Abstract
Background:
Cardiovascular disease is a leading economic and medical burden in the United States (US). As an important risk factor for cardiovascular disease, hypertension represents a critical point of intervention. Less is known about longitudinal effects of neighborhood deprivation on blood pressure outcomes, especially in light of new hypertension guidelines.
Methods:
Longitudinal data from the Dallas Heart Study facilitated multilevel regression analysis of the relationship between neighborhood deprivation, blood pressure change, and incident hypertension over a 9-year period. Factor analysis explored neighborhood perception, which was controlled for in all analyses. Neighborhood deprivation was derived from US Census data and divided into tertiles for analysis. Hypertension status was compared using pre-2017 and 2017 hypertension guidelines.
Results:
After adjusting for covariates, including moving status and residential self-selection, we observed significant associations between residing in the more deprived neighborhoods and 1) increasing blood pressure over time and 2) incident hypertension. In the fully adjusted model of continuous blood pressure change, significant relationships were seen for both medium (SBP: β=4.81, SE=1.39, p=0.0005; DBP: β=2.61, SE=0.71, p=0.0003) and high deprivation (SBP: β=7.64, SE=1.55, p<0.0001; DBP: β=4.64, SE=0.78, p<0.0001). In the fully adjusted model of incident hypertension, participants in areas of high deprivation had 1.69 higher odds of developing HTN (OR 1.69; 95% Cl 1.02, 2.82), as defined by 2017 hypertension guidelines. Results varied based on definition of hypertension used (pre-2017 vs. 2017 guidelines).
Conclusion:
These findings highlight the potential impact of adverse neighborhood conditions on cardiometabolic outcomes, such as hypertension.
Keywords: Hypertension, neighborhood deprivation, socioeconomic status, neighborhood perception, blood pressure, cardiometabolic risk factors
Introduction
Based on recently updated guidelines,1 hypertension (HTN) affects nearly 50% of the U.S. population and is a major contributor to morbidity and mortality via cardiovascular disease,1 stroke,2,3 myocardial infarction,4 and organ failure.5 Both biological and behavioral correlates of HTN have been well described, including neighborhood correlates to HTN prevalence,6,7 but few studies have addressed the broader socio-environmental factors impacting HTN incidence and progression.8,9 Although patients experience and react to environmental influences outside of standard clinical care, the effects of the environment are seen during clinical disease management and therefore are worthy of investigation and understanding within the clinical environment. Understanding community-level contributions to incident HTN may be critical to successful population health interventions, particularly in light of recent changes to HTN guidelines.1
There are consistent area-level socioeconomic factors that contribute to cardiovascular disease risk and overall mortality independently of individual-level socioeconomic measures.10–12 Neighborhood factors such as residential segregation by race/ethnicity and socioeconomic position, unequal resource distribution, environmental exposures, poor quality of the built environment (for example, housing quality), violence and safety concerns, and social cohesion have been used to characterize these area-level influences on health.11 Using U.S Census data, it is possible to assemble multiple measured neighborhood characteristics and create an aggregate, cohesive measure of neighborhood deprivation.13 Neighborhood deprivation has been shown to be associated with a multitude of health outcomes, and cardiovascular disease is no exception. For example, residing in a deprived neighborhood is associated with increased odds of prevalent obesity, 14–17weight gain, 18low HDL, 17hypertension, 17elevated fasting glucose,17 venous thromboembolism,19 smoking,16 and inflammatory markers.17 More specifically, neighborhood social deprivation has been associated with higher cardiovascular disease mortality.20 Previous studies suggest that cumulative exposure of greater than 11 years to neighborhoods of high deprivation increases the likelihood of developing obesity and associated cardiovascular risks such as HTN.14 While this evidence is compelling, these studies have been largely cross-sectional,16,21–24 taken place outside of the US,16,19,23 or employed limited measures to characterize deprivation.16,22,24,25
Of the few longitudinal studies that have investigated neighborhood deprivation and HTN, none have accounted for the impact of moving on study populations. Moving status is an important covariate as it permits observation of changes in health status following alterations in the environment (i.e. residential neighborhood).26 Without accounting for moving status, it becomes challenging to claim a relationship between exposure and outcome, as the exposure itself has changed. Another limitation of previous work is failure to include perceptions of neighborhood environment, which are not well correlated to objective measures and therefore may elucidate the true associations between neighborhood environment and cardiovascular health. It is possible that residents’ perceptions may outweigh the influence of objective neighborhood qualities in some instances.27,28 Therefore, using data from the Dallas Heart Study, we endeavor to comprehensively detail neighborhood deprivation, including the influence of both moving and resident perception, and its association with hypertension prevalence, changes in blood pressure, and incident HTN between 2000 and 2009. We will also characterize our findings based on prior and new (2017) HTN guidelines to illustrate the impact of the change in definition, which has not been done previously.
Methods
Dallas Heart Study (DHS)
The DHS is composed of a multi-ethnic cohort of Dallas County residents ages 18–65 years at baseline and is designed to study cardiovascular disease risk and outcomes. Probability sampling was used to establish the cohort, and African Americans were intentionally oversampled to comprise 50% of the study cohort. This was done to ensure a sufficient cohort of African Americans for analyses by race/ethnicity. Baseline data collection took place from 2000–2002. Detailed data collection methods have been previously published.29 Briefly, participants were asked to attend a visit at the University of Texas (UT) Southwestern Medical Center. In the baseline cohort, 6101 participants completed the interview visit, including a detailed survey of medical history and health behaviors, while 3072 completed the laboratory evaluation and physical examination. Follow up examination was completed between September 2007 and December 2009, with a median follow up time of 7 years. Median follow up time was calculated based on exact visit dates for those who returned for the follow-up visit (N=2485). The DHS protocol was approved by the UT Southwestern Medical Center’s Institutional Review Board (IRB); all study participants provided written informed consent at entry and follow-up. A protocol for DHS neighborhood environment data analyses (13-H-N041) was approved by the IRB of the National Heart, Lung, and Blood Institute of the National Institutes of Health.
The Powell-Wiley research group is funded by the Division of Intramural Research of the National Heart, Lung, and Blood Institute at the National Institutes of Health. This research is also supported by the National Institutes of Health Undergraduate Scholarship Program via funding for Joel Adu-Brimpong and the U.S. Health Resources and Services Administration (HRSA), D34HP16299 (Dr. Marquetta Faulkner, PI) for Alnesha Banks. Sophie E. Claudel is supported by the NIH Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and generous contributions to the Foundation for the NIH from the Doris Duke Charitable Foundation, the American Association for Dental Research the Colgate-Palmolive Company, Genentech, Elsevier, and other private donors. The DHS was funded by a grant from the Donald W. Reynolds Foundation. This work was also supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR001105 to the University of Texas Southwestern Medical Center. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; the U.S. Department of Health and Human Services or HRSA. The authors are solely responsible for the design and conduct of this study, all study analyses and drafting and editing of the paper.
Study Definitions
Medical histories and demographic data, including age, sex, race/ethnicity, household income, achieved education, and smoking status were collected via self-report. Specifically, participants were asked to select an income group (in ranges of $5000) that best represented their total combined family income in the past year. For educational achievement, participants were asked to select their highest attained grade-level or number of years of post-secondary education. Tobacco use was assessed through questions including lifetime use of greater than 100 cigarettes, cigarette use in the past 30 days, age of smoking onset, pack history and quitting attempts. Participants were also asked to self-report their length of residence in their neighborhood. Body mass index (BMI) was calculated based on measured height (m) and weight (kg). HTN was defined by either: self-report, the use of anti-hypertensive medication, measured SBP > 140 mmHg and/or DBP > 90 mmHg at baseline, or measured SPB > 130 mmHg and/or DBP > 80 mmHg at follow-up per the 2017 American Heart Association hypertension guidelines.1 Blood pressure was measured using an automatic oscillo etric device (Series #52,000, Welch Allyn, Inc., Arden, North Carolina), as described previously.29 Physical activity measurements at baseline and follow-up were obtained via self-reported leisure-time physical activity. A validated conversion scale for activity intensity was used to compute METs-minutes per week.30
Neighborhood Deprivation Index
A block group-level neighborhood deprivation index (NDI) was developed for geocoded address data from the DHS cohort using 21 variables from the 2000 U.S. Census.31 These 21 variables are believed to contribute to neighborhood deprivation and were selected from six primary domains: education, employment/occupation, housing conditions, income/poverty, racial composition, and residential stability. Through principal components factor analysis, six variables were found to be relevant to neighborhood deprivation in the DHS population. These variables were selected based on meeting the criterion of having a factor loading score greater than 0.40. They are: percent unemployment, percent female-headed households, percent households on public assistance, percent households with a car, percent population below the federal poverty line, and percent non-Hispanic blacks. Following identification of the variables for inclusion in the NDI, the variables were weighted and standardized by their factor loading coefficients. The resulting NDI was then standardized to a mean value of 0 with a standard deviation of 1. Therefore, the greater the score, the more deprived the neighborhood.21,13 In subsequent analyzes, NDI was examined as a categorical variable divided into tertiles. Grouping the population into tertiles of NDI (low, medium, and high deprivation) allows for group-level comparison that may not be perceived through minute changes in the continuous variable.
Neighborhood Perception Score
To assess neighborhood environment perceptions, participants responded to questions abstracted from the Project on Human Development in Chicago Neighborhoods.32 These questions included indicators of social cohesion, feelings of safety, criminal activity, and physical environment characteristics, including access to resources. An overall neighborhood perception score was computed based on the Likert-scale responses, with a higher score representing more unfavorable perceptions of neighborhood environment. Using principal components factor analysis, neighborhood perception factors were identified and assessed for internal validity using Cronbach’s alpha coefficient, with a value of 0.70 or greater meeting inclusion criteria. Three subgroups, or factors, were identified: physical environment (Cronbach’s a-coefficient=0.82), violence (Cronbach’s a-coefficient=0.84), and social cohesion (Cronbach’s a-coefficient=0.76). As with NDI, a higher score represents more unfavorable perception of the neighborhood environment.
Study Population
Figure 1 demonstrates the selection of study participants. Of the 3072 participants who completed the entire baseline evaluation, including the medical visit with laboratory examination, 2485 participants had follow-up data from a second DHS visit. Of the 2485 participants with follow-up data, we excluded the following groups: those who moved out of Dallas County (n=461); those with missing/inadequate address data after geocoding (n=1); those reporting race/ethnicities other than black, white, or Hispanic (n=33); and those missing blood pressure data (n=1). This resulted in a population of 1989 participants. For the specific analyses of modeling blood pressure change over time and incident HTN, we excluded those with HTN at baseline (n=815), resulting in a population of 1174 participants. Movers were defined as participants who reported a change in residential address between study entry and follow-up. Non-movers were identified based on having the same geocoded address at study entry and follow-up.18 Although it is possible that individuals might have moved within the same residential community and therefore have the same environmental exposures, this method of analysis is standard with longitudinal data.33–36 Those who moved out of Dallas County were excluded from analysis as the study aim was to examine the relationship between Dallas County neighborhood deprivation (based on U.S. Census data) and cardiovascular outcomes.
Figure 1.
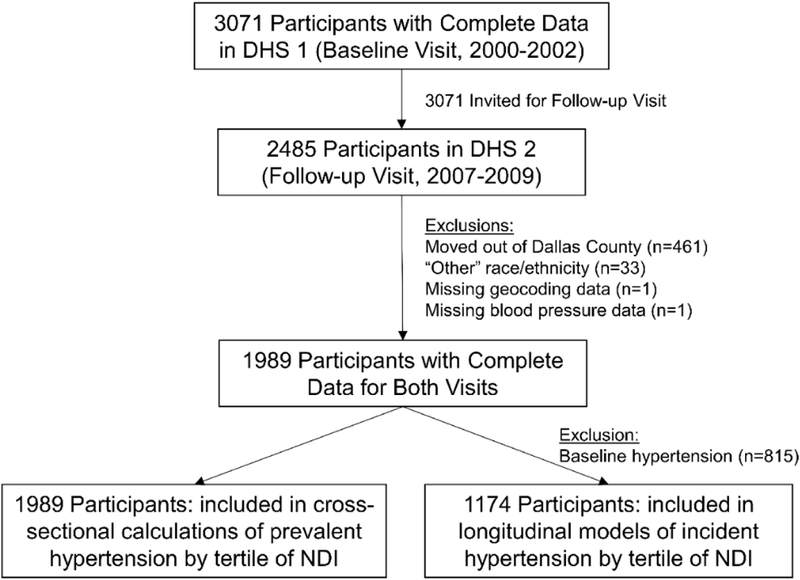
Flow diagram demonstrating selection of the analytic sample.
Statistical Analysis
Neighborhood characteristics included in the development of the NDI were compared across tertiles of neighborhood deprivation using Jonkheere-Terpstra analysis of trend. To cross-sectionally characterize the study population, continuous and categorical variables were also compared across tertiles of neighborhood-level deprivation using the Jonkheere-Terpstra analysis of trend. The cardiometabolic risk factors presented are from the baseline DHS visit.
To evaluate changes in SBP and DBP (mmHg) across tertiles of NDI over time, repeated-measures linear mixed modeling was applied to participants without baseline HTN, as defined by the pre-2017 HTN guidelines (n=1174). Linear mixed modeling was selected because of its ability to model differences in groups accounting for participant random effects. The clustered nature of the participants can be taken into account using a hierarchical model; i.e. participants within the same census block-group can be thought of as being correlated, and this correlation can be accounted for utilizing random effects. Models were adjusted for age, sex, race/ethnicity, smoking status, income, education, BMI, physical activity level, use of antihypertensive medication at follow-up, length of residence in the neighborhood, moving status, and Heckman correction factor. Heckman correction factor is included to account for non-random choice or “self-selection” into improved neighborhoods. Heckman correction factor corrects for bias in non-randomly assigned treatment, such as those participants who are “treated” with an improved neighborhood NDI because they autonomously decided to move neighborhoods. The Heckman correction factor provides reliable causal estimates in the presence of self-selection37 and has been used in prior studies to account for selection bias.38
Logistic regression modeling was used to determine odds of incident HTN by tertile of neighborhood deprivation in those without existing HTN at baseline (as defined by pre-2017 HTN guidelines). Incident HTN was defined using the new, 2017 HTN guidelines. Logistic models were adjusted for age, sex, race/ethnicity, smoking status, income, education, BMI, physical activity, length of neighborhood residence, moving status and Heckman correction factor. Models of blood pressure change and incident HTN were also adjusted for the overall neighborhood perception score and each sub-score of neighborhood perception (physical environment, violence, and social cohesion). Sensitivity analyses including those who moved out of Dallas County were conducted for both the models of change in BP and incident HTN. In these analyses, participants were randomly assigned to have moved to a census tract with a higher, lower, or equal NDI neighborhood in equal proportions.
Results
Neighborhood characteristics for the census tracts included in analysis are shown in Table 1. Significant differences were observed across tertiles of NDI in all variables.
Table 1.
Neighborhood Characteristics by NDI for Census Tracts Included in DHS, US Census 2000
| Overall Sample | Low Deprivation | Medium Deprivation | High Deprivation | p-trend | |
|---|---|---|---|---|---|
| Number of Census Tracts | 261 | 153 | 79 | 29 | |
| Non-Hispanic Black | 22% | 14% | 29% | 41% | <0.0001 |
| Unemployed | 4% | 3% | 5% | 7% | <0.0001 |
| Female Headed Household | 15% | 11% | 17% | 29% | <0.0001 |
| Own a Car | 91% | 95% | 89% | 71% | <0.0001 |
| Family Below Federal Poverty Level | 12% | 6% | 15% | 32% | <0.0001 |
| Individuals Below Federal Poverty Level | 14% | 8% | 17% | 35% | <0.0001 |
| Receive Public Assistance | 3% | 2% | 3% | 9% | <0.0001 |
The study population (n=1989) consisted of 50% non-Hispanic blacks, 30% non-Hispanic whites, and 20% Hispanic whites. Median follow-up time between the study visits was 7 years. Table 2 shows population characteristics at baseline, representing a cross-sectional snapshot of the cohort. The NDI distribution ranged from −1.08 (low deprivation) to 5.83 (high deprivation) (Table 2). Individuals living in higher NDI neighborhoods were more likely to be black, have lower education, lower income, and higher BMI when compared with those living in lower NDI neighborhoods (p trend <0.05 for all). Additionally, residing in neighborhoods in higher NDI tertiles was associated with having higher SBP (124 vs. 128 vs. 132 mmHg, p trend <0.0001) and DBP (78 vs. 79 vs. 82 mmHg, p trend <0.0001) and higher HTN prevalence, based on pre-2017 HTN guidelines (23.4% vs. 35.1% vs. 43.6%, p trend <0.0001) at the baseline visit. Demographic information for the analytic sample (n=1174) is shown in Supplemental Table 1.
Table 2:
Sample Baseline Characteristics by NDI for DHS Participants included in the Final Analyses, 2000–2009 (N=1174)
| Overall Sample | Low Deprivation | Medium Deprivation | High Deprivation | p-trend | |
|---|---|---|---|---|---|
| Sample Size (N) | 1174 | 448 | 386 | 340 | |
| Range of NDI | 1.08 to 5.90 | 1.08 to −0.03 | 0.03 to 1.07 | 1.10 to 5.90 | |
| Age (years), mean (SD) | 40.1 (9.6) | 41.9 (9.6) | 39.0 (9.7) | 38.8 (9.0) | <0.0001 |
| Female Sex, n(%) | 678 (58%) | 239 (53%) | 227 (59%) | 212 (62%) | 0.01 |
| Moved During Study Period, n(%) | 594 (51%) | 159 (35%) | 207 (54%) | 228 (67%) | <0.0001 |
| Race/Ethnicity, n(%) | |||||
| Non-Hispanic Black | 591 (50%) | 68 (15%) | 215 (56%) | 308 (91%) | <0.0001 |
| Non-Hispanic White | 360 (31%) | 297 (66%) | 57 (15%) | 6 (2%) | <0.0001 |
| Hispanic | 223 (19%) | 83 (19%) | 114 (30%) | 26 (8%) | 0.002 |
| Education, n(%) | |||||
| Less than High School | 213 (18%) | 51 (11%) | 87 (23%) | 75 (22%) | <0.0001 |
| High School | 349 (30%) | 87 (19%) | 116 (30%) | 146 (43%) | <0.0001 |
| Some College | 344 (29%) | 135 (30%) | 114 (30%) | 95 (28%) | 0.52 |
| College Degree or higher | 268 (23%) | 175 (39%) | 69 (18%) | 24 (7%) | <0.0001 |
| Annual Income, n(%) | |||||
| <$16,000 | 174 (17%) | 20 (5%) | 48 (15%) | 106 (37%) | <0.0001 |
| $16,000 – $29,999 | 264 (26%) | 68 (17%) | 104 (33%) | 92 (32%) | <0.0001 |
| $30,000 – $49,999 | 256 (25%) | 92 (23%) | 99 (31%) | 65 (23%) | 0.75 |
| $50,000 or higher | 318 (31%) | 224 (56%) | 68 (21%) | 26 (9%) | <0.0001 |
| Cardiometabolic Risk Factors | |||||
| BMI (kg/m2) | 28.5 (6.6) | 27.9 (6.3) | 28.9 (6.8) | 28.9 (6.8) | 0.02 |
| Systolic Blood Pressure (mmHg) | 119 (11) | 118 (11) | 119 (12) | 120 (11) | 0.11 |
| Diastolic Blood Pressure (mmHg) | 75 (7) | 75 (7) | 75 (8) | 76 (7) | 0.11 |
| Prevalent HTN, pre-2017 definition | 0 | 0 | 0 | 0 | 0.003 |
| Prevalent CVD, n(%) | 23 (2%) | 1 (0.2%) | 12 (3%) | 10 (3%) | <0.0001 |
| Physical Activity (MET-mins/week), mean (SD) | 495.5 (870.3) | 593.4 (958.5) | 469.6 (920.0) | 402.6 (661.7) | <0.0001 |
| Current Smokers, n(%) | 296 (25%) | 90 (20%) | 88 (23%) | 118 (35%) | |
| Neighborhood Perception Score | |||||
| Total NPS | 29.3 (11.0) | 25.2 (8.6) | 29.1 (9.9) | 35.0 (12.5) | <0.0001 |
| Violence (Factor 1) | 8.8 (4.6) | 7.5 (3.8) | 8.6 (4.1) | 10.9 (5.4) | <0.0001 |
| Physical Environment (Factor 2) | 12.9 (6.3) | 10.7 (4.8) | 12.8 (6.0) | 15.9 (7.0) | <0.0001 |
| Social Cohesion (Factor 3) | 7.5 (3.2) | 6.95 (2.8) | 7.68 (3.2) | 8.17 (3.7) | <0.0001 |
Note: NDI = Neighborhood Deprivation Index; SD = Standard Deviation; BMI = Mass Index; HTN = Hypertension; CVD = Cardiovascular Disease; NPS = Neighborhood Perception Score
Higher tertile of NDI was associated with statistically significant increases in SBP and DBP among study participants without prevalent HTN (Table 3). In the unadjusted models, neighborhood deprivation was associated with increased blood pressure for both medium deprivation (SBP: β=4.18, SE=1.25, p=0.0009; BDP: β=2.14, SE=0.62, p<0.0001) and high deprivation (SBP: β=7.56, SE=1.46, p=<0.0001; DBP: β=4.24, SE=0.66, p=0.0006). After adjusting for age, sex, race, income, education, smoking status, physical activity, BMI, use of anti-hypertensive medications at follow-up, years in the neighborhood, moving status, and Heckman correction factor, the relationship between NDI and blood pressure remained significant for both medium (SBP: β=4.54, SE=1.35, p=0.0008; DBP: β=2.51, SE=0.70, p=0.0004) and high deprivation (SBP: β=7.33, SE=1.52, p<0.0001; DBP: β=4.51, SE=0.77, p<0.0001). Additional adjustments for overall neighborhood perception did not attenuate the relationship for either medium (SBP: β=4.81, SE=1.39, p=0.0005; DBP: β=2.61, SE=0.71, p=0.0003) or high deprivation (SBP: β=7.64, SE=1.55, p<0.0001; DBP: β=4.64, SE=0.78, p<0.0001). Similarly, no significant changes were observed in the model following adjustment for individual components of the overall neighborhood perception score (physical environment, violence, and social cohesion) (Supplemental Table 2).
Table 3.
Changes in Systolic and Diastolic Blood Pressures (BP) by Tertile of NDI for the DHS Population, 2000–2009 (N=1174)
| Unadjusted | Model 1* | Model 2† | ||||
|---|---|---|---|---|---|---|
| Estimate (SE) | p-value | Estimate (SE) | p-value | Estimate (SE) | p-value | |
| Systolic BP | ||||||
| Low NDI (ref) | ||||||
| Medium NDI | 4.18 (1.25) | 0.0009 | 4.54 (1.35) | 0.0008 | 4.81 (1.39) | 0.0005 |
| High NDI | 7.56 (1.46) | <0.0001 | 7.33 (1.52) | <0.0001 | 7.64 (1.55) | <0.0001 |
| Diastolic BP | ||||||
| Low NDI (ref) | ||||||
| Medium NDI | 2.14 (0.62) | 0.0006 | 2.51 (0.70) | 0.0004 | 2.61 (0.71) | 0.0003 |
| High NDI | 4.24 (0.66) | <0.0001 | 4.51 (0.77) | <0.0001 | 4.64 (0.78) | <0.0001 |
Note: Referent (ret) = Low NDI; SE = standard error
Model 1: Adjusted for age, sex, race, income, education, smoking, physical activity, BMI, use of anti-hypertensive medications at follow-up, years in neighborhood, moving status, and Heckman correction factor.
Model 2: Adjusted for Model 1 covariates and total perceptions of neighborhood environment (violence, physical environment, and social cohesion)
As expected, living in areas of higher neighborhood deprivation was associated with higher odds of developing HTN during the follow up period (Table 4). Table 4 demonstrates the odds of incident HTN during the study period based on the use of either pre-2017 or current (2017) HTN guidelines. In unadjusted models using either definition of HTN, those living in areas of both medium and high deprivation were more likely to develop HTN. However, with additional adjustment for covariates, using the pre-2017 diagnostic cutoff for HTN resulted in non-significant estimates. Using the 2017 HTN guidelines, participants living in areas of high deprivation were more likely to develop incident HTN in all models. For example, in the fully adjusted model of high deprivation, participants had 1.69 higher odds of developing HTN (OR 1.69; 95% Cl 1.02, 2.82). Similarly, no significant differences were observed following adjustment for individual components of the overall neighborhood perception score (physical environment, violence, and social cohesion) (Supplemental Table 3). Finally, the 95% confidence intervals for the high deprivation groups between the models (pre-2017 vs. 2017 guidelines) overlap.
Table 4.
Estimated Odds Ratios (OR) and 95% Confidence Intervals (Cl) of Incident Hypertension at Follow-Up by Tertile of NDI for the DHS Population Population, 2000–2009 (N=1174)
| Unadjusted | Model 1* | Model 2† | ||||
|---|---|---|---|---|---|---|
| OR | OR 95% CI | OR | 95% CI | OR | 95% CI | |
| Pre-2017 Hypertension Guidelines | ||||||
| Low NDI (ref) | 1.00 | 1.00 | 1.00 | |||
| Medium NDI | 1.62 | 1.14, 2.28 | 1.35 | 0.88, 2.07 | 1.32 | 0.87, 2.00 |
| High NDI | 2.35 | 1.64, 3.37 | 1.77 | 1.08, 2.90 | 1.66 | 1.00, 2.79 |
| 2017 Hypertension Guidelines | ||||||
| Low NDI (ref) | 1.00 | 1.00 | 1.00 | |||
| Medium NDI | 1.51 | 1.09, 2.09 | 1.47 | 0.98, 2.21 | 1.42 | 0.94, 2.14 |
| High NDI | 2.03 | 1.42, 2.89 | 1.85 | 1.13, 3.02 | 1.69 | 1.02, 2.82 |
Note: Referent = Low NDI; OR = odds ratio; Cl = confidence interval
Model 1: Adjusted for age, sex, race, income, education, smoking, physical activity, BMI, years in neighborhood, moving status, and Heckman correction factor.
Model 2: Adjusted for Model 1 covariates and total perceptions of neighborhood environment (violence, physical environment, and social cohesion).
Results of the sensitivity analyses were consistent with the main study findings (data not shown).
Discussion
This study adds to the discussion of combatting cardiovascular disease by focusing on the effects of exposure to a deprived neighborhood environment. First, it corroborates existing cross-sectional evidence by demonstrating higher blood pressure and HTN prevalence at baseline within areas of high deprivation. Second, to our knowledge, it is the first to show a longitudinal relationship between neighborhood deprivation and incident HTN while controlling for movement between neighborhoods and residents’ perception of the environment. Furthermore, this study is one of the first to assess the impact of the new 2017 definitions of HTN in clinical epidemiologic research.
Changing the definition of HTN has powerful implications for both healthcare practitioners and patients. The instantaneous rise in the prevalence of HTN due to the new guidelines may leave clinicians wondering at how to handle a vastly increased patient load, nearly 50% of the US population.39 Simultaneously, patients may be unaware of the implications of the updated definition, such as the need for treatment. Understanding the impact of neighborhood deprivation may assist in developing policies aimed at treating these newly classified hypertensive patients on a broad scale. In the context of this study, the results suggest the potential for differences in the magnitude of the effects based on the definition of HTN used, although we were unable to demonstrate statistical differences. This highlights that further work is warranted to discern the full impact of the updated HTN guidelines.
As evidence regarding neighborhood deprivation and HTN has been conflicting in the past, the longitudinal perspective we present is particularly relevant to untangling the relationship. Our study is one of the first longitudinal analyses to illustrate the relationship between neighborhood deprivation and incident HTN, independent of confounders. For example, while Diez-Roux and colleagues were able to demonstrate changes in blood pressure and HTN incidence across neighborhood socioeconomic status during a 9-year period, the authors acknowledge the confounding effect of age and prior life events in their cohort, which was significantly older at baseline.40 As we are able to control for age in this study and had a broad range of ages represented, we can be slightly more confident that the higher HTN incidence observed in individuals living in more deprived neighborhoods is due to neighborhood conditions. However, we acknowledge that we were also unable to account for prior life events in this study.
By showing a significant relationship between blood pressure and measures of neighborhood deprivation, which includes factors pertaining to the physical environment, this study adds to the existing literature regarding the potential importance of improvements in the built environment on HTN development. Kershaw et al showed that moving from a highly segregated to a less-segregated neighborhood led to a significant drop in blood pressure among African Americans, but did not explore other neighborhood-level factors that may have contributed to the observed changes in blood pressure.41 The exact mechanism between neighborhood deprivation and HTN is not clearly understood, but several hypotheses exist. Individuals living in areas of greater deprivation may face greater social stressors, leading to alterations in cortisol regulation.17 Alternatively, these individuals may have fewer nutritional resources, leading to increased sodium intake and subsequent HTN.42 To compound these influences, deprived neighborhoods may have lower walkability and perceived safety, leading to decreased physical activity and increased sedentary time. Taken together, these findings suggest population-based HTN intervention efforts in low-resource, socioeconomically deprived communities may benefit from improved changes in the built environment, including access to community resources.
The clinical and economic implications of this study cannot be ignored. In the U.S., cardiovascular disease is the leading cause of death and costs an approximate $555 billion annually in combined medical care and lost productivity.43 Costs are expected to reach $1.1 trillion annually by 2035.43 Therefore, identifying and acting on modifiable risk factors, such as neighborhood environment, is critical to both improving health outcomes and reducing the financial burden of treatment on both individual patients and the health economy of the United States. While combatting neighborhood influences may seem beyond the scope of clinical practice for cardiologists and family practitioners, understanding the forces at play in a patients’ disease course may enable discussion regarding health behaviors, such as physical activity, within a deprived environment.
Strengths and Limitations
Our study exhibits several strengths. First, we compared both the old and new HTN guidelines in a clinically relevant setting, using objectively measured SBP and DBP. Second, we studied a bi-racial, urban cohort that is more representative than the traditionally homogenous, Caucasian samples. Third, longitudinal analyses allowed us to follow blood pressure changes over time, which is not possible in cross-sectional studies. Finally, we were able to control for different components of the neighborhood environment, which enabled us to specifically observe potential mediating factors in the relationship between deprivation and HTN.
The limitations of this study are also recognized. We were unable to account for changes in anti-hypertensive medications during the interim study period, which may have affected the results. We were unable to assess moving status in the interim study period, as we only had access to geocoded addresses at the baseline and follow-up visits. Therefore, we may not have been able to adequately capture the effect of moving multiple times or exposure to several different environments. In some cases, individual socio-demographic factors such as education, income, and neighborhood composition may have influenced residential selection among participants leading to bias in our results. However, we accounted for neighborhood self-selection by including the Heckman correction factor in all models. In this study, the same participants both rated the neighborhood environment and were included as patients with blood pressure measurements. Future studies should consider engaging separate individuals within the same community to provide the neighborhood assessment and capture the independent effect of neighborhood on HTN. Our study was also limited due to our inability to stratify by race and gender, which may have revealed different group-level trends, due to lack of statistical power. We were also unable to investigate whether development of HTN lead to further cardiovascular events, such as stroke or myocardial infarction. Finally, as the study was restricted to Dallas County, we cannot assume generalizability to the broader U.S population.
Conclusions
Our study adds to the small but nascent literature on the effects of neighborhood deprivation on HTN incidence, especially in the U.S. The findings suggest that public policy targeting neighborhood-level factors, such as the neighborhood physical environment and available community resources, within Dallas County may be beneficial in improving the cardiovascular health of residents. While improvements to sidewalks, food resources, and recreational areas may substantially improve cardiovascular health, it is equally important for physicians to recognize the context in which their patients are developing HTN and associated cardiovascular risks.
Supplementary Material
Highlights.
More deprived neighborhoods are associated with higher baseline blood pressure.
Living in deprived neighborhoods is associated with worsening blood pressure.
Living in deprived neighborhoods results in higher odds of incident hypertension.
New hypertension guidelines may have broad impact on clinical epidemiology.
Targeting neighborhood factors may be beneficial in improving the heart health.
Acknowledgments
Funding: The Powell-Wiley research group is funded by the Division of Intramural Research of the National Heart, Lung, and Blood Institute at the National Institutes of Health. This research is also supported by the National Institutes of Health Undergraduate Scholarship Program via funding for Joel Adu-Brimpong and the U.S. Health Resources and Services Administration (HRSA), D34HP16299 (Dr. Marquetta Faulkner, PI) for Alnesha Banks. Sophie E. Claudel is supported by the NIH Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and generous contributions to the Foundation for the NIH from the Doris Duke Charitable Foundation, the American Association for Dental Research, the Colgate-Palmolive Company, Genentech, Elsevier, and other private donors. The DHS was funded by a grant from the Donald W. Reynolds Foundation. This work was also supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR001105 to the University of Texas Southwestern Medical Center. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; the U.S. Department of Health and Human Services or HRSA. The authors are solely responsible for the design and conduct of this study, all study analyses and drafting and editing of the paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: none.
References
- 1.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practic. Hypertension. 2017. doi: 10.1161/HYP.0000000000000065/-/DC1.The. [DOI] [Google Scholar]
- 2.Russell RWR. How Does Blood Pressure Cause Stroke? Lancet. 1975;306(7948):1283–1285. [DOI] [PubMed] [Google Scholar]
- 3.Kannel WB, Wolf PA, Verter J, McNamara PM. Framingham Study Insights on the Hazards of Elevated Blood Pressure. JAMA. 1970;214(2):301–310. [PubMed] [Google Scholar]
- 4.Suchy-Dicey AM, Wallace ER, Mitchell SVE, et al. Blood pressure variability and the risk of all-cause mortality, incident myocardial infarction, and incident stroke in the cardiovascular health study. Am J Hypertens. 2013;26(10):1210–1217. doi: 10.1093/ajh/hpt092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agarwal R Blood Pressure Components and the Risk for End-Stage Renal Disease and Death in Chronic Kidney Disease. Clin J Am Soc Nephrol. 2009;4(4):830–837. doi: 10.2215/CJN.06201208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mujahid MS, Diez Roux AV, Cooper RC, Shea S, Williams DR. Neighborhood stressors and race/ethnic differences in hypertension prevalence (the Multi-Ethnic Study of Atherosclerosis). Am J Hypertens. 2011;24(2):187–193. doi: 10.1038/ajh.2010.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mujahid MS, Diez-Roux AV., Morenoff JD, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008;19(4):590–598. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- 8.Kaiser P, Diez Roux AV., Mujahid M, et al. Neighborhood Environments and Incident Hypertension in the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2016;183(11):988– 997. doi: 10.1093/aje/kwv296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halonen JI, Stenholm S, Pentti J, et al. Childhood psychosocial adversity and adult neighborhood disadvantage as predictors of cardiovascular disease: A cohort study. Circulation. 2015;132(5):371–379. doi: 10.U61/CIRCULATIONAHA.U5.015392. [DOI] [PubMed] [Google Scholar]
- 10.Diez Roux AV Residential Environments and Cardiovascular Risk. J Urban Heal. 2003;80(4):569– 589. doi: 10.1093/jurban/jtg065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diez Roux AV, Mair C, Roux AVD, Mair C, Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y AcadSci. 2010;1186(1):125–145. doi: 10.UU/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 12.Ben-Shlomo Y, White IR, Marmot M. Does the variation in the socioeconomic characteristics of an area affect mortality? Bmj. 1996;312(7037):1013–1014. doi: 10.1136/bmj.312.7037.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Heal. 2006;83(6):1041–1062. doi: 10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Powell-Wiley TM, Ayers C, Agyemang P, et al. Neighborhood-Level Socioeconomic Deprivation Predicts Weight Gain in a Multi-Ethnic Population: Longitudinal Data from the Dallas Heart Study. Prev Med (Baltim). 2014;66:22–27. doi: 10.1016/j.neuron.2009.10.017.A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Powell-Wiley TM, Ayers CR, de Lemos JA, et al. Relationship between perceptions about neighborhood environment and prevalent obesity: data from the Dallas Heart Study. 2013;21(1):e14–21. doi:doi: 10.1002/oby.20012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cubbin C, Sundquist K, Ahlen H, Johansson SE, Sundquist J, Winkleby MA. Neighborhood deprivation and cardiovascular disease risk factors: Protective and harmful effects. Scand J Public Health. 2006;34(3):228–237. doi: 10.1080/14034940500327935. [DOI] [PubMed] [Google Scholar]
- 17.Keita AD, Judd SE, Howard VJ, Carson AP, Ard JD, Fernandez JR. Associations of neighborhood area level deprivation with the metabolic syndrome and inflammation among middle- and older- age adults. BMC Public Health. 2014;14(1):1319. doi: 10.1186/1471-2458-14-1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powell-Wiley TM, Cooper-McCann R, Ayers C, et al. Change in Neighborhood Socioeconomic Status and Weight Gain: Dallas Heart Study. Am J Prev Med. 2015;49(1):72–79. doi: 10.1038/nmeth.2839.A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zoller B, Li X, Sundquist J, Sundquist K. Neighborhood deprivation and hospitalization for venous thromboembolism in Sweden. J Thromb Thrombolysis. 2012;34(3):374–382. doi: 10.1007/s11239-012-0728-4. [DOI] [PubMed] [Google Scholar]
- 20.Ford MM, Highfield LD. Exploring the spatial association between social deprivation and cardiovascular disease mortality at the neighborhood level. PLoS One. 2016;11(1):1–17. doi: 10.1371/journal.pone.0146085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laraia BA, Karter AJ, Warton EM, Schillinger D, Moffet HH, Adler N. Place matters: neighborhood deprivation and cardiometabolic risk factors in the Diabetes Study of Northern California (DISTANCE). SocSciMed. 2012;74(7):1082–1090. doi: 10.1016/j.socscimed.2011.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chaix B, Bean K, Leal C, et al. Individual/neighborhood social factors and blood pressure in the record cohort study: Which risk factors explain the associations? Hypertension. 2010;55(3):769– 775. doi: 10.1161/HYPERTENSIONAHA.109.143206. [DOI] [PubMed] [Google Scholar]
- 23.Matheson FI, White HL, Moineddin R, Dunn JR, Glazier RH. Neighbourhood chronic stress and gender inequalities in hypertension among Canadian adults: A multilevel analysis. J Epidemiol Community Health. 2010;64(8):705–713. doi: 10.1136/jech.2008.083303. [DOI] [PubMed] [Google Scholar]
- 24.Chaix B, Ducimetiere P, Lang T, et al. Residential environment and blood pressure in the PRIME Study: Is the association mediated by body mass index and waist circumference? J Hypertens. 2008;26(6): 1078–1084. doi: 10.1097/HJH.0b013e3282fd991f. [DOI] [PubMed] [Google Scholar]
- 25.Vijayaraghavan M, Kushel MB, Vittinghoff E, et al. Housing instability and incident hypertension in the CARDIA cohort. J Urban Heal. 2013;90(3):427–441. doi: 10.1007/sll524-012-9729-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boone-Heinonen J, Gordon-Larsen P, Guilkey DK, Jacobs DR, Popkin BM. Environment and physical activity dynamics: the role of residential self-selection. Psychol Sport Exerc. 2011;12(l):54–60. doi: 10.1016/j.psychsport.2009.09.003.Environment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Franzini L, Caughy MO, Nettles SM, O’Campo P. Perceptions of disorder: contributions of neighborhood characteristics to subjective perceptions of disorder. J Environ Psychol. 2008;28:83–93. [Google Scholar]
- 28.Ahuja C, Ayers C, Hartz J, et al. Examining relationships between perceptions and objective assessments of neighborhood environment and sedentary time: Data from the Washington, D.C. Cardiovascular Health and Needs Assessment. Prev Med Reports. 2018;9(November 2017):42–48. doi: 10.1016/j.pmedr.2017.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Victor RG, Haley RW, Willett DL, et al. The Dallas Heart Study: a population-based probability sample for the multidisciplinary study of ethnic differences in cardiovascular health. Am J Cardiol. 2004;93(12):1473–1480. doi: 10.1016/j.amjcard.2004.02.058. [DOI] [PubMed] [Google Scholar]
- 30.LaMonte MJ, Durstine JL, Addy CL, Irwin ML, Ainsworth BE. Physical activity, physical fitnes, and Framingham 10-year risk score: the cross-cultural activity participation study. J Cardiopulm Rehabil. 2001;21(2):63–70. [DOI] [PubMed] [Google Scholar]
- 31.Lian M, Struthers J, Liu Y. Statistical Assessment of Neighborhood Socioeconomic Deprivation Environment in Spatial Epidemiologic Studies. Open J Stat. 2016;6(3):436–442. doi: 10.4236/ojs.2016.63039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science (80-). 1997;277(5328):918–924. [DOI] [PubMed] [Google Scholar]
- 33.Wing JJ, August E, Adar SD, et al. Change in Neighborhood Characteristics and Change in Coronary Artery Calcium: A Longitudinal Investigation in the MESA (Multi-Ethnic Study of Atherosclerosis) Cohort. Circulation. 2016;134(7):504–513. doi: 10.1161/CIRCULATIONAHA.115.020534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Powell-Wiley TM, Moore K, Allen N, et al. Associations of Neighborhood Crime and Safety and with Changes in Body Mass Index and Waist Circumference: The Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2017. doi: 10.1093/aje/kwx082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kerr Z, Evenson KR, Moore K, Block R, Diez-Roux AV. Changes in walking associated with perceived neighborhood safety and police-recorded crime: the Multi-Ethnic Study of Atherosclerosis. Prev Med (Baltim). 2015;73:88–93. doi: 10.1002/nbm.3369.Three. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boone-Heinonen J, Roux AVD, Kiefe CI, Lewis CE, David K, Gordon-larsen P. Neighborhood socioeconomic status predictors of physical activity through young to middle adulthood: The CARDIA Study. Soc Sci Med. 2011;72(5):641–649. doi: 10.1016/j.socscimed.2010.12.013.Neighborhood. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heckman JJ. Sample Selection Bias as a Specification Error. Econometrica. 1979;47(1):153–161. doi: 10.3982/ECTA9859. [DOI] [Google Scholar]
- 38.Leonard T, Ayers C, Das SR, Neeland IJ, Powell-Wiley TM. Do neighborhoods matter differently for movers and non-movers? Analysis of weight gain in the longitudinal Dallas Heart Study. Heal Place. 2017;44(May 2016):52–60. doi: 10.1016/j.healthplace.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.AHA. Nearly half of US adults could now be classified with high blood pressure, under new definitions. AHA News. https://news.heart.org/nearly-half-u-s-adults-now-classified-high-blood-pressure-new-definitions/. Published 2017.
- 40.Diez Roux AV, Chambless L, Merkin SS, et al. Socioeconomic disadvantage and change in blood pressure associated with aging. Circulation. 2002;106(6):703–710. doi: 10.1161/01.CIR.0000025402.84600.CD. [DOI] [PubMed] [Google Scholar]
- 41.Kershaw KN, Robinson WR, Gordon-Larsen P, et al. Association of changes in neighborhood-level racial residential segregation with changes in blood pressure among black adults: The CARDIA study. JAMA Intern Med. 2017;177(7):996–1002. doi: 10.1001/jamainternmed.2017.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gutierrez OM. Contextual poverty, nutrition, and chronic kidney disease. Adv Chronic Kidney Dis. 2015;22(1):31–38. doi: 10.1053/j.ackd.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.AHA. Cardiovascular Disease: a Costly Burden for America - Projections Through 2035. AHA Assoc CVD Burd Rep. 2017. doi:1/17DS11775. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


