Abstract
Background and Objectives:
No previous study has compared different concentrations of lignocaine for topical anesthesia during endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA). In this pilot study, we compared 1% versus 2% lignocaine for topical airway anesthesia during EBUS-TBNA.
Methods:
In this double-blind, randomized trial, subjects were randomized to receive either 1% or 2% lignocaine for “spray-as-you-go” administration. All received combined moderate intravenous sedation (midazolam and fentanyl). Ten percent pharyngeal lignocaine spray (two sprays) and nebulized lignocaine (2.5 ml of 4% solution) were administered to all subjects. Administration of additional lignocaine was allowed at operator's discretion. The primary endpoints were operator-rated overall procedural satisfaction and cough, each assessed on visual analog scale (VAS), while the secondary outcomes included patient-rated faces pain scale scores, cumulative lignocaine dose, number of subjects receiving lignocaine >8.2 mg/kg, doses of midazolam/fentanyl between groups, and adverse events during procedure.
Results:
The mean (standard deviation [SD]) VAS scores for operator-rated procedure satisfaction were 64.2 (25.6) and 68.7 (23.7) in 1% and 2% group, respectively (P = 0.35). The median (interquartile range) VAS scores for operator-rated cough were 48.4 (23.9–69.9) in 1% group and 38.7 (18.6–69.5) in 2% group (P = 0.24). The mean [SD] cumulative lignocaine received in the 2% lignocaine group (248.6 [29.1] mg) was significantly greater than in 1% lignocaine group (178.5 [14.6] mg) (P < 0.01).
Conclusion:
One percent lignocaine is equally efficacious as 2% lignocaine for topical anesthesia during EBUS-TBNA, at a significantly lower cumulative lignocaine dose.
KEY WORDS: Anesthesia, bronchoscopy, endobronchial ultrasound-guided transbronchial needle aspiration, lignocaine
INTRODUCTION
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is a firmly established modality for the evaluation of mediastinal lymphadenopathy. It has evolved into the initial investigation modality of choice for histologic sampling of the mediastinum in lung cancer staging.[1]
EBUS-TBNA is usually performed under moderate sedation with the administration of lignocaine for topical anesthesia.[1,2] It can also be performed under deep sedation or general anesthesia. Two large randomized controlled trials (RCTs) comparing 1% versus 2% lignocaine concentrations during flexible bronchoscopy (most procedures performed without sedation) have demonstrated equal efficacy of both concentrations for procedural satisfaction and cough suppression.[3,4] Performance of EBUS-TBNA with exclusive use of topical anesthesia is uncommon.[5] The available guidelines and expert panel report on technical aspects of EBUS-TBNA do not clarify the optimum lignocaine concentration for topical anesthesia during the procedure.[2] While the British Thoracic Society guidelines recommend the use of 1% lignocaine for flexible bronchoscopy, there are no recommendations for EBUS-TBNA.[6] Some groups have advocated the use of 2% lignocaine during EBUS-TBNA.[7]
We hypothesized that the larger diameter of the EBUS bronchoscope may be associated with differing topical airway anesthesia requirements as compared with flexible bronchoscopy. In contrast with flexible bronchoscopy, close and prolonged mucosal contact is often necessary to obtain optimum ultrasonic images, there is frequent scope contact near the carinal region, and the procedure duration is generally longer. No previous studies have compared 1% versus 2% lignocaine concentrations for topical anesthesia during EBUS-TBNA. We conducted this pilot RCT to determine if 1% lignocaine solution is as effective as 2% lignocaine for providing topical airway anesthesia during EBUS-TBNA.
METHODS
Study design
This was an investigator-initiated, randomized, double-blind, active comparator trial comparing 1% versus 2% lignocaine solution delivered using spray-as-you-go method, for topical anesthesia during EBUS-TBNA. The study protocol was approved by the Institute Ethics Committee (IECPG-254). The trial was registered in the Clinical Trial Registry, www.clinicaltrials.gov NCT02913300. Written informed consent was obtained from all subjects before randomization.
Participants and randomization
Consecutive subjects aged 18 years or more and planned for EBUS-TBNA willing for participation were randomized in a 1:1 ratio to either 1% or 2% lignocaine groups. Randomization was computer generated and sealed envelopes were used for allocation. The exclusion criteria were subjects undergoing EBUS-TBNA under general anesthesia, subjects with significant hypoxemia at baseline (pulse oximetry saturation <92% while breathing oxygen FiO2 >0.3), hemodynamically unstable subjects (systolic blood pressure [BP] >180 or diastolic BP >90 mmHg), subjects with known previous documented allergic reaction to lignocaine, pregnancy, and advanced renal or hepatic dysfunction.
Study procedures
Subjects were asked to report fasting (nil oral for solids 6 h before the procedure). Baseline parameters including heart rate, BP, and pulse oximetry saturation were recorded. A peripheral venous access was secured and low flow oxygen was administered through nasal prongs. Subjects in both the groups were prepared in a similar fashion, except for the concentration of lignocaine solution used for “spray-as-you-go” technique. Subjects were initially nebulized with 2.5 ml of 4% lignocaine solution (equivalent dose 100 mg). Following that, two sprays of 10% lignocaine (equivalent dose 20 mg) applied to the oropharynx. All the procedures were performed under moderate sedation as per the protocol, for which intravenous medication comprising a combination of short-acting benzodiazepine (midazolam) and an opioid agent (fentanyl) was used. Initially, midazolam 0.015 mg/kg and fentanyl 1.0 mcg/kg were given and dose was escalated targeting a sedation level where subject was sedated and verbal contact was possible at all times. Sedation administration was performed by an experienced bronchoscopy nurse (blinded to the group allocation), who supervised sedation in all subjects. EBUS was performed using the Olympus BF-UC180F Convex Probe Bronchoscope (Olympus Corporation, Japan) through the oral route after insertion of a bite block. During the procedure, 1 ml aliquots of 1% or 2% lignocaine solution were delivered through the bronchoscope using spray-as-you-go technique. The allocated lignocaine solution was prepared by the bronchoscopy nurse and was handed over to the primary bronchoscopy assistant for use who along with the operator was blinded to the concentration used. A total of six aliquots of 1 ml of lignocaine were administered at the baseline in all subjects that included three at the vocal cords, one each in trachea, and both main bronchi. Five ml of air was injected following each aliquot administration so as to push the drug completely out of the working channel of the bronchoscope. Supplemental aliquots of lignocaine were allowed at operator's discretion and were also recorded. Subjects were monitored for any adverse effects. At the completion of the procedure, a bronchoscopist marked the overall procedure satisfaction as well as severity of cough during the procedure on visual analog scale (VAS). The VAS charts for overall procedure satisfaction were anchored by “totally unsatisfactory” (0) to “very satisfactory” (100). The VAS for operator-rated cough was rated on a horizontal line, anchored by “no cough’’ (0) on the one end and “worst cough’’ (100) on the other end. Post-procedure, the subjects were also asked to rate their procedure discomfort on the faces pain scale having six categories ranging between “no pain” and “excruciating pain” demonstrated by various facial expressions.
Endpoints
The primary outcome measures of the study were the operator-rated overall procedure satisfaction on a VAS and operator-rated cough on VAS between the groups. The secondary outcome measures included the total lignocaine dose, number of subjects receiving lignocaine dose >8.2 mg/kg body weight, doses of midazolam and fentanyl between groups, patient-rated faces pain scale scores, and adverse events during procedure.
Statistical analysis
As a pilot study, recruitment of 100 participants was planned. The statistical software package STATA (V9.0 Stata Corp, College Station, TX) was used for statistical analysis, and a P < 0.05 was considered statistically significant. Continuous variables are presented as mean ± standard deviation (SD) or median (interquartile range [IQR]). Two-tailed Pearson's Chi-square test or Fisher's exact test was used to analyze the categorical variables. The differences between non-normally distributed data were compared using nonparametric tests. Student t-test was used to compare the means between groups for normally distributed data, whereas Mann–Whitney U-test was used for comparison between groups in non-normal distribution.
RESULTS
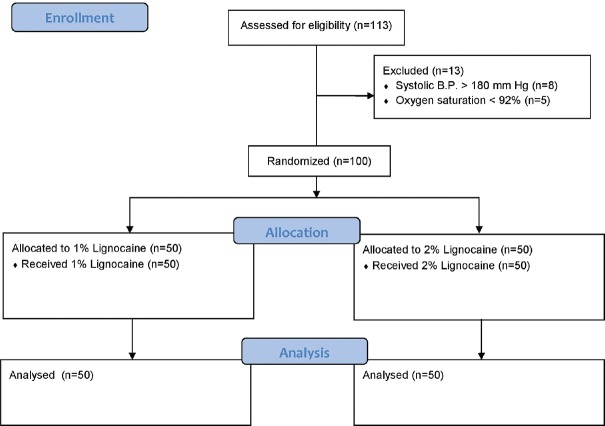
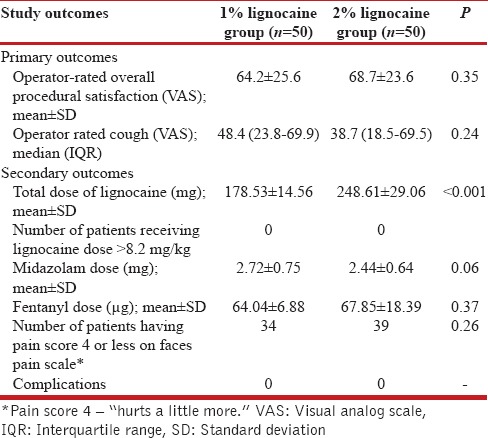
Of the 113 subjects screened for eligibility, 100 subjects were randomized (mean age 45.2 years). Thirteen subjects were excluded before randomization. Fifty subjects each were randomized to 1% and 2% groups, and all randomized subjects completed the study protocol. The flow of participants through the study is depicted in the CONSORT diagram [Figure 1]. The demographic and baseline characteristics were similar between the two groups [Table 1]. The hemodynamic parameters at baseline were comparable between the groups. The summary of study endpoints is summarized in Table 2. The VAS for operator-rated overall procedure satisfaction (mean [SD] [64.2 (25.6) and 68.7 (23.6) in 1% and 2% groups, respectively] [P = 0.35]) and operator-rated cough (median [IQR] [48.4 (23.8–69.9) in 1% group and 38.7 (18.5–69.5) in 2% group] [P = 0.24]) were similar between the two groups. The cumulative dose of lignocaine administered in 2% lignocaine group was significantly greater than in 1% group [248.6 [29] mg vs. 178.5 [14.5] mg; P < 0.01). The doses of midazolam (2.7 [0.7] mg and 2.4 [0.6] mg in 1% and 2% lignocaine groups, respectively [P = 0.058]) and fentanyl (64 [6.8] μg and 67.8 [18.3] μg in 1% and 2% lignocaine groups [P = 0.37], respectively) administered were similar. None of the patient in either group received lignocaine dose >8.2 mg/kg of body weight. There was no significant difference in the faces pain scale scores between the two groups. The overall procedure duration between the groups was similar.
Figure 1.
CONSORT diagram showing the flow of participants through the study
Table 1.
Baseline characteristics of the study participants
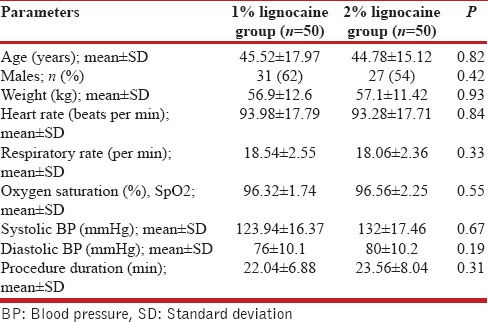
Table 2.
Summary of the primary and secondary outcome measures
DISCUSSION
This is the first study to compare two different lignocaine concentrations for topical anesthesia during EBUS-TBNA. One percent lignocaine was found to be as efficacious as 2% lignocaine, for EBUS-TBNA performed under moderate sedation at a significantly lesser cumulative dose of lignocaine administered. The findings of this study are similar to those in flexible bronchoscopy, thereby demonstrating that airway anesthesia responses during EBUS-TBNA are like those in flexible bronchoscopy and a lower concentration of lignocaine (1%) using spray-as-you-go method is indeed efficacious in this setting also.[3,8,9,10,11]
The sedation and anesthesia practices in EBUS-TBNA, to a large extent, have been extrapolated from flexible bronchoscopy.[12] Canneto et al. have suggested the use of 2% lignocaine solution as mandatory for obtaining ideal conditions during performance of EBUS-TBNA.[7] In studies by Yarmus et al. and Casal et al., 1% lignocaine solution was used, but the mean cumulative lignocaine doses were not available.[13,14] Goyal et al. also used 1% lignocaine for topical anesthesia in conjunction with laryngeal nerve block for advanced diagnostic bronchoscopy procedures including EBUS-TBNA under moderate sedation and reported cumulative lignocaine dose of 4.3 mg/kg.[15] The requirement of sedatives used was however greater than our study. Other authors have reported the use of higher lignocaine concentrations. One study reported use of 4% topical lignocaine during EBUS-TBNA. The mean dose of lignocaine reported was 560 mg which borders the usually prescribed upper limit.[16] There is also description of shifting from a higher to a lower lignocaine concentration for airway anesthesia during EBUS-TBNA. Dhooria et al., in their retrospective analysis (July 2011 through January 2016) of subjects who underwent EBUS-TBNA in a tertiary care center, reported shifting to 1% lignocaine for the procedure after January 2015 while 2% was being used before that.[17] This indicates the need for standardizing the sedation and topical anesthesia approaches during EBUS-TBNA and using a lower concentration of lignocaine during the procedure.
The primary issue concerning topical lignocaine administration is potential toxicity (seizures, arrhythmias, or methemoglobinemia) related to excessive absorption through the airway mucosa. There is a potential for higher serum lignocaine levels in both the elderly and subjects with underlying liver disease. As there is no absolute method to determine which patients will have greater lignocaine absorption and therefore be at greater risk for life-threatening toxicity, published guidelines favor the smallest lignocaine dose possible.
Limited studies are available that have evaluated other topical anesthesia methods specifically in the setting of EBUS-TBNA. Lee et al. compared two different techniques for topically anesthetizing the airway with lignocaine during Convex probe-EBUS-TBNA procedure.[18] They compared standard injection of 2% lignocaine solution through the working channel of the bronchoscope in one group and using a dedicated spray catheter in the other group. The primary endpoint was number of significant cough episodes during the first 30 minutes of the procedure, and delivery through the spray catheter was superior in reducing the procedural cough, P < 0.01. The total dose of lignocaine was 236 (±34) mg and 256 (±66) mg in the spray catheter and injection group, respectively, which is comparable to the dose used in the 2% group, 248.61 (±29.06) mg in our study.
The small sample size is a limitation of our study. Some operators may consider 1 mL lignocaine aliquot volume as low for spray-as-you-go administration. We targeted a sedation level at which verbal contact was possible with the subjects always, but lack of use of a sedation scale is another possible limitation of this pilot study. However, as the sedation administrator was blinded to the lignocaine concentration allocation, it is unlikely to be of major concern in a randomized setting. We did not perform serum lignocaine level estimation due to nonavailability of the same at our center. Although, at the time of this study, we were routinely using nebulized lignocaine administration before EBUS-TBNA, the evidence to support nebulized lignocaine administration during bronchoscopy is weak.[4] All the EBUS-TBNA procedures in our study were performed through the oral route; therefore, the results may not be applicable to nasal route for performing the procedure. Nasal route has also been found safe and feasible to perform EBUS-TBNA though the requirement of lignocaine is likely to be higher in this case as nasal lignocaine gel application is additionally required. Some studies have highlighted that the use of oral route during bronchoscopy may be preferable.[19,20] This is unlikely to be an important limitation as most centers use oral route as the usual approach for performing EBUS-TBNA as in our study.
CONCLUSION
In this pilot study comparing the effectiveness of 1% versus 2% lignocaine solution for airway anesthesia during EBUS-TBNA, there was no significant difference in operator-rated overall procedure satisfaction or cough in between the two groups. We recommend that 1% lignocaine be used for spray-as-you-go administration during EBUS-TBNA. More studies are needed to clarify the ideal sedation and topical anesthesia approaches during EBUS-TBNA.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Madan K, Mohan A, Ayub II, Jain D, Hadda V, Khilnani GC, et al. Initial experience with endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) from a tuberculosis endemic population. J Bronchology Interv Pulmonol. 2014;21:208–14. doi: 10.1097/LBR.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 2.Wahidi MM, Herth F, Yasufuku K, Shepherd RW, Yarmus L, Chawla M, et al. Technical aspects of endobronchial ultrasound-guided transbronchial needle aspiration: CHEST guideline and expert panel report. Chest. 2016;149:816–35. doi: 10.1378/chest.15-1216. [DOI] [PubMed] [Google Scholar]
- 3.Kaur H, Dhooria S, Aggarwal AN, Gupta D, Behera D, Agarwal R. A randomized trial of 1% vs.2% lignocaine by the spray-as-you-go technique for topical anesthesia during flexible bronchoscopy. Chest. 2015;148:739–45. doi: 10.1378/chest.15-0022. [DOI] [PubMed] [Google Scholar]
- 4.Madan K, Biswal SK, Mittal S, Hadda V, Mohan A, Khilnani GC, et al. 1% versus 2% lignocaine for airway anesthesia in flexible bronchoscopy without lignocaine nebulization (LIFE): A randomized controlled trial. J Bronchology Interv Pulmonol. 2018;25:103–10. doi: 10.1097/LBR.0000000000000458. [DOI] [PubMed] [Google Scholar]
- 5.Li YP, Yang J, Duan RW, Jiang GN, Fan J, Zhao RM. Application of modified laryngeal mask airway in endobronchial ultrasound-guided transbronchial needle aspiration. Acta Medi Mediterr. 2013;29:625–32. [Google Scholar]
- 6.Du Rand IA, Blaikley J, Booton R, Chaudhuri N, Gupta V, Khalid S, et al. British Thoracic Society guideline for diagnostic flexible bronchoscopy in adults: Accredited by NICE. Thorax. 2013;68(Suppl 1):i1–44. doi: 10.1136/thoraxjnl-2013-203618. [DOI] [PubMed] [Google Scholar]
- 7.Canneto B, Ferraroli G, Falezza G, Infante MV. Ideal conditions to perform EBUS-TBNA. J Thorac Dis. 2017;9:S414–7. doi: 10.21037/jtd.2017.04.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bansal A, Maqbool S, Jha R. A study on clinical efficacy of 1% versus 2% lignocaine in cough suppression and patient satisfaction during fiber-optic bronchoscopy. CHEST J. 2011;140:869A. [Google Scholar]
- 9.Hasmoni MH, Rani MF, Harun R, Manap RA, Tajudin NA, Anshar FM. Randomized-controlled trial to study the equivalence of 1% versus 2% lignocaine in cough suppression and satisfaction during bronchoscopy. J Bronchol Interv Pulmonol. 2008;15:78–82. [Google Scholar]
- 10.Madan K, Mohan A, Agarwal R, Hadda V, Khilnani GC, Guleria R. A survey of flexible bronchoscopy practices in India: The Indian Bronchoscopy Survey (2017) Lung India. 2018;35:98–107. doi: 10.4103/lungindia.lungindia_417_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mainland PA, Kong AS, Chung DC, Chan CH, Lai CK. Absorption of lidocaine during aspiration anesthesia of the airway. J Clin Anesth. 2001;13:440–6. doi: 10.1016/s0952-8180(01)00298-7. [DOI] [PubMed] [Google Scholar]
- 12.Vaidya PJ, Chhajed PN. Bronchoscopist-guided sedation in EBUS-TBNA: Can the pitcher also be a hitter? J Bronchology Interv Pulmonol. 2017;24:4–6. doi: 10.1097/LBR.0000000000000351. [DOI] [PubMed] [Google Scholar]
- 13.Casal RF, Lazarus DR, Kuhl K, Nogueras-González G, Perusich S, Green LK, et al. Randomized trial of endobronchial ultrasound-guided transbronchial needle aspiration under general anesthesia versus moderate sedation. Am J Respir Crit Care Med. 2015;191:796–803. doi: 10.1164/rccm.201409-1615OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yarmus LB, Akulian JA, Gilbert C, Mathai SC, Sathiyamoorthy S, Sahetya S, et al. Comparison of moderate versus deep sedation for endobronchial ultrasound transbronchial needle aspiration. Ann Am Thorac Soc. 2013;10:121–6. doi: 10.1513/AnnalsATS.201209-074OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goyal G, Pisani MA, Murphy TE, Araujo KL, Puchalski JT. Advanced diagnostic bronchoscopy using conscious sedation and the laryngeal nerve block: Tolerability, thoroughness, and diagnostic yield. Lung. 2014;192:905–13. doi: 10.1007/s00408-014-9607-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeyabalan A, Medford AR. Endobronchial ultrasound-guided transbronchial needle aspiration: Patient satisfaction under light conscious sedation. Respiration. 2014;88:244–50. doi: 10.1159/000363063. [DOI] [PubMed] [Google Scholar]
- 17.Dhooria S, Sehgal IS, Gupta N, Aggarwal AN, Behera D, Agarwal R. Diagnostic yield and complications of EBUS-TBNA performed under bronchoscopist-directed conscious sedation: Single center experience of 1004 subjects. J Bronchology Interv Pulmonol. 2017;24:7–14. doi: 10.1097/LBR.0000000000000332. [DOI] [PubMed] [Google Scholar]
- 18.Lee HJ, Haas AR, Sterman DH, Solly R, Vachani A, Gillespie CT. Pilot randomized study comparing two techniques of airway anaesthesia during curvilinear probe endobronchial ultrasound bronchoscopy (CP-EBUS) Respirology. 2011;16:102–6. doi: 10.1111/j.1440-1843.2010.01861.x. [DOI] [PubMed] [Google Scholar]
- 19.Choi CM, Yoon HI, Lee SM, Yoo CG, Kim YW, Han SK, et al. Oral insertion of a flexible bronchoscope is associated with less discomfort than nasal insertion for Korean patients. Int J Tuberc Lung Dis. 2005;9:344–8. [PubMed] [Google Scholar]
- 20.de Boer GM, Türk Y, Meuleman-van Waning VH, Braunstahl GJ. Bronchoscopy: Oral or nasal insertion? J Bronchology Interv Pulmonol. 2017;24:125–30. doi: 10.1097/LBR.0000000000000356. [DOI] [PubMed] [Google Scholar]