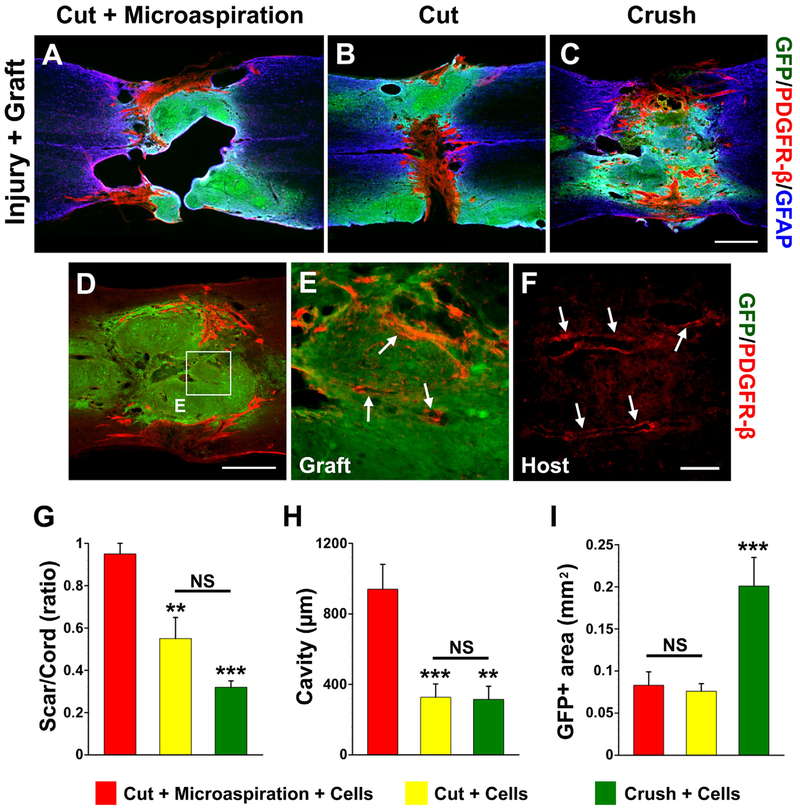
Fig. 3.
Scarring, cavitation and cell survival after embryonic BS-NSC transplanting. Eight weeks after cellular transplantation into the lesion site, a PDGFR-β-labeled fibrotic scar rift and large cavities separate GFP+ grafts in cords receiving (A) cut + microaspiration. In contrast, the graft in cords treated with (B) cut only or (C) crush forms a neural tissue bridge across the non-neural scar. Interestingly, some PDGFR-β-labeled fibroblasts are associated with (D, E) vessel-like structures (arrows) within GFP+ grafts, which are similar to (F) labeled real blood vessels (arrows) in the host tissue of same section. E is higher magnification of boxed region in D. Statistical analysis shows that the sizes of (G) fibrotic scars or cavities (H) are significantly larger in rats receiving cut + microaspiration than other two groups. Furthermore, quantification of the size of graft demonstrates that a larger GFP+ area in cords receiving crush injury compared to other two groups (I), indicating better survival of grafts in this injury model. (one-way ANOVA followed by LSD post hoc, **p < 0.01, ***p < 0.001, NS p > 0.05). Scale bars: C, 0.5 mm; D, 100 μm; F, 70 μm.