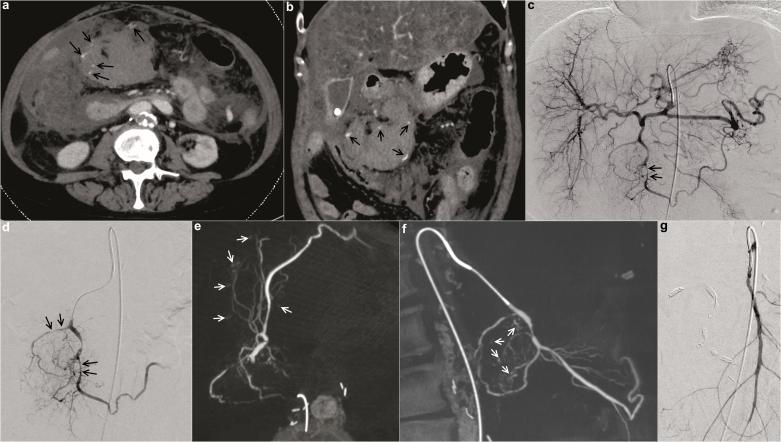
Figure 2.
Images of a hemodynamically unstable 63-year-old female patient with history of liver cirrhosis who presented with acute pancreatitis, hepatic failure and clinical concern for acute GI bleeding. In the emergency department, the patient had a decrease in haemoglobin of 2.4 mg dl−1 within 150 min. Pre-interventional CTA (a, b) demonstrated multiple bleeding sites (marked with arrows) suspected to originate from different feeding vessels of the celiac trunk and superior mesenteric artery. Selective angiograms [of the celiac trunk (c) and the proximal gastroduodenal artery (d)] could not clearly delineate the bleeding source. Gross vasospasm of gastroduodenal artery branches (marked with arrows) was seen. CBCT from the same catheter position as in (d) was performed. CBCT revealed all sites of active haemorrhage of the gastroduodenal artery branches precisely and involvement of the superior mesenteric artery could be excluded [axial (e) and sagittal MIP reconstructions (f); bleeding sites marked by arrows]. Selective and super-selective angiography of the superior mesenteric artery confirmed lack of involvement (g). The patient was treated successfully with super-selective pushable coil embolization of the major bleeding sites and coil embolization of the proximal gastroduodenal artery. CBCT, cone beam CT; CTA, CT angiography; GI, gastrointestinal.