TO THE EDITOR:
GATA2 encodes a zinc-finger transcription factor that is required for proliferation and survival of hematopoietic stem cells.1 First described in 2011, germline heterozygous mutations in GATA2 lead to haploinsufficiency2 and are associated with bone marrow failure, immunodeficiency, lymphedema, and other organ dysfunction, with a high propensity for transformation to myelodysplastic syndrome (MDS)/acute myeloid leukemia (AML).3-8 Multigenerational family cohorts demonstrate that age of disease presentation, phenotypic manifestations, and progression are highly variable,9-12 which may hinder recognition of familial disease. The overall lifetime risk of developing MDS/AML in GATA2 deficiency is estimated at 75% to 90%,13,14 with a median age of onset of 20 years. The prevalence of germline GATA2 mutations varies from 3.9% of inherited bone marrow failure15 to 15% of pediatric/adolescent MDS, and 72% of adolescent MDS with monosomy 7.13,16 Hematopoietic stem cell transplantation (HSCT) offers the only cure for MDS/AML and reconstitution of the immune system.17,18
Related mutation-positive donors, with or without a clinical phenotype, should be avoided. For the first time, we describe 3 families with germline GATA2 mutations (Table 1), in which 1 member was transplanted using a mutation-positive healthy related donor resulting in donor-derived posttransplant MDS/AML, recurrent MDS/AML, or fatal infection due to impaired immune reconstitution.
Table 1.
Patients with MDS/AML and germline GATA2 mutation who underwent HSCT from a healthy mutation-positive related donor
| Family/Patient | 1 | 2 | 3A | 3B |
|---|---|---|---|---|
| Age | 21 | 13 | 15 | 18 |
| Gender | M | M | F | F |
| Recipient | ||||
| Family history | ||||
| At presentation | Negative | Negative | Positive | |
| Other family members | Mother, healthy | Two older siblings, healthy; twin brother, healthy at donation, subsequently developed MDS-EB | Father, died with dx of AA at 41 y; 1 female sibling died at 2 mo of age due to sepsis; 3 male siblings were dxed with MDS/AML at ages 27, 29, and 51 | |
| GATA2 mutation | ||||
| Genomic | c.1061C>T | c.1082G>A | c.1018-50_1143+247del | |
| Protein | p.T354M | p.R361H | p.340_381del | |
| Pre-HSCT | ||||
| Clinical features | Pancytopenia | Weakness, epistaxis | Weakness | Weakness, pancytopenia |
| Infection | None | Warts | Multiple | None |
| Bone marrow | AML-MRC | MDS-EB | MDS | MDS |
| Cytogenetics | 45,XY, −7[5]/47,XY,+13 [5]/46,XY[8] | 45,XY,−7[18]/46, idem,+mar [1]/45,XY,−14[1] | Unknown | 46, XX, −18, +22 [3]/48, XX, +22, +mar[13] |
| Molecular | NRAS mutation (c.182A>G, p.Q61R) | Unknown | Unknown | Unknown |
| Post-HSCT | ||||
| Donor | Mother | Monozygotic twin | Brother | |
| Time post-HSCT | 3 y | 140 d | 30 d | 121 d |
| Bone marrow | MDS | Recurrent MDS/AML | Not done | Hypocellular |
| Chimerism | 100% donor | Not done | Unknown | 100% donor |
| Cytogenetics | 45,XX,−7[20] | 45,XY, −7[6] ;45,idem, t(6;20)(q15;p13)[2] | Unknown | Unknown |
| Molecular | SETBP1 mutation (c.2608G>A, p.G870S) | Unknown | Unknown | Unknown |
| Cause of death | Not applicable | Recurrent MDS/AML | Candida sepsis | CMV & fungal pneumonia |
| Donor | ||||
| After donating HSC | ||||
| Age at donation | 64 | 13 | 9 | 11 |
| Age of MDS/AML presentation | Healthy to date | 31 | 29 | |
| Clinical features | Healthy to date | Pancytopenia & lung infiltrates | Cytopenias and pneumonia | |
| Infection | None | Disseminated warts | Disseminated MAC | |
| Bone marrow | Not done | MDS-EB | MDS with transformation to AML | |
| Cytogenetics | Not done | 46,XY | 47,XY,del(7)(q22q32),+8[5]/47,XY,+8,der(11)t(1;11)(q21;q21)[2] | |
| Molecular | Unknown | STAG2 mutation (c.993T>A, p.Y331termination) | Unknown | Unknown |
| Outcome | Healthy | Died of sepsis prior to MUD HSCT | Died post-MUD HSCT due to MAC infection, GVHD, sepsis | |
CMV, cytomegalovirus; Dx, diagnosis; Dxed, diagnosed; F, female; GVHD, graft-versus-host-disease; M, male; MAC, Mycobacterium avium complex; MDS-EB, MDS with excess blasts; MUD, matched unrelated.
The proband of the first family presented with malaise, fatigue, and pancytopenia at 21 years of age. His family history was negative for known hematological or immunodeficiency disorders. The bone marrow revealed AML with MDS-related changes (Figure 1A) and monosomy 7 and trisomy 13 on cytogenetic analysis. An NRAS mutation (c.182A>G, p.Q61R) was also detected. Remission was induced with daunorubicin and cytarabine followed by consolidation with high-dose cytarabine. He underwent haploidentical allogeneic HSCT in August 2014, using his healthy 64-year-old mother as a donor after fludarabine, cyclophosphamide, and total body irradiation (TBI) on BMT CTN trial 1101. Post-HSCT studies revealed complete engraftment with 100% donor chimerism. Cytogenetic studies of marrow 1-year posttransplant revealed a female karyotype with trisomy 8 (47,XX,+8[3]/46,XX[20]). Two years after HSCT, he developed neutropenia, and cytogenetic studies revealed the donor karyotype with trisomy 8 and monosomy 7. Molecular sequencing panel identified a germline GATA2 mutation (c.1061C>T; p.T354M) in both the parent donor and the recipient. Three years after HSCT, the marrow showed dysplastic changes (Figure 1A) with monosomy 7 in all donor metaphases (45,XX,−7[20]), indicative of donor-derived MDS. Targeted sequencing analysis identified a mutation in SETBP1 (c.2608G>A, p.G870S) with variant allele frequency (VAF) of 44.5% (see supplemental Methods, available on the Blood Web site). The mother is alive and continues to be asymptomatic.
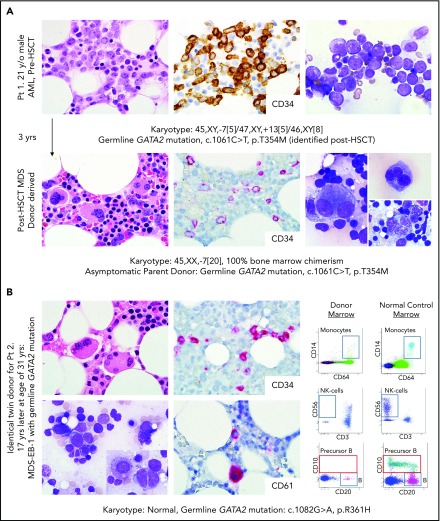
Figure 1.
Donor-derived MDS/AML with germline GATA2 mutation in recipient from Family 1, and MDS/AML in matched related donor from Family 2. (A) Donor-derived MDS/AML after HSCT in patient with germline GATA2 mutation transplanted with healthy parent harboring same mutation. Upper panel shows pre-HSCT bone marrow of 21-year-old man diagnosed with AML (patient 1). The bone marrow is hypocellular for age with numerous blasts (upper left image of core biopsy; original magnification ×500; hematoxylin and eosin [H&E] stain) that are positive for CD34 by immunohistochemistry (IHC; brown stained cells, upper middle image; original magnification ×500). The blasts are large with a high nuclear to cytoplasmic ratio and fine chromatin shown on the marrow aspirate (upper right image; original magnification ×1000; Wright-Giemsa stain). Cytogenetic analysis revealed an abnormal karyotype involving monosomy 7 and trisomy 13. Lower panel shows bone marrow 3 years after HSCT when the patient peripheral blood counts were falling. Abnormal dysplastic megakaryocytes are seen (lower left image; original magnification ×500; H&E core biopsy) in a hypocellular marrow for age. CD34-positive blasts are increased (5% to 9%) by IHC (red stained cells in lower middle image; original magnification ×500). Aspirate smear shows dysplastic megakaryocytes, multinucleated erythroid precursors, and abnormal dysplastic cells (composite lower right image; original magnification ×1000). Cytogenetic analysis revealed presence of monosomy 7 in all of the female donor cells, consistent with donor-derived MDS/AML. Germline GATA2 mutation was identified in both the mother donor and the recipient son after HSCT. (B) MDS/AML with germline GATA2 mutation in identical twin MRD. Images of the bone marrow of the identical twin MRD for patient 2. At the time of HSCT, the donor was healthy with normal peripheral blood counts. Patient 2 died several months after HSCT of AML, and MDS developed in the identical twin donor 17 years later. Images of bone marrow show dysplastic megakaryocytes (upper left image of core biopsy; original magnification ×500; H&E stain) and increased CD34-positive blasts (red cells, IHC for CD34, upper middle image; original magnification ×500). IHC for CD61 highlights presence of micromegakaryocytes (small red cell, lower middle image; original magnification ×500). Aspirate shows scattered blasts and dysplastic binucleated precursor (inset) (lower left image of aspirate; original magnification ×1000; Wright-Giemsa stain). Flow cytometry analysis of the bone marrow of the patient in comparison with normal control marrow (right panels) revealed underlying immunodeficiency characterized by severe decrease to absence of monocytes, natural killer cells, precursor B cells, and mature B cells in the bone marrow. EB-1, excess blasts 1.
The index patient of the second family presented at age 13 with MDS-EB with monosomy 7. He had a history of warts. The family history was negative for hematologic/immunodeficiency disorders. Two older siblings and his identical twin brother were healthy. The white blood cell count was 8.1 × 109/L with 5% circulating blasts. Severe anemia (6.5 g/dL) and thrombocytopenia (14 × 109/L) were present. He underwent syngeneic HSCT from his healthy monozygotic twin brother after cyclophosphamide, cytarabine, and TBI in March 1995. There was reemergence of MDS-EB with monosomy 7 and additional t(6;20)(q15;p13) on day +140. The patient died, and autopsy revealed leukemic blasts infiltrating the spleen, lungs, and liver. Seventeen years later, at age 31, the identical twin donor presented with pancytopenia, disseminated warts, and lung infiltrates. His marrow showed hypocellular MDS with features commonly seen in GATA2 deficiency,7,19 including dysplastic megakaryocytes, and loss of monocytes, B cells, B-cell precursors, and natural killer cells (Figure 1B). A germline GATA2 mutation (c.1082G>A; p.R361H) was identified along with mutation in STAG2 (c.993T>A, p.Y331Termination; VAF 26.4%). He progressed to MDS-EB with neutropenia and expired prior to HSCT due to sepsis in 2013.
The third family has numerous members with blood disorders over multiple generations and was previously reported in 1978.20 The father of the proband was diagnosed with aplastic anemia (AA) and lymphedema at age 30 and died at 41.20 Four of the 7 children were diagnosed in adolescence or young adulthood with “MDS vs AA,” with transformation to high-grade MDS or AML. Two female siblings underwent matched related donor (MRD) HSCT for MDS using the same healthy male sibling donor. The first sister presented at age 15 with multiple infections. She died 30 days after HSCT (performed in 1988) secondary to fatal disseminated fungal infection. The second sister presented with pancytopenia. Her initial bone marrow revealed MDS with monosomy 18 and trisomy 22. She underwent MRD HSCT after TBI in April 1991. The posttransplant evaluation revealed 100% donor chimerism. Her post-HSCT course was complicated by persistent neutropenia, GVHD, and fatal CMV infection. Twenty years later, the male sibling donor presented with disseminated MAC, and MDS/AML with trisomy 8 and deletion 7q. He died following MUD HSCT secondary to disseminated MAC infection, GVHD, sepsis, and multiorgan failure. One decade later, a remaining male sibling (proband) presented with chronic neutropenia, numerous warts, recurrent infections, and bilateral lymphedema at 51 years of age. Marrow analysis showed MDS with multilineage dysplasia with trisomy 8, and immunodeficiency with absence of monocytes, dendritic cells, B-cell precursors, and B lymphopenia. Initial genetic sequencing was negative; however, subsequent in-depth analysis revealed a large novel germline GATA2 deletion (c.1018-50_1143+247del; p.340_381del), and targeted sequencing identified a STAG2 mutation (1810C>T, p. R604Termination; VAF 53.9%). The patient underwent successful MUD-HSCT in 2017 with restoration of normal hematopoiesis and immune reconstitution.
The experiences of these 3 families underscore the importance of considering germline mutations in GATA2 in pediatric/adolescent and young adult patients diagnosed with MDS/AML regardless of family history or phenotypic manifestations. For this reason, we recommend that all pediatric, adolescent, and young adults diagnosed with MDS/AML be screened for germline mutations in GATA2 and other genes predisposing to MDS/AML, particularly if there is consideration of using a related donor for HSCT. All healthy potential related donors should be tested for the patient’s mutation prior to HSCT21 to avoid donor-derived MDS/AML, failed engraftment, or failed immune reconstitution after HSCT. Similar poor outcomes have also been reported in families with germline predisposition to MDS/AML and mutations in CEBPA,22 RUNX1,23 and DDX4124
Supplementary Material
The online version of this article contains a data supplement.
Acknowledgments
This research project has been funded in whole or in part with federal funds from the National Institutes of Health (NIH), National Cancer Institute under Contract no. HHSN261200800001E, and by the Intramural Research Program of the NIH Clinical Center, National Institute of Allergy and Infectious Diseases, National Cancer Institute, and National Heart, Lung, and Blood Institute.
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government.
Authorship
Contribution: K.R.C., D.D.H., and S.M.H. designed the study; A.P.H., S.D., W.W., and R.C. did GATA2 and/or targeted sequencing studies; P.G., W.W., S.D., J.M.K., J.R.S., L.M., C.Z., M.J.P., N.S.Y., and S.A. acquired clinical/laboratory data and/or provided patient samples; K.R.C., P.G., J.R.S., and J.M.K. reviewed bone marrow pathology; K.R.C. and P.G. analyzed data, wrote the paper, and made the figure and table; and all authors reviewed the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Katherine R. Calvo, Hematology Section, Department of Laboratory Medicine, Clinical, Center, National Institutes of Health, 10 Center Dr, Building 10, Room 2C306, Bethesda, MD 20892-1508; e-mail: katherine.calvo@nih.gov.
REFERENCES
- 1.Tsai FY, Orkin SH. Transcription factor GATA-2 is required for proliferation/survival of early hematopoietic cells and mast cell formation, but not for erythroid and myeloid terminal differentiation. Blood. 1997;89(10):3636-3643. [PubMed] [Google Scholar]
- 2.Hsu AP, Johnson KD, Falcone EL, et al. . GATA2 haploinsufficiency caused by mutations in a conserved intronic element leads to MonoMAC syndrome. Blood. 2013;121(19):3830-3837, S1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsu AP, Sampaio EP, Khan J, et al. . Mutations in GATA2 are associated with the autosomal dominant and sporadic monocytopenia and mycobacterial infection (MonoMAC) syndrome. Blood. 2011;118(10):2653-2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dickinson RE, Griffin H, Bigley V, et al. . Exome sequencing identifies GATA-2 mutation as the cause of dendritic cell, monocyte, B and NK lymphoid deficiency. Blood. 2011;118(10):2656-2658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hahn CN, Chong CE, Carmichael CL, et al. . Heritable GATA2 mutations associated with familial myelodysplastic syndrome and acute myeloid leukemia. Nat Genet. 2011;43(10):1012-1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ostergaard P, Simpson MA, Connell FC, et al. . Mutations in GATA2 cause primary lymphedema associated with a predisposition to acute myeloid leukemia (Emberger syndrome). Nat Genet. 2011;43(10):929-931. [DOI] [PubMed] [Google Scholar]
- 7.Ganapathi KA, Townsley DM, Hsu AP, et al. . GATA2 deficiency-associated bone marrow disorder differs from idiopathic aplastic anemia. Blood. 2015;125(1):56-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pasquet M, Bellanné-Chantelot C, Tavitian S, et al. . High frequency of GATA2 mutations in patients with mild chronic neutropenia evolving to MonoMac syndrome, myelodysplasia, and acute myeloid leukemia. Blood. 2013;121(5):822-829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsu AP, McReynolds LJ, Holland SM. GATA2 deficiency. Curr Opin Allergy Clin Immunol. 2015;15(1):104-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dickinson RE, Milne P, Jardine L, et al. . The evolution of cellular deficiency in GATA2 mutation. Blood. 2014;123(6):863-874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al Seraihi AF, Rio-Machin A, Tawana K, et al. . GATA2 monoallelic expression underlies reduced penetrance in inherited GATA2-mutated MDS/AML [published online ahead of print 19 April 2018]. Leukemia. 2018.doi:10.1038/s41375-018-0134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spinner MA, Sanchez LA, Hsu AP, et al. . GATA2 deficiency: a protean disorder of hematopoiesis, lymphatics, and immunity. Blood. 2014;123(6):809-821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wlodarski MW, Collin M, Horwitz MS. GATA2 deficiency and related myeloid neoplasms. Semin Hematol. 2017;54(2):81-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Collin M, Dickinson R, Bigley V. Haematopoietic and immune defects associated with GATA2 mutation. Br J Haematol. 2015;169(2):173-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bluteau O, Sebert M, Leblanc T, et al. . A landscape of germ line mutations in a cohort of inherited bone marrow failure patients. Blood. 2018;131(7):717-732. [DOI] [PubMed] [Google Scholar]
- 16.Wlodarski MW, Hirabayashi S, Pastor V, et al. ; EWOG-MDS. Prevalence, clinical characteristics, and prognosis of GATA2-related myelodysplastic syndromes in children and adolescents. Blood. 2016;127(11):1387-1397, quiz 1518. [DOI] [PubMed] [Google Scholar]
- 17.Parta M, Shah NN, Baird K, et al. . Allogeneic hematopoietic stem cell transplantation for GATA2 deficiency using a busulfan-based regimen. Biol Blood Marrow Transplant. 2018;24(6):1250-1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tholouli E, Sturgess K, Dickinson RE, et al. . In vivo T-depleted reduced-intensity transplantation for GATA2-related immune dysfunction. Blood. 2018;131(12):1383-1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calvo KR, Vinh DC, Maric I, et al. . Myelodysplasia in autosomal dominant and sporadic monocytopenia immunodeficiency syndrome: diagnostic features and clinical implications. Haematologica. 2011;96(8):1221-1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Branda RFMC, Moldow CF, MacArthur JR, Wintrobe MM, Anthony BK, Jacob HS. Folate-induced remission in aplastic anemia with familial defect of cellular folate uptake. N Engl J Med. 1978;298(9):469-475. [DOI] [PubMed] [Google Scholar]
- 21.Godley LA, Shimamura A. Genetic predisposition to hematologic malignancies: management and surveillance. Blood. 2017;130(4):424-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xiao H, Shi J, Luo Y, et al. . First report of multiple CEBPA mutations contributing to donor origin of leukemia relapse after allogeneic hematopoietic stem cell transplantation. Blood. 2011;117(19):5257-5260. [DOI] [PubMed] [Google Scholar]
- 23.Owen CJ, Toze CL, Koochin A, et al. . Five new pedigrees with inherited RUNX1 mutations causing familial platelet disorder with propensity to myeloid malignancy. Blood. 2008;112(12):4639-4645. [DOI] [PubMed] [Google Scholar]
- 24.Kobayashi S, Kobayashi A, Osawa Y, et al. . Donor cell leukemia arising from preleukemic clones with a novel germline DDX41 mutation after allogenic hematopoietic stem cell transplantation. Leukemia. 2017;31(4):1020-1022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.