Abstract
Background:
Appalachia is a rural, socioeconomically disadvantaged region with high rates of cancer and obesity. Using community-based participatory research principles, the Appalachia Community Cancer Network tested an initiative to reduce weight among overweight and obese participants by partnering with churches, an important community-based institution in Appalachia.
Methods:
A group randomized trial was conducted with counties or groups of counties in five Appalachian states. These groups were randomly assigned to receive either monthly diet and exercise education sessions (“Walk by Faith”) (WbF) or an educational program focused on cancer screening and education (“Ribbons of Faith”) (RoF) to examine effects on weight change. Participants completed questionnaires and biometric measurements at baseline and 12 months. The primary outcome of the study was weight change from baseline to 12 months.
Results:
The relative difference in weight loss from baseline to 12 months for WbF compared to RoF was 1.4% but was not statistically significant (p=0.13). However, results varied by sex and marital status. WbF men experienced a significant 2.8% decrease in body weight, married WbF women a 1.5% decrease and unmarried WbF women a 1.5% increase compared to their respective RoF subgroups (interaction p=0.016). Among WbF participants, greater participation in monthly educational sessions was associated with greater weight loss (p=0.002).
Conclusions:
WbF facilitated weight loss mainly in male participants. Level of participation in WbF activities correlated with weight loss.
Impact:
Findings suggest that additional research is needed to better understand factors associated with participation in health promotion programs for underserved rural communities.
Keywords: Behavioral epidemiology; Cancer in minority and medically underserved populations; Diet, alcohol, smoking, and other lifestyle risk factors; Diet and cancer
Introduction:
In the United States (US), cancer is the second leading cause of death; however, in the Appalachian region of the US, cancer is the primary cause of death [1]. Access to early detection through screening and prompt and proper treatment can reduce cancer deaths. Prevention strategies can also impact cancer mortality by reducing cancer incidence. In Appalachia, cancers of the lung, colon, and cervix are the major contributors to disparities in cancer incidence. Additional cancers, such as breast cancer, contribute to disparities in cancer mortality [1, 2]. Cancer prevention strategies include tobacco prevention and cessation, sun safe behaviors, vaccination, screening, and of importance in Appalachia - obesity prevention and reduction.
The Appalachian region extends across 13 states, is mainly rural, and has medically underserved populations characterized by low socioeconomic status, poor health, and high rates of obesity [3]. Adults living in this region have lower rates of leisure-time physical activity and eat fewer servings of fruits and vegetables daily compared to other adults living in the US [4–6]. In addition to individual causes of obesity, fewer opportunities for physical activity and limited access to healthy foods create an obesogenic environment [7, 8].
Effective strategies are needed to engage Appalachian populations to reduce obesity through improved diet and increased physical activity. Qualitative studies in Appalachian communities have identified community assets that residents identify with and see as important, including family, schools, their county, and the church [9] – which could be a channel to help change health behaviors. Thus, this study used the church as a vehicle to deliver an obesity-reduction intervention among at-risk individuals within communities that were part of the Appalachian Community Cancer Network (ACCN), a trusted cancer prevention and control initiative that consisted of academic-community partnerships. In the Appalachian context, particular in Central Appalachia, most residents indicate the centrality of religion and spirituality in their lives and report being religiously affiliated, and nearly all religious congregations are Christian [10].
The ACCN is a National Cancer Institute-funded research initiative that collaborates with community-based cancer coalitions to increase awareness, provide education, and promote cancer prevention in the Appalachian region and is a collaboration of the University of Kentucky, The Ohio State University, The Pennsylvania State University, Virginia Polytechnic Institute and State University, and West Virginia University. ACCN academic partners have worked together to forge partnerships with community members and utilized community-based participatory research (CBPR) [11–14] for cancer prevention and control efforts. The purpose of this report is to provide the results of an ACCN-led faith-based intervention conducted to reduce obesity among residents of these five Appalachian states.
Materials and Methods:
The ACCN partnered with churches in the Appalachian counties of Kentucky, Ohio, Pennsylvania, Virginia, and West Virginia to conduct a group-randomized trial of an intervention (Walk by Faith) with a goal of reducing obesity through environmental and individual-level change. The primary outcome of interest was change in participant weight from baseline to 12 months, and secondary outcomes included changes in blood pressure (systolic), physical activity (measured by daily steps recorded by pedometers worn by participants and physical activity questionnaires), and diet (measured by a validated food frequency questionnaire). Details of the study design and theoretical framework for the interventions have been described elsewhere [15]; the study population, intervention, assessments, and outcomes are briefly described below.
Study Population
Churches
ACCN researchers collaborated with community members to identify size-eligible (>250 adult members) churches in Appalachian counties interested in participating in the study. Churches in counties that were designated by the Appalachian Regional Commission (ARC) as economically distressed were the first priority. However, not all selected counties were ARC-designated distressed. This was due to a number of limiting factors, including distance from regional offices, available churches with adequate congregation sizes, and number of churches within a county willing to participate.
Once churches agreed to participate, they were grouped as regions (counties or groups of counties) that were randomized to either the Walk by Faith (WbF) intervention or the Ribbons of Faith (RoF) control group. Regions were defined by grouping churches within geographic proximity prior to randomization. Each state contained two regions – one randomized to WbF and the other to RoF, for a total of 10 regions across the five states. Regions were randomized as opposed to individual churches in order to reduce the risk of contamination (multiple churches in the same area) and for logistical reasons, so that program events could be coordinated across churches in the same arm and to reduce travel time and costs for WbF program staff. As shown in Figure 1, 60 churches were approached for participation, and 28 churches agreed to participate from 10 regions across the five states (i.e., 2 regions per state). Five regions (13 churches) were randomly assigned to receive the WbF program, the dietary and physical activity faith-based intervention program, and five regions (15 churches) were randomly assigned to receive the RoF attention control program.
Figure 1.
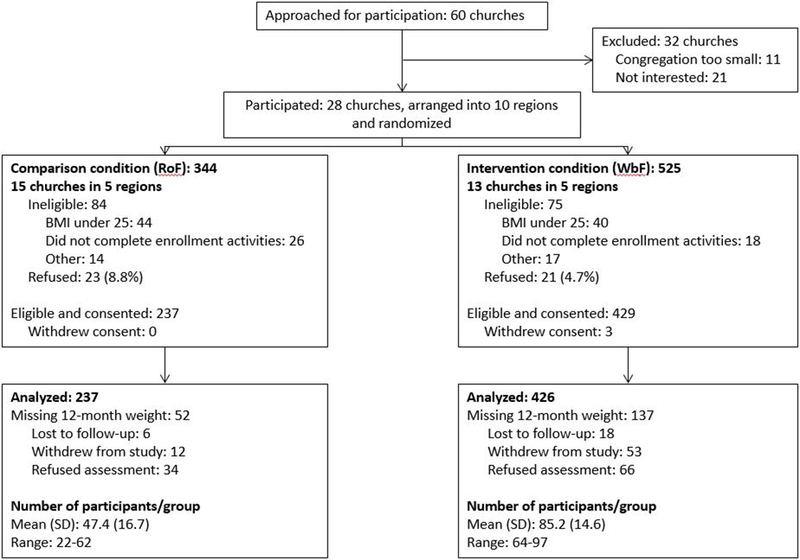
CONSORT Diagram. 60 churches were approached for participation, and 28 churches agreed to participate from 10 regions across the five states (i.e., 2 regions per state). Five regions (13 churches) were randomly assigned to receive the WbF program, the dietary and physical activity faith-based intervention program, and five regions (15 churches) were randomly assigned to receive the RoF attention control program.
Participants
The study goal was to recruit and enroll 1000 adult church members who were overweight (BMI of 25–29.9 kg/m2) or obese (BMI of 30+ kg/m2) from the participating churches in the five states. Eligibility criteria included: at least 18 years of age, attending services at the church at least 4 times in the past two months, able to understand and read English, cognitively able to provide informed consent, resident of an Appalachian county, not residing in a nursing facility or residential home, not planning to move away from the study area, willing to use a computer, no dietary restrictions prescribed for weight-loss or part of a formal weight-loss program, weight less than 400 pounds, having a BMI of at least 25 kg/m2, and, if female, not pregnant, breastfeeding or less than 9 months post-partum, or planning to become pregnant during study period. An adapted version of the Physical Activity Readiness Questionnaire (PAR-Q) was used to determine whether medical clearance from a physician was required to participate [16].
Recruitment
Participants were recruited at information sessions held at participating churches. The respective programs (WbF or RoF) were introduced through notices in church bulletins and announcements from the pulpit. At least one information session was held at each church after church services, where regional principal investigators gave brief presentations on the program, eligibility criteria, assessments, and participant time commitment. Following the presentation, study staff were available to answer questions about the study, complete informed consent, and complete eligibility screening. Eligible participants then proceeded to different stations set up within the church where weight, height, waist and hip circumference (used to compute waist to hip ratio, WHR), blood pressure, resting heart rate, and body image were assessed following specific, standardized protocols [17, 18]. Interested individuals who were unable to attend an information session were encouraged to make an appointment with a field interviewer hired from the local community to complete the enrollment process and baseline data collection. Participants were given gift cards as a thank-you for travel to the church and time for completing baseline and annual follow-up surveys and biometric measurements. The project was implemented in two waves. Ohio and Pennsylvania acted as a vanguard group and recruited participants from January 2012 through September 2012 (Wave 1). Lessons learned during Wave 1 recruitment were used to modify and refine recruitment strategies for when Kentucky, Virginia, and West Virginia, recruited participants from November 2012 through September 2013 (Wave 2).
Intervention Programs
The intervention program was developed and maintained using community-engaged strategies and was delivered in the church setting, an influential part of daily life within Appalachian populations. CBPR principles were employed in many ways. First, both programs had initially been developed by Ohio Appalachian community coalitions in response to health problems in their counties. Focus groups were then used to decide the names of the programs (Walk by Faith and Ribbons of Faith), to obtain a list of topics of interest for the education sessions in each arm, and to review materials. A community advisory board was assembled to review counties selected and education session and other program materials. All materials were edited to reflect this feedback prior to implementation. Throughout the course of the study, the community advisory board was called upon for input on all aspects of the study, including recruitment and attendance at education sessions. Local navigators from the churches helped promote the study and deliver the intervention. Given that changing diet and exercise is difficult, such promotion was essential [19]. In Appalachia, norms about these behaviors are not as positive as needed and life situations often create stress that reinforces poor dietary behaviors; moreover, in rural Appalachia, walking is difficult due to lack of sidewalks, although church representatives were encouraged to mark walking paths and organize group walks [20].
Walk by Faith:
The intervention program, WbF, focused on environmental and individual level behavioral changes to reduce overweight/obesity by focusing on components of a healthy diet and increasing physical activity. Educational and motivational materials were delivered to participants at monthly sessions held at each church and with the aid of a dedicated website, Faithfully Living Well (FLW). Each session was approximately one hour in length. Print handouts of any presentations were provided to attendees and made available in the church for participants who were unable to attend. A touchscreen computer, printer and high-speed internet were installed in each church to encourage participants to visit FLW and print healthy recipes or health-related articles. At least one member of each church volunteered to be a church navigator who facilitated program events and assisted participants, as needed.
The diet intervention focused on increasing fruit and vegetable and water intake, reducing sugary drink consumption, and reducing dietary fat. Short and long-term goals were set for each participant with the personal assistance of trained regional staff using the output of the baseline web surveys as a starting point. Participants were encouraged to meet with regional staff quarterly to discuss previous goals, adjust if necessary, and set new short and long-term goals. Examples of goals included trying a new fruit and/or vegetable each month, increasing number of servings of fruits or vegetables per day, increasing average steps per day over a period of time, and losing a certain amount of weight over a period of time.
The navigators, community advisors, and regional project staff worked together to identify strategies to support environmental approaches to increase physical activity, such as setting up walking courses, group walks, and walking challenges. They also identified safe walking paths within the communities and secured promotional offers and donations from local businesses and organizations to be used as incentives to encourage participants to increase their physical activity levels and utilize program components, such as completing dietary inventories, attending events, and using the FLW website. Healthy potluck meals were held in the churches. Omron HJ-720ITC pedometers, nutrition guides, and diet and exercise journals were provided to each enrolled participants. The FLW website also allowed participants to upload steps from their pedometers, track progress toward their individual walking and weight loss goals, read health-related articles, submit and access recipes, participate in discussion forums, view photo albums, and have access to a rewards page – all tailored to each county. A celebration event was held in each church after the active program was completed 12 months after the first event. During these events, participants were invited to talk about their experiences and progress and were given rewards and certificates of completion.
Ribbons of Faith:
RoF focused on environmental and individual level behavior changes to increase cancer screening knowledge and promote cancer screening as recommended by the American Cancer Society. Each church was provided a touchscreen computer, printer and high-speed internet to allow participants to access and print cancer screening information online. At least one volunteer navigator in each church was appointed to facilitate program events. Components of the RoF program included an information session, a health fair, cancer education inserts in church bulletins, and monthly education sessions with brochures and other handouts. Monthly education sessions were approximately one hour in length and spanned a variety of cancer-related topics, such as the importance of understanding their family health history and encouraging loved ones to get cancer screening, and site-specific cancer education sessions on colon, skin, lung, breast, cervical, prostate and testicular cancers. Church members were encouraged to complete age and sex-appropriate screening tests for cervical, breast, colorectal, prostate, testicular, and skin cancers. A celebration event was held after the 12-month active phase.
Measures
Height was measured at baseline only, and weight, blood pressure, and waist and hip circumference were measured at baseline and 12-months. Participants also completed paper and telephone-based surveys containing questions on demographic characteristics, socioeconomic status, health literacy, cancer diagnoses and cancer screening history, tobacco use history, depression, social support, loneliness, and sleep habits.
WbF participants completed two additional web-based surveys with the assistance of study staff. An interactive, image-based food frequency questionnaire was used to assess daily dietary intake of food and beverages. This inventory was developed by Viocare, Inc., a private technology company focused on health and wellness programs [21, 22]. The International Physical Activity Questionnaire (IPAQ) long form was used to measure physical activity at baseline and 12-months. Measures of walking, moderate-intensity, vigorous-intensity, and total physical activity were included in this study [23]. Physical activity was reported in terms of days per week and minutes and/or hours per day over the prior seven days and was converted to MET-minutes per week for analyses. The IPAQ has been used to measure physical activity in diverse populations and is reliable (r=0.8), with acceptable validity (r=0.3) compared with accelerometry [24].
Analysis:
A longitudinal mixed effects modeling approach was used to evaluate the primary outcome of weight change between the intervention and attention control groups. A random effect was included for the ten randomized regions by time using an unstructured covariance matrix. Correlated errors were modeled within participant by time, also using an unstructured covariance matrix. Fixed effects included arm, time, and the interaction of time and arm. In this approach, a significant interaction would indicate a treatment effect (i.e., differential change in weight from baseline to 12-months by arm). Age and sex were identified as predictive of weight using only the baseline data and were included in the model. Intention-to-treat principles were employed in the analysis. All participants who were assessed at baseline were included in the analysis regardless of whether their follow-up data were obtained. The mixed effect modeling framework employed is a likelihood-based approach, and as such is an effective method in dealing with the additional bias and uncertainty associated with missing outcome data under the missing at random assumption [25–27].
Diagnostic plots of the model residuals were used to determine if the model assumptions were satisfied, and transformations were used where necessary. Where logarithmic transformations were used, estimates are expressed in terms of percent change from baseline. Three-way interaction tests were used to test for significant modification of the treatment effect over time. The same modeling approach was used for the secondary outcomes of blood pressure, WHR, physical activity and fruit and vegetable consumption. Analyses examining the impact of program participation in the intervention arm (WbF) participants only used a longitudinal model without the random effect for region. Degrees of freedom were determined using the Kenward-Roger method [28] and all analyses were conducted in SAS v9.4 (SAS Institute, Cary, NC).
Results:
Accrual and 12-month Follow-up:
Sixty churches were contacted and responded to the study team to discuss participation in the study. Of these churches, 15 (25%) were not interested in participating and 6 (10%) reported being too busy to participate. Eleven churches (18%) were deemed ineligible due to small congregation sizes. The remaining 28 churches (57% of eligible churches) across the five states participated in the study.
As shown in the CONSORT diagram (Figure 1), 344 church members were screened in the RoF arm, of which 84 were deemed ineligible and 23 (8.9% of the eligible participants) refused to participate, leaving 237 participants who consented to participate. In the WbF arm, 525 church members were screened, of which 75 deemed ineligible and 21 (4.7% of the eligible participants) refused to participate; thus 429 participants were consented. Over time, three WbF participants withdrew consent, leaving 426 eligible participants to be included in the analysis.
At 12-months, 52 (21.9%) RoF participants and 137 (32.2%) WbF participants did not participate in biometric assessments and therefore were missing weight data.
Participant Characteristics:
Participant characteristics are presented by arm in Table 1. Overall, more women (71%) were enrolled in the study than men with relatively fewer women participating in the RoF arm (65% of RoF participants vs. 74% of WbF). The remaining demographic characteristics were similar across the two arms. Mean age of participants was approximately 56 years. Most participants had some college or a bachelor degree (75%). About 80% of the sample was married or living with a partner and 62% of participants worked full or part-time. Two-thirds (67%) of participants were privately insured, 28% had public insurance, and only 5% reported being uninsured. About 25% of participants had incomes under $40,000 per year. At baseline, mean weight was 92 kg and mean BMI was 33 kg/m2. Systolic and diastolic blood pressure averaged 135.9 and 82.4 mmHg, respectively.
Table 1:
Participant Demographic and Physical Measures at Baseline (N=663)
| Variable | Level | Ribbons of Faith (n=237) | Walk by Faith (n=426) | Total |
|---|---|---|---|---|
| Sex | Male | 84 (35.4%) | 110 (25.8%) | 194 (29.3%) |
| Female | 153 (64.6%) | 316 (74.2%) | 469 (70.7%) | |
| State of church | KY | 22 (9.3%) | 64 (15.0%) | 86 (13.0%) |
| OH | 52 (21.9%) | 97 (22.8%) | 149 (22.5%) | |
| PA | 62 (26.2%) | 93 (21.8%) | 155 (23.4%) | |
| VA | 40 (16.9%) | 76 (17.8%) | 116 (17.5%) | |
| WV | 61 (25.7%) | 96 (22.5%) | 157 (23.7%) | |
| Age | Mean (SD) | 56.1 (12.5) | 55.5 (12.9) | 55.7 (12.8) |
| Are you of Hispanic, Latino, or Spanish origin? | Yes | 2 (0.8%) | 2 (0.5%) | 4 (0.6%) |
| No | 235 (99.2%) | 424 (99.5%) | 659 (99.4%) | |
| Race | White | 234 (98.7%) | 415 (97.4%) | 649 (97.9%) |
| African American | 1 (0.4%) | 11 (2.6%) | 12 (1.8%) | |
| Other | 2 (0.8%) | 0 (0.0%) | 2 (0.3%) | |
| Education | <=HS/GED | 54 (22.8%) | 113 (26.5%) | 167 (25.2%) |
| Some coll or assoc deg | 87 (36.7%) | 160 (37.6%) | 247 (37.3%) | |
| Bachelor deg or more | 96 (40.5%) | 153 (35.9%) | 249 (37.6%) | |
| Marital status | Married/living w partner | 191 (80.6%) | 331 (77.7%) | 522 (78.7%) |
| Divorced/separated/widowed | 32 (13.5%) | 75 (17.6%) | 107 (16.1%) | |
| Never been married | 14 (5.9%) | 20 (4.7%) | 34 (5.1%) | |
| Employment status | Full-time/part-time/student | 154 (65.0%) | 258 (60.7%) | 412 (62.2%) |
| Unemp/keeping house/disabled | 23 (9.7%) | 59 (13.9%) | 82 (12.4%) | |
| Retired | 60 (25.3%) | 108 (25.4%) | 168 (25.4%) | |
| Insurance status 3-level | Uninsured | 11 (4.6%) | 20 (4.7%) | 31 (4.7%) |
| Public | 64 (27.0%) | 121 (28.4%) | 185 (27.9%) | |
| Private | 162 (68.4%) | 285 (66.9%) | 447 (67.4%) | |
| Household income | < $40,000 | 47 (25.1%) | 90 (25.9%) | 137 (25.6%) |
| $40K to $69,999 | 70 (37.4%) | 128 (36.8%) | 198 (37.0%) | |
| $70K+ | 70 (37.4%) | 130 (37.4%) | 200 (37.4%) | |
| Smoking status | Never | 180 (75.9%) | 303 (71.1%) | 483 (72.9%) |
| Former | 55 (23.2%) | 108 (25.4%) | 163 (24.6%) | |
| Current | 2 (0.8%) | 15 (3.5%) | 17 (2.6%) | |
| Weight (kg) | Mean (SD) | 91.6 (18.9) | 92.6 (19.9) | 92.2 (19.5) |
| BMI | Mean (SD) | 32.7 (5.8) | 33.5 (6.6) | 33.2 (6.3) |
| Waist/hip ratio | Mean (SD) | 0.91 (0.08) | 0.90 (0.09) | 0.90 (0.09) |
| Systolic BP | Mean (SD) | 134.5 (17.3) | 136.7 (17.7) | 135.9 (17.6) |
| Diastolic BP | Mean (SD) | 81.2 (9.9) | 83.0 (10.8) | 82.4 (10.5) |
| Baseline estimated daily intake of fruit + vegetable (servings) | Mean (SD) | 2.9 (2.2) | 2.8 (2.0) | 2.8 (2.1) |
| MSPSS score (higher indicates greater support, range: 12–84) | Mean (SD) | 73.9 (8.8) | 72.2 (9.0) | 72.8 (9.0) |
| CES-D greater than 15 | Yes | 26 (11.0%) | 60 (14.2%) | 86 (13.0%) |
| No | 211 (89.0%) | 364 (85.8%) | 575 (87.0%) | |
| When was the last time you had a pap test? | Never | 0 (0.0%) | 4 (1.3%) | 4 (0.9%) |
| Less than 1 yr | 77 (50.7%) | 158 (50.0%) | 235 (50.2%) | |
| More than 1 yr | 75 (49.3%) | 154 (48.7%) | 229 (48.9%) | |
| When was the last time you had a mammogram? | Never | 5 (3.6%) | 6 (2.2%) | 11 (2.6%) |
| Less than 1 yr | 103 (74.6%) | 198 (71.2%) | 301 (72.4%) | |
| More than 1 yr | 30 (21.7%) | 74 (26.6%) | 104 (25.0%) | |
| When was the last time you had a FOBT? | Never | 85 (49.7%) | 172 (59.5%) | 257 (55.9%) |
| Less than 1 yr | 12 (7.0%) | 22 (7.6%) | 34 (7.4%) | |
| More than 1 yr | 74 (43.3%) | 95 (32.9%) | 169 (36.7%) | |
| When was the last time you had a colonoscopy? | Never | 24 (13.9%) | 65 (22.4%) | 89 (19.2%) |
| Less than 10 yrs | 146 (84.4%) | 219 (75.5%) | 365 (78.8%) | |
| More than 10 yrs | 3 (1.7%) | 6 (2.1%) | 9 (1.9%) | |
| When was the last time you had a flex sig? | Never | 142 (82.1%) | 250 (87.7%) | 392 (85.6%) |
| Less than 5 yrs | 1 (0.6%) | 6 (2.1%) | 7 (1.5%) | |
| More than 5 yrs | 30 (17.3%) | 29 (10.2%) | 59 (12.9%) | |
| When was the last time you had a PSA test? | Never | 6 (9.8%) | 13 (20.3%) | 19 (15.2%) |
| Less than 1 yr | 39 (63.9%) | 42 (65.6%) | 81 (64.8%) | |
| More than 1 yr | 16 (26.2%) | 9 (14.1%) | 25 (20.0%) | |
| Within guidelines for CRC screening by either FOBT, flexsig, or colonoscopy? | Yes | 148 (85.5%) | 227 (78.3%) | 375 (81.0%) |
| No | 25 (14.5%) | 63 (21.7%) | 88 (19.0%) | |
| IPAQ Physical Activity | Mean (SD) of Walking MET-min/week | 1323.8 (1468.1) | 1425.4 (1573.0) | 1390.9 (1537.7) |
| Mean (SD) of Moderate-intensity MET-min/week | 3580.6 (2826.5) | 3102.6 (2762.5) | 3264.9 (2791.2) | |
| Mean (SD) of Vigorous-intensity MET-min/week | 1387.7 (2048.7) | 958.2 (1808.4) | 1104.0 (1902.6) | |
| Mean (SD) of Total MET-min/week | 6292.1 (5104.2) | 5486.2 (4689.3) | 5759.8 (4844.9) |
Primary Outcome:
Results are reported in Table 2. Although there was a 1.4% relative decrease (95% CI: −3.2, 0.5; p=0.13) in weight for WbF participants compared to RoF participants, the difference was not statistically significant. Weight decreased among WbF participants by 1.2% (95% CI: −2.5, 0.0) and increased slightly among the RoF participants by 0.1% (95% CI: −1.2, 1.5). After adjusting for age, sex, marital status and education, changes in weight over time were similar in both groups (p=0.13).
Table 2:
Model adjusted mean estimates and differences for primary and secondary outcomes
| Outcome (change from baseline) | WbF Adj Mean (95% CI) | RoF Adj Mean (95% CI) | Difference (95% CI) | p-value for difference |
|---|---|---|---|---|
| Primary | ||||
| Weight (%) | −1.2 (−2.5, 0.0) | 0.1 (−1.2, 1.5) | −1.4 (−3.2, 0.5) | 0.13 |
| Secondary | ||||
| Waist-hip ratio | −0.012 (−0.025, 0.00) | 0.001 (−0.012, 0.015) | −0.014 (−0.032, 0.005) | 0.57 |
| Systolic BP (%) | −1.9 (−3.7, 0.00) | −1.3 (−3.3,0.8) | −0.6 (−3.4, 2.3) | 0.64 |
| Fruit and vegetable consumption (%) | 15.5 (−6.6, 42.9) | −7.7 (−25.7, 14.7) | 25.1 (−7.6, 69.5) | 0.12 |
| MET-minutes per week (%) | 36.7 (−35.1, 188.2) | 1.1 (−18.2, 24.8) | 35.4 (−1.0, 85.1) | 0.056 |
Tests for effect modification were conducted using a three-way interaction between arm, time and the given covariate. No differences were found for age (p=0.66), education (p=0.57), employment status (p=0.83), insurance status (p=0.94), and income (p=0.12). As only 18 (9%) of the male participants were unmarried, a new three-level variable was created with categories of male (n=194), female-married (n=346) and female-unmarried (n=123) to explore the relationship with marital status. The three-way interaction test for this variable was significant (p=0.016) with WbF males showing a 2.8% weight decrease (95% CI: −5.0, −0.5) relative to the RoF arm, WbF married females a 1.5% decrease (95% CI: −3.4, 0.5) and WbF unmarried females a 1.5% increase (95% CI: −1.3, 4.4).
Secondary Outcomes:
The secondary outcomes of waist-hip ratio, blood pressure (systolic), physical activity and self-reported fruit and vegetable consumption were evaluated using the same methods and are also displayed in Table 2. There was no significant intervention effect for waist-hip ratio (p=0.57), systolic blood pressure (p=0.72), and fruit and vegetable consumption p=0.12). After adjusting for sex, age, education and BMI at baseline, participants in the WbF intervention group reported increases of 35% in walking MET-minutes per week relative to participants in the RoF control group (95% CI: −1.0, 85.1; p=0.0556). There were no other significant changes in physical activity between the WbF intervention and RoF control groups.
Impact of Program Participation:
For WbF participants, process data was used to evaluate program participation and its effect on weight change. Participants were invited to attend between 11 and 14 sessions over the 12-month intervention period. Forty-four percent of WbF participants attended three or more sessions. There was a significant positive relationship (p<0.001) between percentage of sessions attended and weight loss with a 20% absolute increase in attendance (roughly two additional sessions) resulting in a 0.8% decrease in weight (95% CI: −1.2, −0.3). Daily website usage was also tracked and revealed a wide variety of patterns. While the median number of logins was four, the distribution was highly skewed with 10% of participants using the website on 20 or more days. During Wave 1 of the study conducted in the first two states, there were numerous problems that deterred website usage by the participants. When the three remaining states started the program, the problems were largely resolved and participation increased from a median of two to five logins. There was a significant relationship between weight change and the number of daily logins in Wave 2 church members (p<0.001) that was not documented in Wave 1 church members (p=0.67). For Wave 2 churches, a doubling of the number of daily logins resulted in a 0.4% decrease in weight (95% CI: −0.7,−0.1).
Discussion:
This study tested an intervention to reduce weight in overweight and obese Appalachian residents and found no significant effect overall; however, subgroups, e.g., men, benefited from the program. Although a 5% weight loss is generally accepted as the threshold for health benefits, we saw an average decrease of only 2.8% among men [29]. More women participated in the WbF intervention, however, men tended to lose more weight. Prior studies have found that men, in general, are less likely to participate in weight loss programs compared to women [30]. However, men tend to lose weight faster due to higher metabolic rates [31]. No effect of the intervention was seen on blood pressure, possibly due to the low rate of weight loss and the few participants uploading step data to suggest regular walking.
Since the Appalachian region suffers from disparities in obesity and cancer incidence and mortality, such an intervention is needed to reduce risk. There are several reasons why this intervention might not have been as effective as hypothesized. First, we examined the effectiveness of the various components of the intervention. While our sensitivity analyses showed that WbF participants who logged into the website, visited the website regularly, and attended education sessions were more likely to lose weight versus those who did not, these components of the intervention had poor adherence. Reasons for not logging steps were associated with difficulties with the technical aspects of the intervention for Wave 1 churches. Specifically, the software developed to facilitate pedometer data uploads to the FLW website proved to be unreliable during the first two months of the Wave 1 WbF intervention and, even after improvement, remained too complicated for some participants. Some participants grew frustrated with the pedometer software as research staff worked toward a simpler, more dependable, and permanent solution. As a result, only limited pedometer data were recorded from participants in Wave 1 states, even though the research team tried various strategies to collect the data. For example, a system was developed whereby participants could provide their steps either on paper or by email to a church navigator, interventionist, or system administrator. Any of these individuals could then upload step counts per day manually in batches through a backend on the FLW website. Participants’ accounts would reflect the changes immediately, and the participant would still earn points for these steps on the FLW website. After a solution was developed, instructions detailing the new upload process were released to all WbF participants, resulting in an increase in pedometer upload activity, and website traffic increased as a result.
Wave 2 states benefited from this improvement, and study staff learned that a brief introduction to FLW and pedometer demonstration session at the onset of the intervention phase enhanced participant comfort levels with the new materials. While the pedometers used were considered “state of the art” when the project was developed, the difficulties encountered suggest that these were less than ideal tools for this application. We have no data to indicate if pedometer use and effectiveness would be better if newer activity tracker tools (e.g., Fitbit or smartphone applications) with simpler interfaces were used in future programs.
The project website, FLW, was not well-utilized by participants. When the study was being developed in 2010, eHealth programs were shown to be effective and were gaining in popularity in many settings. The use of technology was meant to be a tool to aid participants in reaching diet, physical activity and weight loss goals. The research team was aware of the potential for complications due to lack of high-speed internet access and population familiarity with technology and planned for these potential pitfalls by offering simplified, touch-screen computers and high-speed internet connections within the churches, less-complicated pedometers than many on the market at the time, and trained paid and volunteer staff within the churches to offer assistance with technology.
Website content was added throughout the intervention in an effort to keep participants engaged in the program, and FLW encouraged user-generated content submissions as a strategy to encourage participants to revisit the website on a regular basis. Moreover, to increase access to a computer, each church was given a computer for participants to use. The software used to house the articles and recipes linked to the website in a way to track number of views per item, but it did not offer a feature to track where the physical user was when the item was viewed, so tracking of usage by location (home v. church setting) was not available.
Unfortunately, even though the study also provided internet access, many churches had unreliable internet connections, likely due to their rural location, making connection difficult on a consistent basis. We also found that many participants did not have time to come to the church to use the computer. Of those participants who reported owning computers, 53.2% reported having dial-up or digital subscriber line (DSL) internet transmitted through telephone lines with lower speeds and reliability as compared to cable or fiber optic broadband internet more common in urban areas. Many participants were older adults having little experience with technology and even less interest in learning how to use new devices or systems. A hybrid method of physically sharing information along with limited use of very simple technology with little to no reliance on a constant high-speed internet connection would be ideal in this setting and should be considered in future studies.
Low attendance at the education sessions is also likely to have influenced the lack of effect of the intervention program. On average, participants attended only 32% of the intervention sessions. Education session attendance waned in some churches and was inconsistent in others after the first few months of program activities. Low attendance at the education sessions was most likely due to participants and their family members who accompanied them to church having competing interests and activities after church services. In an effort to increase participation at these sessions, church bulletin inserts, announcements from the pulpit, and reminder phone calls were employed to increase participant awareness of the education sessions. Trivia games and prizes were incorporated into the sessions in order to increase participant interest. Some WbF churches chose to recognize participants with the most steps for the month at education sessions, as well. Although content of monthly education sessions was held constant to ensure participants across multiple states received similar experiences, local experts nominated by each church (physicians, nurses from local health departments) presented education sessions when they were available. These strategies helped to increase attendance at education sessions during the 12-month program, but not to our goal of 80% of participants attending 80% of sessions.
The second area to examine is recruitment and follow-up rates. Not all church members attended the information sessions at the churches. We do not have any way to assess the percentage of church members who attended the sessions, as these numbers fluctuate in each church weekly. The percentage of participants who did not complete follow-up measurements in both WbF and RoF arms (32.2% and 21.9%, respectively) was higher than anticipated and was attributed to migration of church members and reduced interest in the program over time. Participants were encouraged to schedule meetings with field interviewers to complete follow-up measures before or after services and as time permitted throughout the week. Sign-up sheets were made available at the church. Field interviewers and state coordinators and managers called and mailed letters to participants to try to schedule follow-ups as well.
Lastly, we examined the use of churches to deliver this program. Because we conducted this behavioral intervention across 28 churches, 10 regions, and 5 states, experiences varied across states and between churches in the same state. We hypothesized that churches would engage people of all socioeconomic statuses. However, churchgoers of lower socioeconomic status may have skipped the enrollment session as they may have thought they had no time to participate. To enroll more participants of lower socioeconomic status, researchers might have to enroll residents from different organizations, such as worksites that employ blue collar or hourly employees or food banks.
All churches participating in WbF and RoF were Christian, but denominations differed, as did resources available within the churches and counties. Meetings within the church and worship and prayer service days and times varied and determined when WbF or RoF activities could be held. Physical spaces available for program activities also varied, with some churches having full kitchens that were used for cooking demonstrations and gyms for physical activity events, while other churches were limited to holding WbF and RoF events in meeting halls or church basements. Some communities offered supportive built environments and physical activity resources and stores to buy fruits and vegetables, while others had no grocery stores county-wide. In addition, it was more difficult for regional staff and navigators to secure incentives in counties with fewer local businesses and resources than counties with more community resources.
The level of commitment from church leaders and volunteer navigators also differed from church to church. Participants tended to be more active in the program in churches where pastors wore pedometers and promoted and attended education sessions and activities. Navigator buy-in also played a major role in participant engagement. Churches with more than one navigator or a very involved navigator tended to have better attendance at program events. In addition, WbF participants in churches with active navigators were afforded more opportunities to upload their pedometer steps to FLW than those in churches with less active navigators. Field staff, navigator or pastor turnover was a challenge for most states in at least one church, which also played a role in participants’ or overall church interest in the programs.
Despite these challenges, we were able to recruit 28 churches from five Appalachian states to participate in a year-long intervention that was developed and implemented with on-going community input. Participants who actively participated and attended more education sessions were significantly more likely to lose weight. More importantly, our use of churches as a social vehicle to motivate behavior change was validated.
In conclusion, churches are an important part of the Appalachian community. However, to increase the impact of a church-based diet and exercise intervention program, more in-person contact is needed. While messages of faith were included in both interventions and the social support effect of the church congregation was utilized for classes and activities, the effect of the intervention on reducing body weight was not realized. Thus, additional efforts to tie this important community establishment to healthy choices need to be tested. Future studies can build on our experience to design, implement and test these types of intervention programs to address health disparities in Appalachia or similar areas.
Acknowledgments
FUNDING:
This research was supported by grant U54 CA153604 from the National Institutes of Health and a Pelotonia Idea Grant. This study was also supported by the National Cancer Institute Grant P30 CA016058, The Behavioral Measurement Shared Resource at The Ohio State University Comprehensive Cancer Center.
Footnotes
The authors declare no potential conflicts of interest.
References
- 1.Blackley D, Behringer B, and Zheng S, Cancer mortality rates in Appalachia: descriptive epidemiology and an approach to explaining differences in outcomes. J Community Health, 2012. 37(4): p. 804–13. [DOI] [PubMed] [Google Scholar]
- 2.Wingo PA, et al. , Cancer in Appalachia, 2001–2003. Cancer, 2008. 112(1): p. 181–92. [DOI] [PubMed] [Google Scholar]
- 3.Encyclopedia of Appalachia. Choice: Current Reviews for Academic Libraries, 2006. 44(3): p. 464–464. [Google Scholar]
- 4.Diabetes Interactive Atlases. July 10, 2013].
- 5.The Cancer Burden in Appalachia. 2009, Appalachia Community Cancer Network.
- 6.Michimi A and Wimberly MC, Spatial patterns of obesity and associated risk factors in the conterminous U.S. Am J Prev Med, 2010. 39(2): p. e1–12. [DOI] [PubMed] [Google Scholar]
- 7.Gordon-Larsen P, et al. , Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics, 2006. 117(2): p. 417–24. [DOI] [PubMed] [Google Scholar]
- 8.Swinburn B, Egger G, and Raza F, Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med, 1999. 29(6 Pt 1): p. 563–70. [DOI] [PubMed] [Google Scholar]
- 9.Coyne CA, Demian-Popescu C, and Friend D, Social and cultural factors influencing health in southern West Virginia: a qualitative study. Prev Chronic Dis, 2006. 3(4): p. A124. [PMC free article] [PubMed] [Google Scholar]
- 10.Kosmin e.a. American religious identification survey. 2008; Available from: http://commons.trincoll.edu/aris/.
- 11.Bencivenga M, et al. , Community partnerships, food pantries, and an evidence-based intervention to increase mammography among rural women. J Rural Health, 2008. 24(1): p. 91–5. [DOI] [PubMed] [Google Scholar]
- 12.Katz ML, et al. , Community involvement in the development and feedback about a colorectal cancer screening media campaign in Ohio Appalachia. Health Promot Pract, 2011. 12(4): p. 589–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schoenberg NE, Howell BM, and Fields N, Community strategies to address cancer disparities in Appalachian Kentucky. Fam Community Health, 2012. 35(1): p. 31–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vanderpool RC, et al. , Adapting and implementing evidence-based cancer education interventions in rural Appalachia: real world experiences and challenges. Rural Remote Health, 2011. 11(4): p. 1807. [PMC free article] [PubMed] [Google Scholar]
- 15.Baltic RD, et al. , Study design, intervention, and baseline characteristics of a group randomized trial involving a faith-based healthy eating and physical activity intervention (Walk by Faith) to reduce weight and cancer risk among overweight and obese Appalachian adults. Contemp Clin Trials, 2015. 44: p. 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gledhill N, Physical Activity Readiness Questionnaire-PAR-Q. Ottawa: Minister of Public Works and Government Services Canada, 2002. [Google Scholar]
- 17.Hamilton CM, et al. , The PhenX Toolkit: get the most from your measures. Am J Epidemiol, 2011. 174(3): p. 253–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williamson DA, et al. , Body image assessment for obesity (BIA-O): development of a new procedure. Int J Obes Relat Metab Disord, 2000. 24(10): p. 1326–32. [DOI] [PubMed] [Google Scholar]
- 19.Mastellos N, et al. , Transtheoretical model stages of change for dietary and physical exercise modification in weight loss management for overweight and obese adults. Cochrane Database Syst Rev, 2014(2): p. CD008066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wewers ME, et al. , Risky behaviors among Ohio Appalachian adults. Prev Chronic Dis, 2006. 3(4): p. A127. [PMC free article] [PubMed] [Google Scholar]
- 21.Viocare. Viocare Nutrition Software Solutions for Healthcare & Research; Available from: http://www.viocare.com/about.html.
- 22.Kristal AR, et al. , Evaluation of web-based, self-administered, graphical food frequency questionnaire. J Acad Nutr Diet, 2014. 114(4): p. 613–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sjostrom M BF, Craig C, Towards Standardized Global Assessment Of Heatlh-related Physical Activity-The International Physical Activity Questionnaires (ipaq). Medicine & Science in Sports & Exercise, 2002. 34(5). [Google Scholar]
- 24.Craig CL, et al. , International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc, 2003. 35(8): p. 1381–95. [DOI] [PubMed] [Google Scholar]
- 25.Kenward MG and Carpenter J, Multiple imputation: current perspectives. Stat Methods Med Res, 2007. 16(3): p. 199–218. [DOI] [PubMed] [Google Scholar]
- 26.Peters SA, et al. , Multiple imputation of missing repeated outcome measurements did not add to linear mixed-effects models. J Clin Epidemiol, 2012. 65(6): p. 686–95. [DOI] [PubMed] [Google Scholar]
- 27.Twisk J, et al. , Multiple imputation of missing values was not necessary before performing a longitudinal mixed-model analysis. J Clin Epidemiol, 2013. 66(9): p. 1022–8. [DOI] [PubMed] [Google Scholar]
- 28.Kenward MG and Roger JH, Small sample inference for fixed effects from restricted maximum likelihood. Biometrics, 1997. 53(3): p. 983–97. [PubMed] [Google Scholar]
- 29.Donnelly JE, et al. , American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc, 2009. 41(2): p. 459–71. [DOI] [PubMed] [Google Scholar]
- 30.Hwang KO, et al. , Website usage and weight loss in a free commercial online weight loss program: retrospective cohort study. J Med Internet Res, 2013. 15(1): p. e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williams RL, et al. , Effectiveness of weight loss interventions--is there a difference between men and women: a systematic review. Obes Rev, 2015. 16(2): p. 171–86. [DOI] [PMC free article] [PubMed] [Google Scholar]


