exposure, the vessel appears to be unable to develop a form of accommodation, and is somewhat sensitised to noise-induced vascular damage.[5] As expected, the deterioration in endothelial function was paralleled by increased catecholamine production and impaired sleep quality.[5] In subjects with established coronary artery disease, there was also a significant increase in blood pressure.[4] Interestingly, in these studies of patients with coronary artery disease, there was no correlation between annoyance reactions and the degree of deterioration of vascular function in response to noise, suggesting that noise per se adversely affects vascular function, whether the person is getting annoyed or not.[4]
Many epidemiological studies indicate that nocturnal noise exposure may be more relevant for cardiovascular health than daytime noise exposure. For aircraft noise, the Hypertension and Exposure to Noise near Airports (HYENA) study found no significant association for daytime noise, but a significant increase in blood pressure with increases in nighttime noise.[6] Furthermore, a recent Swiss study showed an adverse effect of railway noise on blood pressure, which was more strongly associated with nighttime exposure.[7] Compatible with this evidence, it has been demonstrated that road traffic noise exposure has a larger impact in those who sleep with open windows or whose bedroom faces the road.[8] A sustained decrease in blood pressure during the night (so-called ‘dipping’) seems to be important for resetting the cardiovascular system and for long-term cardiovascular health.[9] Repeated nocturnal autonomic arousals may prevent blood pressure dipping and contribute to the risk for developing hypertension in those exposed to relevant levels of environmental noise for prolonged periods of time.[10,11] In line with this, it has been reported that the risk of developing hypertension is higher in subjects sleeping with open windows during the night, whereas people sleeping in houses with sound insulation or where the bedroom does not face the main road have lower risk.[12]
The Night Noise Guidelines for Europe published by the WHO in 2009 constitute an expert consensus correlating four noise exposure ranges to negative health outcomes ranging from ‘no substantial biological effects’ to ‘increased risk of cardiovascular disease’.[13] The WHO considers average nocturnal noise levels of equivalent A-weighted noise outside (LAeq) of 55 dB as the interim goal when the recommended guideline value of 40 dB is not feasible in the short term for the prevention of noise-induced health effects.
In sum, nocturnal noise has been shown to affect both autonomic regulation, with increases in heart rate mediated by sympathetic activation and/or parasympathetic withdrawal[10,14,15] and with increases in blood pressure.[16] Furthermore, nocturnal noise has been shown to directly affect vascular function through the induction of endothelial dysfunction. Importantly, both endothelial dysfunction and reduced heart rate variability have been demonstrated to have prognostic value in patients with peripheral artery disease, arterial hypertension, and patients with an acute coronary syndrome or chronic stable coronary artery disease.[17–19] Taken together, these observations are compatible with the observation of an increased incidence of arterial hypertension and subsequent myocardial infarction and stroke in subjects with long-term exposure to relevant noise levels.
It should also be noted that residential exposure to road traffic noise correlates with exposure to ambient air pollution — another environmental pollutant suspected of increasing the risk for hypertension. The suggested pathophysiological pathway behind an effect of air pollution on cardiovascular disease shares some characteristics with the mechanisms proposed for noise, including effects on the immune system, endothelial dysfunction and changed levels of blood lipids.[20] It is possible, therefore, that these two environmental pollutants can act together to increase the risk for hypertension, which needs to be addressed in future studies.
Epidemiological Studies: Noise and Arterial Hypertension
Studies on chronic exposure to road traffic and/or railway or aircraft noise have reported a relationship with elevated blood pressure, arterial hypertension or the use of antihypertensive medications. These studies indicate that environmental noise may carry a considerable health burden with important medical and economic implications. A recent report from the European Environment Agency concluded that in Europe, more than 900,000 cases of hypertension are caused by environmental noise each year.[21]
Road Traffic Noise, Blood Pressure and Hypertension
A 2012 meta-analysis of 24 cross-sectional studies on the relationship between road traffic noise and the prevalence of hypertension among adults reported an OR of 1.07 (95 % CI [1.02–1.12]) per 10 dB increase in the 16-hours daytime average road traffic noise level (LAeq16h) in the range <50 to >75 dB.[22] A certain degree of heterogeneity among studies was detected with respect to age, gender, the way the exposure was assessed, the noise reference level used, and the duration of the exposure. For example, in the large HYENA study, road traffic noise was linked to hypertension in men but not women,[6] and in a Dutch study road traffic noise was significantly associated with hypertension only among people aged 45–55 years.[23] Later studies have confirmed the association between road traffic noise and prevalence of hypertension. A large Danish cohort study found a significantly higher systolic blood pressure per 10 dB increase in road traffic noise in middle-aged subjects, with stronger and significant associations in men and older subjects.[24] No associations were found between road traffic noise and diastolic blood pressure. Similarly, a Spanish cohort study also found road traffic noise to be associated with systolic blood pressure as well as prevalent hypertension.[25] In this study, exposure to nighttime noise was estimated outdoors as well as indoors, using information about the bedroom’s orientation and indoor insulation. As expected, indoor nighttime noise levels were more consistently associated with systolic blood pressure and hypertension when compared with the outdoor levels. A major concern in studies of road traffic noise is potential confounding from air pollution. In the Spanish study, exposure to especially indoor traffic noise was associated with systolic blood pressure and hypertension independently of estimated exposure to air pollution, probably reflecting that indoor levels of road traffic noise and air pollution are less correlated than outdoor levels.[25]
The association between transportation noise and blood pressure in children has also been investigated. A recent meta-analysis examined 13 studies comprising 8,770 children that addressed the relationship between road traffic noise and blood pressure in kindergarten and school children.[26] The authors reported that a 5 dB rise in road traffic noise at kindergarten/school was associated with a 0.48 mmHg higher systolic blood pressure (95 % CI [−0.87–1.83]) and a 0.22 mmHg higher diastolic blood pressure (95 % CI [−0.64–1.07]). However, there was high heterogeneity in the study, and further well-designed studies are needed to further assess this association.
All these studies, both in children and adults, are of cross-sectional design, which prevents conclusions on causality and chronological order of events. Only one study has addressed the association between road traffic and railway noise and hypertension using a longitudinal design.[24] This study found no association between long-term exposure to road traffic noise and risk of hypertension, whereas for railway noise the results indicated an association. However, this study was based on self-reported information on hypertension, which probably leads to underestimation of the actual number of subjects with hypertension, and longitudinal studies based on repeated blood pressure measurements are needed.
The effect of transportation noise on hypertension during pregnancy has also been examined. A recent Danish study found road traffic noise to be associated with hypertension among pregnant women.[27] Based on a birth cohort including almost 73,000 pregnant women with singleton pregnancies,[27] a 10 dB higher exposure to residential road traffic noise during the first trimester was associated with a higher risk of preeclampsia (OR 1.10; 95 % CI [1.02–1.18]) and pregnancy-induced hypertensive disorders (OR 1.08; 95 % CI [1.02–1.15]). Adjustment for air pollution lowered the estimates slightly (OR 1.08; 95 % CI [0.98–1.17] for preeclampsia and OR 1.06; 95 % CI [0.98–1.14] for all subtypes of hypertensive disorders during pregnancy). The results are comparable with results from a small Lithuanian study of approximately 3,000 women, which reported a non-significant association between road traffic noise and gestational hypertension.[28] Although these two studies indicate that transportation noise may be a risk factor for hypertension during pregnancy, more studies addressing this end-point are warranted.
Aircraft Noise and Arterial Hypertension
An increased prevalence of arterial hypertension in the vicinity of Stockholm airport was reported in 2001.[29] With respect to the early stages of hypertension, a time-series study in the area surrounding Frankfurt Airport showed that, even in the physiological blood pressure range, a relationship existed between aircraft noise and early-morning blood pressure.[30] In this study, two groups exposed to nighttime outdoor aircraft noise of 50 dB(A) were followed over a period of three months. The ‘western group’ were exposed for 75 % of the time, and the ‘eastern group’ for 25 % of the time. The evaluation of ∼8,000 blood pressure measurements from 53 individuals showed a statistically significant 10 mmHg higher morning systolic blood pressure and an 8 mmHg higher diastolic blood pressure for the western group compared with the less exposed eastern group.
One of the largest and most comprehensive studies on aircraft noise and hypertension is the HYENA study, based on almost 5,000 participants from six European countries.[6] In this study, an exposure-response relationship was found, showing that for every 10 dB increase in nighttime aircraft noise (Lnight) the prevalence of hypertension increased by 14 % (95 % CI [1.01–1.29]; p=0.031). In contrast, no effect was found for daytime aircraft noise exposure (LAeq: OR 0.93; 95 % CI [0.83–1.04]; p=0.19). Results from the HYENA study also suggest an effect of aircraft noise on the use of antihypertensive medication, but this effect did not hold for all participating study centers.[31]
Data from the European Union-funded Road Traffic and Aircraft Noise Exposure and Children’s Cognition and Health study reported an association between both daytime and nocturnal noise exposure at home and blood pressure values in children aged 9–10 years living near Schiphol (Amsterdam) or Heathrow (London).[32] A 2009 meta-analysis of four cross-sectional studies and one cohort study on the relationship between aircraft traffic noise and the prevalence of hypertension reported an OR of 1.13 (95 % CI [1.00–1.28]; p<0.001) per 10 dB increase of the day-night weighted noise level (LDEN) in the range <55 to >65 dB.[33] This picture has been confirmed in later studies, such as a recent French study that found that 10 dB higher nighttime aircraft noise was associated with a 34 % higher prevalence of hypertension in men (95 % CI [1.00–1.97]).[34]
Only one study has investigated the association between aircraft noise and hypertension using a longitudinal approach.[35] This study is based on a cohort of almost 5,000 participants with repeated blood pressure measurements and living around Stockholm Arlanda airport. The authors reported that a 5 dB increase in long-term exposure to aircraft noise was associated with an 8 % increased risk for developing hypertension among men. After exclusion of the ∼30 % that smoked or used snuff during or directly preceding the blood pressure measurements, this estimate increased to 21 % per 5 dB (95 % CI [1.05–1.39]). In contrast, the study indicated no association between aircraft noise and hypertension among women. The study, however, included only few subjects exposed to high levels of aircraft noise (≥60 dB), and larger prospective studies are needed in this area.
Conclusion
The existing literature of both mechanistic and epidemiological design strongly points towards a relationship between exposure to transportation noise and elevated blood pressure. The consequence is that noise per se as an environmental stressor should be considered as a novel cardiovascular risk factor. This calls for prevention strategies, as around one third of the European population is exposed to transportation levels exceeding 55 dB; a number that is rising.[21]
References
- 1.World Health Organization. Burden of disease from environmental noise. http://www.euro.who.int/__data/assets/pdf_file/0008/136466/e94888.pdf Available at: (accessed 22 January 2017)
- 2.Münzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. Eur Heart J. 2014;35:829–36. doi: 10.1093/eurheartj/ehu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lundberg U. Coping with stress: Neuroendocrine reactions and implications for health. Noise Health. 1999;1:67–74. [PubMed] [Google Scholar]
- 4.Schmidt F, Kolle K, Kreuder K et al. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin Res Cardiol. 2015;104:23–30. doi: 10.1007/s00392-014-0751-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmidt FP, Basner M, Kroger G et al. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur Heart J. 2013;34:3508–14a. doi: 10.1093/eurheartj/eht269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jarup L, Babisch W, Houthuijs D et al. HYENA Study Team. Hypertension and exposure to noise near airports: The HYENA study. Environ Health Perspect. 2008;116:329–33. doi: 10.1289/ehp.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dratva J, Phuleria HC, Foraster M et al. Transportation noise and blood pressure in a population-based sample of adults. Environ Health Perspect. 2011;120:50–5. doi: 10.1289/ehp.1103448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Babisch W, Ising H, Gallacher JEJ et al. Traffic noise and cardiovascular risk: The Caerphilly and Speedwell studies, third phase-10-year follow up. Arch Environ Health. 1999;54:210–6. doi: 10.1080/00039899909602261. [DOI] [PubMed] [Google Scholar]
- 9.Sayk F, Becker C, Teckentrup C et al. To dip or not to dip: On the physiology of blood pressure decrease during nocturnal sleep in healthy humans. Hypertension. 2007;49:1070–6. doi: 10.1161/HYPERTENSIONAHA.106.084343. [DOI] [PubMed] [Google Scholar]
- 10.Haralabidis AS, Dimakopoulou K, Vigna-Taglianti F et al. HYENA Consortium. Acute effects of night-time noise exposure on blood pressure in populations living near airports. Eur Heart J. 2008;29:658–64. doi: 10.1093/eurheartj/ehn013. [DOI] [PubMed] [Google Scholar]
- 11.Carrington MJ, Trinder J. Blood pressure and heart rate during continuous experimental sleep fragmentation in healthy adults. Sleep. 2008;31:1701–12. doi: 10.1093/sleep/31.12.1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lercher P, Widmann U, Kofler W. Transportation noise and blood pressure: The importance of modifying factors. Presented at the 29th International Congress and Exhibition on Noise Control Engineering, Nice, France, 27–30 August, 2000.
- 13.World Health Organization. Night noise guidelines for Europe. 2009. http://www.euro.who.int/__data/assets/pdf_file/0017/43316/E92845.pdf Available at: (accessed 7 December 2016)
- 14.Lusk SL, Gillespie B, Hagerty BM, Ziemba RA. Acute effects of noise on blood pressure and heart rate. Arch Environ Health. 2004;59:392–9. doi: 10.3200/AEOH.59.8.392-399. [DOI] [PubMed] [Google Scholar]
- 15.Björ B, Burström L, Karlsson M et al. Acute effects on heart rate variability when exposed to hand transmitted vibration and noise. Int Arch Occup Environ Health. 2007;81:193–9. doi: 10.1007/s00420-007-0205-0. [DOI] [PubMed] [Google Scholar]
- 16.Chang TY, Lai YA, Hsieh HH et al. Effects of environmental noise exposure on ambulatory blood pressure in young adults. Environ Res. 2009;109:900–5. doi: 10.1016/j.envres.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 17.Münzel T, Sinning C, Post F et al. Pathophysiology, diagnosis and prognostic implications of endothelial dysfunction. Ann Med. 2008;40:180–96. doi: 10.1080/07853890701854702. [DOI] [PubMed] [Google Scholar]
- 18.Muxel S, Fasola F, Radmacher MC et al. Endothelial functions: Translating theory into clinical application. Clin Hemorheol Microcirc. 2010;45:109–15. doi: 10.3233/CH-2010-1288. [DOI] [PubMed] [Google Scholar]
- 19.Buccelletti E, Gilardi E, Scaini E et al. Heart rate variability and myocardial infarction: Systematic literature review and metanalysis. Eur Rev Med Pharmacol Sci. 2009;13:299–307. [PubMed] [Google Scholar]
- 20.Münzel T, Sørensen M, Gori T Environmental stressors and cardio-metabolic disease: Part II-mechanistic insights. Eur Heart J. 2016. epub ahead of press. [DOI] [PMC free article] [PubMed]
- 21.European Environment Agency. Noise in Europe 2014. 2014. www.eea.europa.eu/publications/noise-ineurope-2014 Available at: (accessed 7 December 2016)
- 22.van Kempen E, Babisch W. The quantitative relationship between road traffic noise and hypertension: A metaanalysis. J Hypertens. 2012;30:1075–86. doi: 10.1097/HJH.0b013e328352ac54. [DOI] [PubMed] [Google Scholar]
- 23.de Kluizenaar Y, Gansevoort RT, Miedema HM, de Jong PE. Hypertension and road traffic noise exposure. J Occup Environ Med. 2007;49:484–92. doi: 10.1097/JOM.0b013e318058a9ff. [DOI] [PubMed] [Google Scholar]
- 24.Sørensen M, Hvidberg M, Hoffmann B et al. Exposure to road traffic and railway noise and associations with blood pressure and self-reported hypertension: A cohort study. Environ Health. 2011;10:92. doi: 10.1186/1476-069X-10-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foraster M, Kunzli N, Aguilera I et al. High blood pressure and long-term exposure to indoor noise and air pollution from road traffic. Environ Health Perspect. 2014;122:1193–200. doi: 10.1289/ehp.1307156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dzhambov AM, Dimitrova DD. Children’s blood pressure and its association with road traffic noise exposure -A systematic review with meta-analysis. Environ Res. 2017;152:244–55. doi: 10.1016/j.envres.2016.10.024. [DOI] [PubMed] [Google Scholar]
- 27.Pedersen M, Halldorsson TI, Olsen SF et al. Impact of road traffic pollution on pre-eclampsia and pregnancyinduced hypertensive disorders. Epidemiology. 2017;28:99–106. doi: 10.1097/EDE.0000000000000555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bendokiene I, Grazuleviciene R, Dedele A. Risk of hypertension related to road traffic noise among reproductive-age women. Noise Health. 2011;13:371–7. doi: 10.4103/1463-1741.90288. [DOI] [PubMed] [Google Scholar]
- 29.Rosenlund M, Berglind N, Pershagen G et al. Increased prevalence of hypertension in a population exposed to aircraft noise. Occup Environ Med. 2001;58:769–73. doi: 10.1136/oem.58.12.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aydin Y, Kaltenbach M. Noise perception, heart rate and blood pressure in relation to aircraft noise in the vicinity of the Frankfurt airport. Clin Res Cardiol. 2007;96:347–58. doi: 10.1007/s00392-007-0507-y. [DOI] [PubMed] [Google Scholar]
- 31.Floud S, Vigna-Taglianti F, Hansell A et al. HYENA Study Team. Medication use in relation to noise from aircraft and road traffic in six European countries: Results of the HYENA study. Occup Environ Med. 2011;68:518–24. doi: 10.1136/oem.2010.058586. [DOI] [PubMed] [Google Scholar]
- 32.van Kempen E, van Kamp I, Fischer P et al. Noise exposure and children’s blood pressure and heart rate: The RANCH project. Occup Environ Med. 2006;63:632–9. doi: 10.1136/oem.2006.026831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Babisch W, Kamp I. Exposure-response relationship of the association between aircraft noise and the risk of hypertension. Noise Health. 2009;11:161–68. doi: 10.4103/1463-1741.53363. [DOI] [PubMed] [Google Scholar]
- 34.Evrard AS, Lefevre M, Champelovier P Does aircraft noise exposure increase the risk of hypertension in the population living near airports in France? Occup Environ Med. 2016. [DOI] [PubMed]
- 35.Eriksson C, Bluhm G, Hilding A et al. Aircraft noise and incidence of hypertension-gender specific effects. Environ Res. 2010;110:764–72. doi: 10.1016/j.envres.2010.09.001. [DOI] [PubMed] [Google Scholar]


