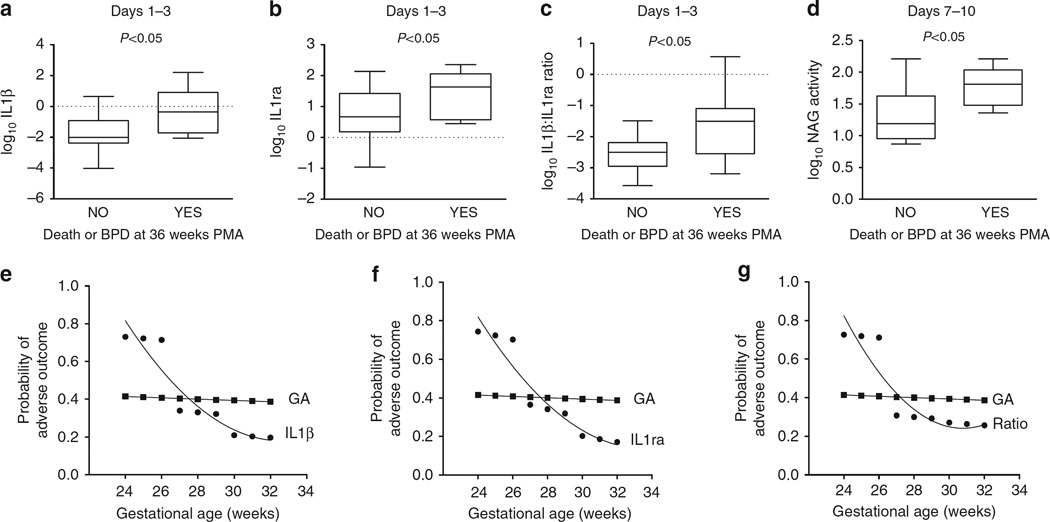
Figure 4. Tracheal aspirate IL1β, IL1ra and N-acetyl glucosaminidase activity are associated with adverse outcome in preterm infants intubated for respiratory failure.
(a–c) Box plots of log-transformed IL1β, IL1ra and IL1β:IL1ra ratio in tracheal aspirates obtained between days 1 and 3 segregated by adverse outcome (death or BPD at 36 weeks PMA). Each biomarker was significantly elevated between days 1 and 3 in infants that subsequently developed adverse outcome at 36 weeks PMA. (d) Box plot of log-transformed NAG activity between days 7 and 10 segregated by adverse outcome. NAG activity at 710 days was increased in those infants that developed death or BPD at 36 weeks PMA. (e–g) Comparisons of the contribution of gestational age and each of the tracheal aspirate biomarkers to the probability of adverse outcome at each gestational age. Using the 50th percentile value for each biomarker at 1–3 days, the probability of adverse outcome at each gestational age was determined and compared with the contribution of gestational age alone. Gestational age alone contributed 40% to the probability of adverse outcome at each gestational age. For infants <27 weeks gestation, each biomarker (IL1β, IL1ra and IL1β:IL1ra ratio) doubled the probability of adverse outcome above that of gestational age alone.