Abstract
Setting:
This study was conducted at a pulmonary function laboratory of a tertiary care hospital in North India.
Objective:
The objective was to study the diagnostic characteristics and clinically useful threshold of forced expiratory time (FET, measured by auscultation over trachea) as a screening tool for identifying airway obstruction and to substantiate the diagnostic utility of FET through a systematic review of English literature.
Methods:
FET was compared in seventy patients with airway obstruction (Group A) and seventy controls with normal spirometry (Group B). Within-subject reproducibility of FET, and its correlation with spirometric parameters, was assessed. Diagnostic accuracy of FET in detecting airway obstruction was evaluated at various time thresholds. A systematic review of English literature on FET was also carried out.
Results:
Median FET was significantly longer in Group A (7.04 s [interquartile range (IQR) 6.67–7.70 s] vs. 4.14 s [IQR 3.60–4.68 s], P < 0.001). At a threshold of 5 s, FET had high sensitivity (0.943) and reasonable specificity (0.814) in detecting airway obstruction. FET measurements were reproducible and correlated negatively with forced expiratory volume in first second (FEV1), FEV1/forced vital capacity, and peak expiratory flow. The systematic review yielded 13 publications. At a widely used threshold of 6 s to describe airway obstruction, pooled sensitivity and specificity from five datasets were 0.802 (95% confidence interval [CI] 0.668–0.890) and 0.837 (95% CI 0.570–0.952), respectively.
Conclusion:
FET of 5 s or more, rather than the commonly recommended threshold of 6 s, should be regarded as abnormal.
KEY WORDS: Forced expiratory time, obstructive lung diseases, sensitivity and specificity, spirometry, systematic review
INTRODUCTION
Airway obstruction is currently defined as a disproportionate reduction of forced expiratory volume in the first second (FEV1) in relation to the forced vital capacity (FVC) during a spirometric evaluation.[1] Spirometry is, therefore, considered essential for evaluation of persons suspected to have airflow limitation due to common disorders such as bronchial asthma or chronic obstructive pulmonary disease (COPD). This is especially important as patient history and clinical examination is often subjective, and symptoms and signs often have poor accuracy in identifying or excluding airflow limitation. Although spirometry can objectively document the presence of an obstructive ventilatory defect, it is an expensive investigation, requires technical expertise in test performance and equipment calibration and maintenance, and is not widely available, especially in resource-constrained settings. There is, therefore, a need for simpler, yet objective, parameters which can detect airway obstruction.
Historically, several tests such as whistling, blowing out candles, and blowing out matches have been employed as a surrogate for spirometry to screen for airway obstruction. However, these, and other physical signs of airway obstruction, were inadequately standardized and suffered from a high degree of variability and were therefore poor markers for this condition.[2] Auscultation of tracheal sounds to generate an objective measure – the forced expiratory time (FET) – was proposed more than 50 years ago. The test is simple to perform, requires no additional infrastructure, can be easily added to routine patient examination without consuming much time, and provides results comparable to the time calculated on spirometry.[3,4] It has good reproducibility and correlates well with other measures of airflow limitation.[5,6,7] Several investigators have found variable diagnostic accuracy at different threshold timings and reported correlation with clinical outcomes.[4,8,9,10,11,12,13,14,15] A threshold of 6 s is widely used based on early description of the test characteristics.[4] However, there is no clarity on the exact utility of this threshold in a clinical scenario. We believe that measurement of FET can be a useful screening tool to identify individuals with higher probability of airway obstruction, who merit more detailed evaluation. FET thresholds therefore need to be optimized to fulfill this target, and an ideal threshold should provide a high sensitivity and an acceptable specificity in identifying airway obstruction. We conducted this study to study the diagnostic characteristics and clinically useful threshold of FET, measured by auscultation over trachea, as a screening tool for identifying airway obstruction, and to substantiate the diagnostic utility of FET through a systematic review of English literature.
METHODS
Participants were prospectively enrolled in this cross-sectional study from among patients referred for spirometry to our pulmonary function laboratory. FET estimation may be useful as a screening test and should demonstrate high sensitivity in identifying airway obstruction. Sample size was therefore estimated at an expected sensitivity of 0.94 ± 0.06 and calculated to be at least 120 participants for a 1:1 case–control distribution. We decided to enroll seventy patients with spirometrically proven obstructive disease (Group A) and an equal number with spirometrically proven normal lung function (Group B). Spirometry was carried out by experienced technicians on a dry rolling seal spirometer (Spiro RS232; P.K. Morgan Ltd., UK), and FVC, FEV1, and peak expiratory flow (PEF) were measured as per standard guidelines.[16] Obstruction on spirometry was defined as FEV1/FVC ratio below the lower limit of normal (derived from reference equations for North Indians being used at our institute) for that individual.[17,18] All study participants provided informed consent, and the study protocol was approved by our institute's Ethics Committee (No. INT/IEC/2013/17).
FET was measured by a single investigator (SD) who had no knowledge about the spirometry report. Participants were made to sit comfortably, and a forced expiratory maneuver was demonstrated to them. They were then asked to inhale deeply, followed by a forced exhalation with mouth open, as quickly and as completely as possible. A stethoscope bell was positioned over the upper trachea in the suprasternal notch for auscultation during exhalation. The total duration of audible expiration was timed to the nearest 0.1 s using a stop watch. The test was considered acceptable if the participant did not pause or cough in between. This exercise was considered as a practice maneuver and its result was not considered further. Next, three more maneuvers were similarly repeated, with at least 30 s interval between successive blows. The largest time from among these was recorded as that participant's FET.
Observed FET timings were summarized as medians and corresponding interquartile range (IQR) and compared between patient groups using the nonparametric Mann–Whitney U-test. Diagnostic accuracy of FET in identifying airway obstruction at various thresholds was studied by computing sensitivity, specificity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), and positive and negative predictive value, and summarized using a receiver operating characteristic (ROC) curve. Intrasubject reliability of repeated measurements was explored through coefficient of variance and intraclass correlation coefficient. FET was also correlated with other measured spirometric variables through Spearman's correlation coefficient. Statistical significance was assessed at P < 0.05.
The systematic review was conducted as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.[19] An electronic database search was conducted through PubMed and Embase platforms, using the search terms forced expiratory time, forced expiratory noise, forced expiratory sound, forced expiratory tracheal time, forced expiratory tracheal noise, and forced expiratory tracheal sound. This was supplemented by additional citations obtained from bibliographic review of key publications, as well as articles from our personal records. Titles and abstracts of publications identified through this search were screened for articles meriting detailed evaluation. Publications in foreign languages, animal studies, and articles not primarily related to FET were excluded. Full text of the remaining articles was evaluated in detail independently by two investigators (ANA and RA) to identify publications suitable for data synthesis. Any disagreements were resolved through consensus. We included all original articles describing methodology, diagnostic performance, and/or clinical utility of FET in identifying airway obstruction or describing clinical features or outcomes. Review articles, case reports, editorials, commentaries, letters to editor not describing original data, and conference abstracts were not considered further. Information related to the study population, technique of FET assessment, diagnostic thresholds, and performance of FET (diagnostic accuracy, reliability, correlation with other lung function tests, relationship with clinical features and outcomes, etc.) was extracted from each included study. Summary estimates of diagnostic accuracy were computed for pooled data using a bivariate random effects model and expressed graphically through a forest plot.
RESULTS
Both groups had 37 men and 33 women. Participants in Group A and Group B had similar age (mean, 46.5 ± 13.8 years vs. 45.7 ± 14.0 years, P = 0.738) and height (mean, 158.9 ± 9.1 cm vs. 161.1 ± 8.9 cm, P = 0.134). Significantly more participants in Group A (21 of 70, 30.0%) had smoked tobacco as compared to those in Group B (11 of 70, 15.7%, P = 0.044). In Group A, 61 (87.1%), 50 (71.4%), and 49 (70.0%) patients, respectively, reported having dyspnea, wheeze, and cough. Of these, 34 patients had asthma, 33 had COPD, and the rest had other diagnoses.
FET could be easily recorded for all the included participants. FET measurements within the same session were quite reproducible, with median coefficient of variation of 3.04% (IQR, 1.61%–5.22%) and intraclass correlation coefficient of 0.977. Median FET was 7.04 s (IQR, 6.67–7.70 s) for Group A participants and 4.14 s (IQR, 3.60–4.68 s) for Group B participants. This difference was statistically significant (P < 0.001 on Mann–Whitney U-test). FET was negatively and significantly correlated with FEV1 (% predicted), FVC (% of predicted), FEV1/FVC, and PEF (Spearman's correlation coefficients −0.717, −0.506, −0.761, and −0.539, respectively, P < 0.001 for all) [Figure 1].
Figure 1.

Correlation between forced expiratory time and percentage of predicted forced expiratory time in the first second (FEV1). Clear circles represent participants with normal spirometry and dark circles represent those with airway obstruction
Diagnostic accuracy estimates for various FET thresholds are summarized in Table 1. Area under the ROC curve was 0.933 (95% confidence interval [CI] 0.890–0.976), suggesting FET to be a good discriminator in identifying airway obstruction [Figure 2]. Using the ROC curve, the best tradeoff between sensitivity and specificity was noted around FET of 5 s. At a threshold of ≥5 s, FET had a high sensitivity and a reasonable specificity to retain its utility as a screening test for airway obstruction [Table 1].
Table 1.
Diagnostic performance of forced expiratory time in assessing spirometrically determined airway obstruction
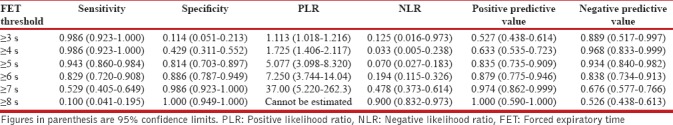
Figure 2.
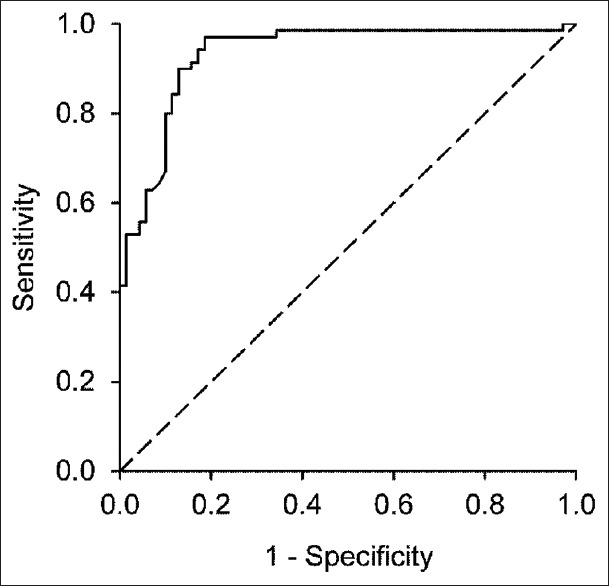
Receiver operating characteristic curve to assess the diagnostic performance of forced expiratory time
Our literature search yielded 392 citations, of which only 13 were finally considered for data synthesis [Figure 3].[3,4,5,6,7,8,9,10,11,12,13,14,15] Auscultation for measuring FET was conducted over posterior chest wall, or over sternum, in one study each.[3,14] All other studies used suprasternal notch for auscultation [Table 2]. Five studies reported some form of training to participants prior to actual testing.[4,7,9,11,12] Both simple wrist watch with seconds hand and a stop watch were used for recording time [Table 2]. Up to five FET maneuvers were performed in each session, and either the longest or the average time was generally reported for data analysis [Table 2]. Five studies provided data on diagnostic accuracy of FET through sensitivity and specificity calculations [Table 3].[4,8,9,11,15] Two of these reported data on multiple diagnostic thresholds and higher thresholds were associated with better sensitivity but with poor specificity.[8,11] At a widely used threshold of 6 s to describe airway obstruction, sensitivity ranged from 0.61 to 0.92 and specificity from 0.43 to 1.00, in four studies [Table 3]. Pooled sensitivity and specificity from these four reports, plus the present study, were 0.802 (95% CI, 0.668–0.890) and 0.837 (95% CI, 0.570–0.952), respectively [Figure 4]. Corresponding pooled PLR and NLR were 4.932 (95% CI, 1.574–15.451) and 0.237 (95% CI, 0.131–0.429), respectively. Four studies summarized diagnostic performance using likelihood ratio or area under ROC curve.[10,11,12,14] Area under ROC curve was 0.61 and 0.72 in two of these studies.[10,11] Five studies reported negative correlations with spirometric volumes and flows, FEV1/FVC, or specific airway conductance [Table 3].[3,4,6,7,15] In one study on preoperative assessment before nonthoracic surgery, 22.4% of patients had obstructive airway disease and higher FET was significantly associated with postoperative complications.[13]
Figure 3.

Selection process to identify studies evaluating forced expiratory time by auscultation
Table 2.
Study characteristics of publications identified for data synthesis
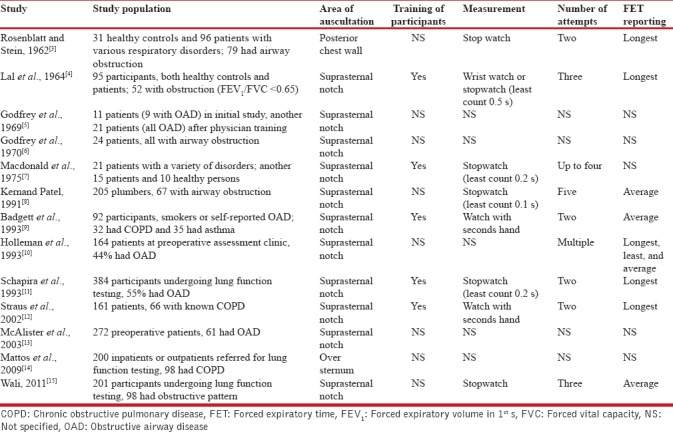
Table 3.
Important observations from studies included in the systematic review
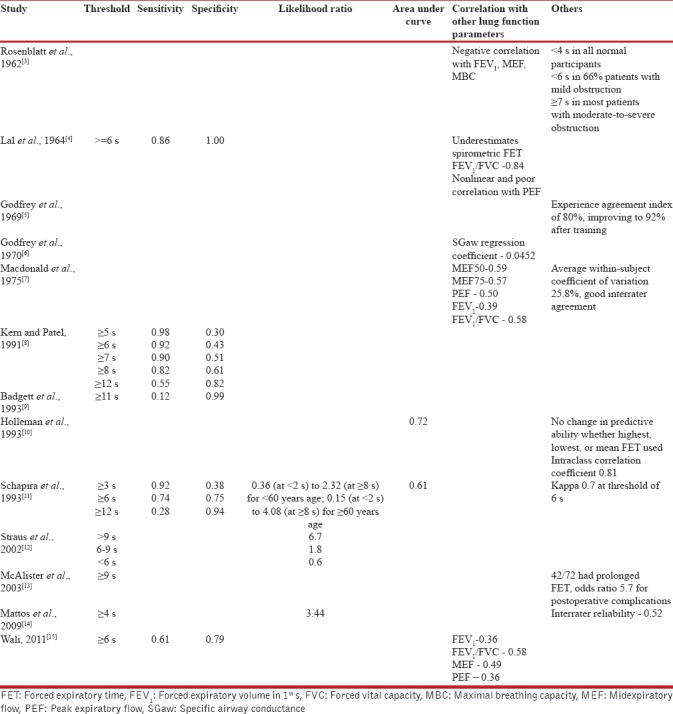
Figure 4.

Forest plot of publications on sensitivity and specificity of forced expiratory time in identifying airway obstruction at a threshold of 6 s. Solid squares represent individual study estimates and horizontal lines represent corresponding 95% confidence limits. Vertical dashed lines represent the pooled estimates from all studies
DISCUSSION
There is no doubt that spirometry is the best modality to diagnose airway obstruction by demonstrating a reduction in FEV1/FVC ratio. However, the investigation is not universally available, and clinicians in resource-limited settings often rely on soft clinical pointers to assess probability of airflow limitation so that only those with higher probability of airway obstruction get referred for pulmonary function testing. Unfortunately, most of these clinical signs are rather subjective and poor at screening for airway obstruction. FET has been proposed as an easy and a more objective marker, but there is no consensus regarding its utility. Very few studies have evaluated FET in clinical practice, as is evident from the results of our systematic review [Tables 2 and 3]. Previous studies have reported on diagnostic accuracy of FET, but not on its performance as a screening test. This study was undertaken to fill some of these knowledge gaps.
We reported the highest FET measurement from among three maneuvers in the same test session. Previous investigators have generally used either the mean or the maximum FET from multiple attempts [Table 2], and there is no consensus on the issue. At least one previous study has suggested that the choice of least, average, or maximum FET does not significantly influence the predictive ability of the test.[10] We tried to establish a threshold for FET that would provide a high sensitivity and a reasonable specificity, features expected from a good screening test. Earlier studies had focused more on optimizing diagnostic accuracy, and a threshold of 6 s is widely used. At this threshold, both sensitivity and specificity are moderately high. Unfortunately, neither is sufficiently high to enable the test to have clinical utility as either a screening (high sensitivity) or a diagnostic (high specificity) tool. We found that a slightly lower FET threshold of 5 s provided high sensitivity (0.943) and an acceptable specificity (0.814), indicating that this cutoff can be used to screen patients for airway obstruction. We also calculated the PLR and NLR at this threshold. Likelihood ratios may be a better way of expressing diagnostic performance, by providing a measure of how much the odds of disease change based on a negative, or a positive, test result. In general, PLRs above 10 or NLRs <0.1 reflect the test's ability to confirm or exclude disease, respectively.[20] Specifically, a NLR of 0.070 at the 5 s threshold in our study suggests that there are only seven false negatives for every 100 true negatives, implying that this threshold can be used to exclude airway obstruction [Table 1]. However, the PLR of 5.077 at this threshold suggests that there are ten false positives for every 51 true positives; hence, this threshold is less useful to confirm airway obstruction. In fact, FET can be a good confirmatory test only at a threshold of 7 s, but a low sensitivity and high NLR at this threshold severely limit its clinical utility [Table 1]. On the other hand, pooled PLR and NLR from five studies (including our study) providing information on the commonly used FET threshold of 6 s were 4.932 and 0.237, respectively. At this threshold, FET is unlikely to be useful in either confirming or excluding airway obstruction.
Our data also support excellent within-subject reproducibility of FET measurements in a single test session. A single previous study had reported mean within-subject coefficient of variation of 25.8% and concluded that such variability precluded the use of FET as a screening test in clinical practice.[7] However, three other studies have shown good test repeatability.[5,10,11] Previous studies have also shown good interrater reliability of the test, although this was not examined in our study.[7,14] We have also shown good negative correlation between FET and spirometrically determined lung volumes and PEF, implying that FET gets prolonged with worsening airway obstruction. This is largely similar to previous studies.[3,7,15]
Our study has certain limitations. We have looked at the diagnostic accuracy of FET as the sole test in diagnosing airway obstruction. However, other clinical parameters can also be indicative of the same, and this information is routinely available to the clinician while figuring a probability of airway obstruction. In one study, self-reported history of COPD and presence of wheezing improved the likelihood of diagnosing COPD.[12] Our study population consisted of patients referred for spirometry at a tertiary care center, and many had severe airflow limitation. Hence, our findings may not be truly reflective of the utility of FET in other settings (for instance, screening for COPD in the general population). Moreover, the general population may also include patients with restrictive ventilatory disorders. We did not include such patients in our study since low lung volumes are associated with early completion of forced expiration, and hence a low FET. Our systematic review identified only articles published in English, and we may have missed some important publications in other languages.
In summary, we have documented diagnostic accuracy and clinical utility of FET in identifying airway obstruction. The frequently used FET threshold of 6 s is a poor discriminator, both for screening and confirming airway obstruction. We propose that FET of 5 s or more should be regarded as abnormal during patient screening, and these patients should undergo spirometry for confirmation of diagnosis. Our suggestions need to be replicated in other studies in more diverse settings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–68. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 2.Holleman DR, Jr, Simel DL. Does the clinical examination predict airflow limitation? JAMA. 1995;273:313–9. [PubMed] [Google Scholar]
- 3.Rosenblatt G, Stein M. Clinical value of the forced expiratory time measured during auscultation. N Engl J Med. 1962;267:432–5. doi: 10.1056/NEJM196208302670903. [DOI] [PubMed] [Google Scholar]
- 4.Lal S, Ferguson AD, Campbell EJ. Forced expiratory time: A simple test for airways obstruction. Br Med J. 1964;1:814–7. doi: 10.1136/bmj.1.5386.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Godfrey S, Edwards RH, Campbell EJ, Armitage P, Oppenheimer EA. Repeatability of physical signs in airways obstruction. Thorax. 1969;24:4–9. doi: 10.1136/thx.24.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Godfrey S, Edwards RH, Campbell EJ, Newton-Howes J. Clinical and physiological associations of some physical signs observed in patients with chronic airways obstruction. Thorax. 1970;25:285–7. doi: 10.1136/thx.25.3.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macdonald JB, Cole TJ, Seaton A. Forced expiratory time – Its reliability as a lung function test. Thorax. 1975;30:554–9. doi: 10.1136/thx.30.5.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kern DG, Patel SR. Auscultated forced expiratory time as a clinical and epidemiologic test of airway obstruction. Chest. 1991;100:636–9. doi: 10.1378/chest.100.3.636. [DOI] [PubMed] [Google Scholar]
- 9.Badgett RG, Tanaka DJ, Hunt DK, Jelley MJ, Feinberg LE, Steiner JF, et al. Can moderate chronic obstructive pulmonary disease be diagnosed by historical and physical findings alone? Am J Med. 1993;94:188–96. doi: 10.1016/0002-9343(93)90182-o. [DOI] [PubMed] [Google Scholar]
- 10.Holleman DR, Jr, Simel DL, Goldberg JS. Diagnosis of obstructive airways disease from the clinical examination. J Gen Intern Med. 1993;8:63–8. doi: 10.1007/BF02599985. [DOI] [PubMed] [Google Scholar]
- 11.Schapira RM, Schapira MM, Funahashi A, McAuliffe TL, Varkey B. The value of the forced expiratory time in the physical diagnosis of obstructive airways disease. JAMA. 1993;270:731–6. [PubMed] [Google Scholar]
- 12.Straus SE, McAlister FA, Sackett DL, Deeks J CARE-COAD2 Group, Clinical Assessment of the Reliability of the Examination-Chronic Obstructive Airways Disease. Accuracy of history, wheezing, and forced expiratory time in the diagnosis of chronic obstructive pulmonary disease. J Gen Intern Med. 2002;17:684–8. doi: 10.1046/j.1525-1497.2002.20102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McAlister FA, Khan NA, Straus SE, Papaioakim M, Fisher BW, Majumdar SR, et al. Accuracy of the preoperative assessment in predicting pulmonary risk after nonthoracic surgery. Am J Respir Crit Care Med. 2003;167:741–4. doi: 10.1164/rccm.200209-985BC. [DOI] [PubMed] [Google Scholar]
- 14.Mattos WL, Signori LG, Borges FK, Bergamin JA, Machado V. Accuracy of clinical examination findings in the diagnosis of COPD. J Bras Pneumol. 2009;35:404–8. doi: 10.1590/s1806-37132009000500003. [DOI] [PubMed] [Google Scholar]
- 15.Wali SO. The diagnostic value of forced expiratory time. Saudi J Int Med. 2011;1:43–6. [Google Scholar]
- 16.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 17.Jindal SK, Wahi PL. Pulmonary function laboratory in the tropics: Needs, problems and solutions. In: Sharma OP, editor. Lung Disease in the Tropics. New York: Marcel Dekker; 1991. pp. 523–42. [Google Scholar]
- 18.Aggarwal AN, Gupta D, Jindal SK. Development of a simple computer program for spirometry interpretation. J Assoc Physicians India. 2002;50:567–70. [PubMed] [Google Scholar]
- 19.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann Intern Med. 2009;151:W65–94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 20.Deeks JJ, Altman DG. Diagnostic tests 4: Likelihood ratios. BMJ. 2004;329:168–9. doi: 10.1136/bmj.329.7458.168. [DOI] [PMC free article] [PubMed] [Google Scholar]


