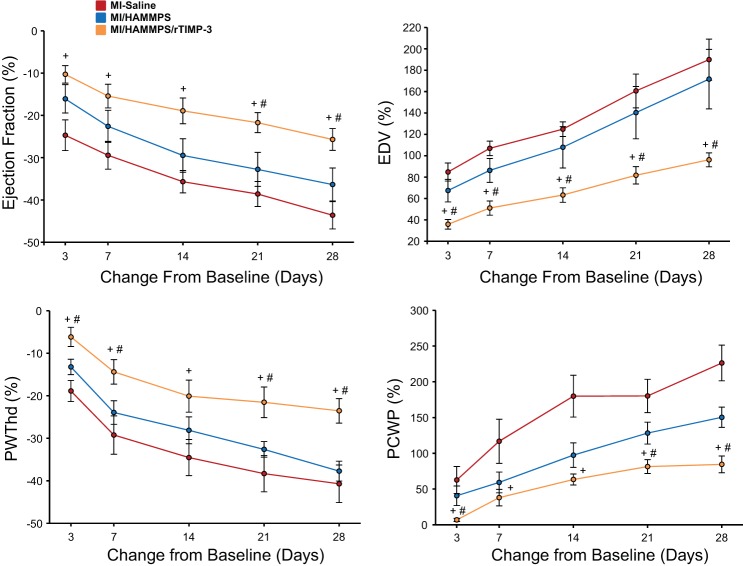
Fig. 1.
To examine more carefully time-dependent changes in key response variables of left ventricular (LV) function and geometry, percent changes from baseline [before myocardial infarction (MI) induction] were computed. The absolute values for these variables are shown in Table 1. LV ejection fraction fell in a time-dependent manner post-MI in all groups, but the relative magnitude of this functional decline was blunted in the MI/matrix metalloproteainase (MMP)-sensitive hyaluronic acid (HA) gel (HAMMPS)/recombinant tissue inhibitor of metalloproteinase (rTIMP)-3 group. LV end-diastolic volume (EDV), a measure of LV dilation, increased significantly in all groups. For example, in the MI/saline group, LV end-diastolic volume increased by over 150% from baseline. However, at all post-MI time points, the degree of LV dilation was reduced in the MI/HAMMPS/rTIMP-3 group. LV end-diastolic posterior wall thickness (PWThd) fell significantly from baseline values, but the degree of LV thinning within this targeted MI region was reduced in the MI/HAMMPS/rTIMP-3 group. Pulmonary capillary wedge pressure (PCWP), an index of LV filling pressures, increased in a time-dependent manner post-MI, but in relation to MI/saline and MI/HAMMPS values was reduced in the MI/HAMMPS/rTIMP-3 group. In all of the data points shown, the change in values was significantly different from baseline (P < 0.05) and thus for clarity have not been marked. Sample sizes for each of the MI groups are shown in Table 1. +P < 0.05 vs. MI/saline; #P < 0.05 vs. MI/HAMMPS.