Abstract
Choanal atresia (CA) is a relatively rare condition manifesting with respiratory distress. Endoscopic approaches have superseded transnasal and transpalatal approaches. We present a case of a premature baby of 1.10 kg, who developed respiratory distress and was diagnosed with bilateral CA. A nasal airway was created endoscopically using a skeeter drill.
Keywords: Choanal atresia, Paediatric, Otorhinolaryngology, Endoscopic, Skeeter, Drill
Introduction
Congenital choanal atresia (CA) refers to the anatomical closure of the posterior conchae. It is a relatively rare condition that affects 1 in 5000-7000 live births [1]. Unilateral atresia occurs more commonly than bilateral atresia, with a ratio of 2:1 [2]. Incidence also appears to be more common in females than males. Congenital CA can be bony or non-bony; for the purposes of this article we will discuss bony CA as it was the case in our patient.
Patients affected by choanal atresia have a multitude of presentations, ranging from acute airway obstruction to chronic recurrent sinusitis. The severity of clinical presentation will depend on several factors including whether it is unilateral or bilateral, if any other associated airway abnormalities are present or not, such as tracheomalacia, laryngomalacia and subglottic stenosis [3]. Bilateral CA has also been found to be associated with craniofacial abnormalities, including CHARGE syndrome (coloboma of the eye, heart defects, atresia of choanae, retardation of growth, genital/urinary abnormalities and ear abnormalities/deafness), Treacher Collins and Crouzon syndromes [3]. As babies are obligate nasal breathers, this causes those born with CA to be in severe respiratory distress requiring the rapid establishment of a secure airway.
Case Report
A new born premature female baby of 1.10 kg, born at 33 weeks of gestation developed respiratory distress immediately after birth. Post-partum, she was intubated orally to allow for ventilation. She was subsequently transferred from Nice Children's Hospital to Care Hospital, Banjara Hills in Hyderabad, India whilst being on ventilator support for life saving endoscopic nasal surgery.
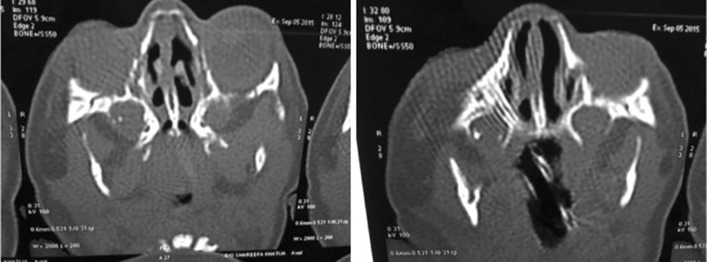
A suction catheter tube was passed into the nose to check for nasal patency. This revealed obstruction bilaterally, confirming the diagnosis of bilateral congenital CA which is inconsistent with life unless an oral airway is kept in the mouth immediately after birth or the baby is intubated and ventilated. The diagnosis was confirmed by CT scanning of the nose and paranasal sinuses (see Fig. 1).
Fig. 1.
CT scans showing bilateral choanal atresia
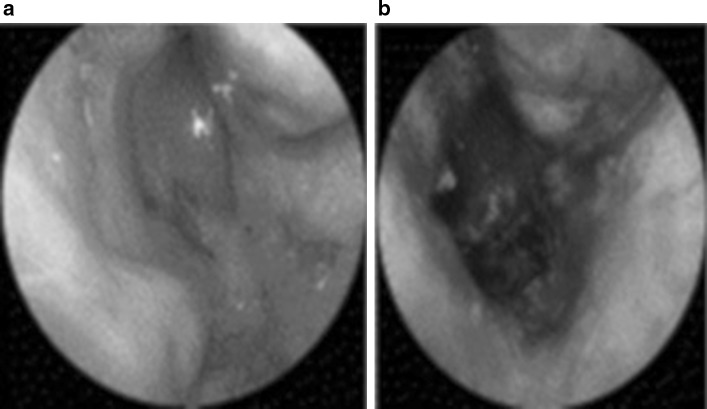
The baby was taken for emergency endoscopic surgery for repair and stenting under general anaesthesia. Firstly mucosal flaps were raised. Then equipment including small diameter 2.7 mm zero and 30° endoscopes (Karl Storz, Germany) and a Skeeter drill with 1 mm diamond burr (Medtronic, USA) were used to reconstruct the nasal passages and to relieve nasal obstruction (Fig. 2). She was weaned off ventilator support on the second post-operative day and nasal breathing was established with nasal stents in place. The stents were kept in the nose for approximately 6 weeks to maintain the patency of the nasal airway and were then removed (Fig. 3). There has been no need for re-surgery since. The baby has been followed up in an outpatient setting on a three-monthly basis with nasal endoscopy for almost a year.
Fig. 2.
The choana area pre (left) and post (right) operative management
Fig. 3.
The patient before (left) and after surgery with stents in place (right)
Discussion
A clinical presentation of severe respiratory distress and cyclical cyanosis are classical signs of neonatal bilateral CA. Airway compromise should be anticipated and managed adequately by establishing a patent airway orally. Intubation may be required if simple airway adjuncts fail to maintain an adequate airway [4].
Definitive management of CA requires surgical intervention. A variety of approaches are used and currently, there is no gold standard approach [5]. Traditionally the transnasal puncture approach was used, and this is especially useful in very small infants where insertion of an endoscope may prove difficult. Surgeons have used antral washout trocar and cannulas, blindly with the assistance of headlights or nasal gouges. This was a crude approach and had the potential to cause peripheral trauma, nasal synechiae and adhesions. Transpalatal repair has also been described. It appears that nowadays, most surgeons have adopted the transnasal endoscopic approach [6]. This approach has reported success rates ranging from 67 to 88% [7].
Now with the advantage of 2.7 mm zero and 30° nasal endoscopes along with HD cameras and HD monitors we can have an excellent view of the atretic segment. Using the 1 mm diamond burr Skeeter drill, we were able to drill the bony atretic segment in a controlled fashion with better visualization as the 1 mm diamond drill and nasal endoscope could be engaged in the same nostril at the same time. The use of the smaller diameter shaft of the Skeeter drill especially in a premature baby with narrower nostrils meant that we could reduce the risk of damage to surrounding structures and resultant complications. This is an advantage over other drills such as mastoid drills as it avoids damage to the columella and nostril through drive shaft contact. As far as we know, the use of a skeeter drill to obtain patency in the atretic segment in cases of congenital CA has not been reported in world literature previously. We believe this was an innovative approach, which evolved on the operating table while we struggled in the narrow nostrils of this patient.
Postoperatively, one of the most common complications includes re-stenosis. Stents have been utilised as a way of preventing re-stenosis as well as to provide a nasal airway for patients with bilateral stenosis. However, literature has shown variability in the benefits of stenting. Some studies have shown that repair of CA can be done safely without the use of stents. Carter et al. [8] found that use of stents was associated with higher rates of granulation tissue formation along with an increased need for further procedures for dilatation. Other studies have recommended the use of stents especially in very young adults and in cases of bilateral atresia, to prevent early re-stenosis [9, 10]. Despite differing views with regards to the use of stents, in the senior author’s experience, the use of stents has not impeded the healing process. They have assisted in maintaining the patency of the nasal airway and facilitated healing at the operated site in the choanal orifices. On balance the use of stents is thought to reduce the risk of re-stenosis in the management of congenital choanal atresia.
In conclusion, we propose the use of a 1 mm diamond skeeter drill in the repair of bilateral choanal atresia. The skeeter drill allows for controlled and precise movements, which help to minimise peripheral damage to surrounding structures and its resulting complications. The variability in efficacy of the use of stents in preventing re-stenosis calls for further study.
References
- 1.Ramsden J, Campisi P, Forte V. Choanal atresia and choanal stenosis. Otolaryngol Clin North Am. 2009;42(2):339–352. doi: 10.1016/j.otc.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 2.Hengerer A, Brickman T, Jeyakumar A. Choanal atresia: embryologic analysis and evolution of treatment, a 30-year experience. Laryngoscope. 2008;118(5):862–866. doi: 10.1097/MLG.0b013e3181639b91. [DOI] [PubMed] [Google Scholar]
- 3.Burrow TA, Saal HM, de Alarcon A, Martin LJ, Cotton RT, Hopkin RJ. Characterization of congenital anomalies in individuals with choanal atresia. Arch Otolaryngol Head Neck Surg. 2009;135(6):543–547. doi: 10.1001/archoto.2009.53. [DOI] [PubMed] [Google Scholar]
- 4.Burrow T, Saal H, de Alarcon A, Martin L, Cotton R, Hopkin R. Characterization of congenital anomalies in individuals with choanal atresia. Arch Otolaryngol-Head Neck Surg. 2009;135(6):543. doi: 10.1001/archoto.2009.53. [DOI] [PubMed] [Google Scholar]
- 5.Kwong K. Current updates on choanal atresia. Front Pediatr. 2015;3:52. doi: 10.3389/fped.2015.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park A, Brockenbrough J, Stankiewicz J. Endoscopic versus tradiational approaches to choanal atresia. Otolaryngol Clin North Am. 2000;33(1):77–90. doi: 10.1016/S0030-6665(05)70208-5. [DOI] [PubMed] [Google Scholar]
- 7.Freitas R, Berkowitz R. Bilateral choanal atresia repair in neonates—a single surgeon experience. Int J Pediatr Otorhinolaryngol. 2012;76(6):873–878. doi: 10.1016/j.ijporl.2012.02.063. [DOI] [PubMed] [Google Scholar]
- 8.Carter J, Lawlor C, Guarisco J. The efficacy of mitomycin and stenting in choanal atresia repair: a 20 year experience. Int J Pediatr Otorhinolaryngol. 2014;78(2):307–311. doi: 10.1016/j.ijporl.2013.11.031. [DOI] [PubMed] [Google Scholar]
- 9.Riepl R, Scheithauer M, Hoffmann T, Rotter N. Transnasal endoscopic treatment of bilateral choanal atresia in newborns using balloon dilatation: own results and review of literature. Int J Pediatr Otorhinolaryngol. 2014;78(3):459–464. doi: 10.1016/j.ijporl.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 10.Elsherif A, Osman Y, Abdelmoghny A, Mahrous A. Endonasal repair of choanal atresia, does stenting have a better outcome? Egypt J Ear Nose Throat Allied Sci. 2012;13(1):13–17. doi: 10.1016/j.ejenta.2012.02.004. [DOI] [Google Scholar]