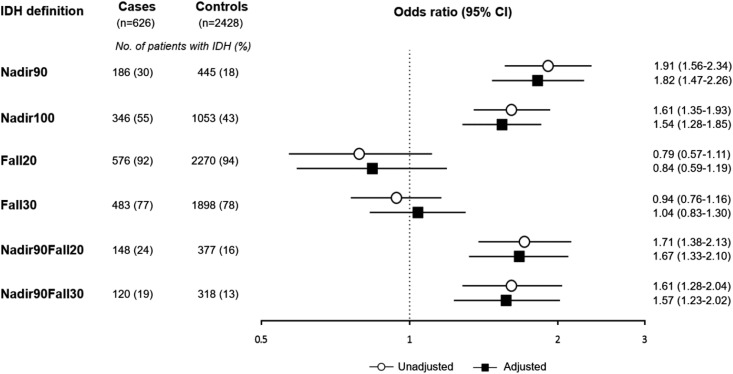
Figure 3.
Odds of intradialytic hypotension (defined in six ways) among cases of hospitalized mesenteric ischemia and matched controls.Cases had a nearly two-fold higher odds of having had intradialytic hypotension in the 30 days before the index date compared with controls, when using a nadir-based IDH definition (i.e., Nadir90, Nadir100, Nadir90Fall20, and Nadir90Fall30). However, when using the two definitions that used the change in SBP (i.e., Fall20 and Fall30), there was no significant association of intradialytic hypotension and mesenteric ischemia. Adjustment for demographic and clinical factors did not significantly change the associations. Adjusted indicates adjusted for cause of ESKD, number of non-nephrology outpatient visits, hospital days, any nursing home stay, on the kidney transplant waiting list, all comorbidities, mean ultrafiltration rate, and central venous catheter use. 95% CI, 95% confidence interval; Fall20, (predialysis SBP – nadir intradialytic SBP) ≥20 mm Hg; Fall30, (predialysis SBP – nadir intradialytic SBP) ≥30 mm Hg; Nadir90, nadir intradialytic SBP <90 mm Hg; Nadir100, nadir intradialytic SBP <100 mm Hg; Nadir90Fall20, nadir intradialytic SBP <90 mm Hg and (predialysis SBP – nadir intradialytic SBP) ≥20 mm Hg; Nadir90Fall30, nadir intradialytic SBP <90 mm Hg and (predialysis SBP – nadir intradialytic SBP) ≥30 mm Hg.