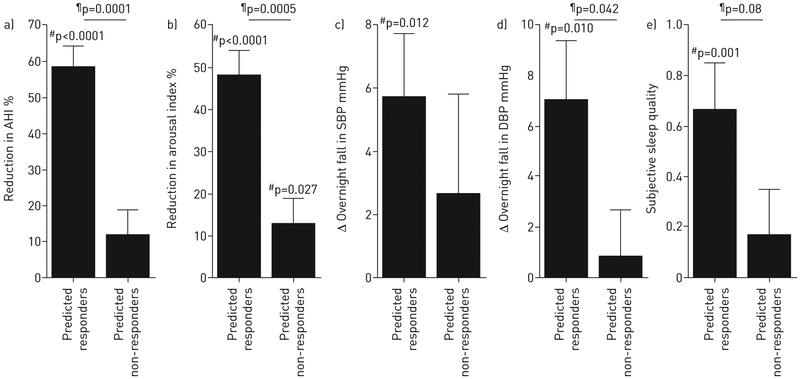
FIGURE 5.
Effect of supplemental oxygen on primary and secondary outcomes in patients with suitable pathophysiology, i.e. “predicted responders” (n=13), and patients with unsuitable pathophysiology, i.e. “predicted non-responders” (n=23), based on endophenotypic traits (logistic regression, cross-validated; table 2, figure 4). a) In predicted responders, treatment led to an improvement in obstructive sleep apnoea severity (reduction in apnoea–hypopnoea index (AHI)); in contrast to figure 1, differences between predicted responders and non-responders are not “by definition” because subgroups were assigned using only data from the other subjects (i.e. cross-validation). Predicted responders also exhibited improvements in b) the frequency of arousals from sleep, c, d) blood pressure (evening minus morning levels) and e) subjective sleep quality. Subjective sleep quality was scored as follows: 1=slept better; 0=slept the same; −1=slept worse. There was no effect on the Stanford Sleepiness Scale (subjective morning alertness, not shown) in either subgroup. SBP: systolic blood pressure; DBP: diastolic blood pressure. #: oxygen versus sham; ¶: responders versus non-responders. Compare results with figure 1.