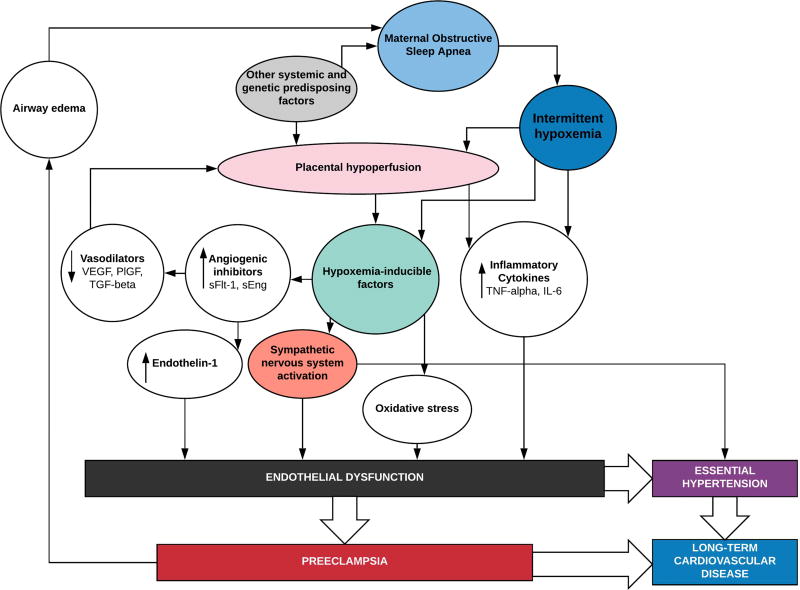
Figure 1.
We propose plausible mechanisms by which intermittent hypoxemia due to maternal obstructive sleep apnea may converge with pathways implicated in the pathogenesis of preeclampsia. The factors that lead to the abnormal placental implantation and vascular development associated with preeclampsia are still under investigation, but several studies suggest that oxygen tension is an important modulating factor early in placental development. Inflammatory cytokines are released both in response to intermittent hypoxemia, and placental hypoperfusion and both may contribute to endothelial dysfunction. Hypoxemia-inducible factors released in response to intermittent hypoxemia and reoxygenation have been implicated as mediators of sympathetic activation, oxidative stress, and angiogenic factors that lead to endothelial dysfunction and subsequent essential hypertension or preeclampsia.
interleukin 6 (IL-6); placental growth factor (PlFG); soluble endoglin (sEng); soluble fms-like tyrosine kinase 1 (sFlt-1); transforming growth factor-beta (TGF-beta); tumor necrosis factor-alpha (TNF-alpha); vascular-derived endothelial growth factor (VEGF)