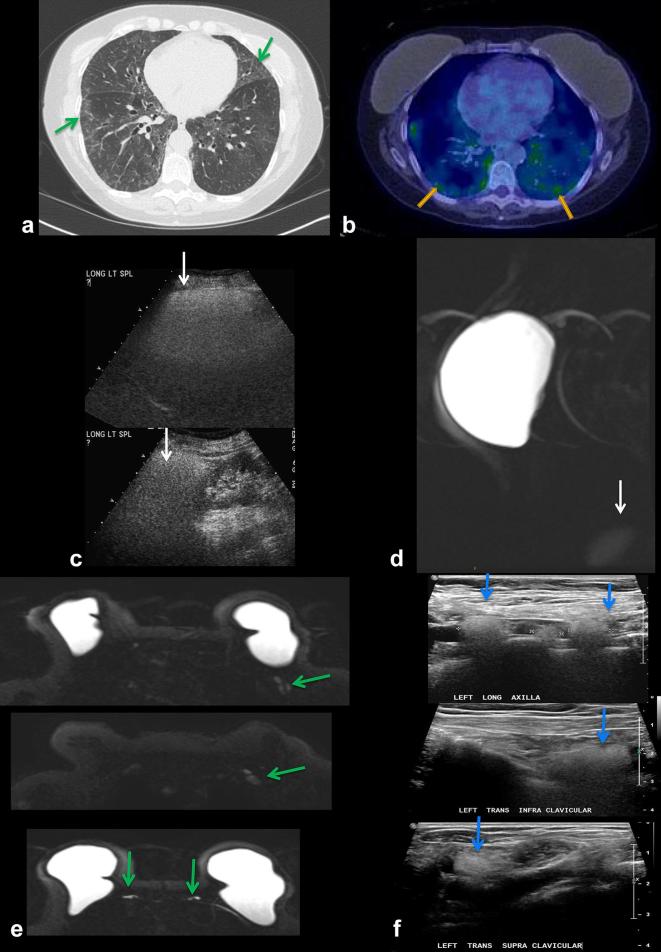
Figure 14.
A 75-year-old patient with chronic pulmonary infiltrates. History of metastatic breast cancer status post-bilateral mastectomies and silicone implant reconstruction 25 years ago, and several implant revisions since. (a) CT chest shows ground-glass opacities in the lungs bilaterally (arrows). Multifocal lymphadenopathy was also noted on CT (not shown) (b) PET/CT shows hypermetabolic FDG-avid pulmonary infiltrates bilaterally (arrows). Patient underwent lung biopsy showing silicone pneumonitis. (c) Interestingly, an ultrasound of the spleen performed 10 years prior to presentation shows hyperechoic shadowing, suggestive of silicone deposition, not appreciated at the time. (d) Recent silicone sensitive MRI demonstrates incidental hyperintense signal in the spleen (arrow), confirming silicone deposition in the spleen. (e) Silicone sensitive MRI sequences showing hyperintense signal in left axillary lymph nodes (top), supraclavicular and infraclavicular lymph nodes (middle) and IM nodes (bottom), compatible with silicone deposition in these nodes (arrows). (f) Ultrasound of left axillary (top), infraclavicular (middle) and supraclavicular (bottom) lymph nodes demonstrating the “snowstorm” appearance of silicone lymphadenopathy . FDG, fludeoxyglucose;IM, internalmammary.