Abstract
Amebiasis is still a major healthcare concern, especially in developing countries like Ecuador. The lack of sanitary control and hygiene measures make parasites infections still a burden for patients and physicians. Despite infections due to this parasites are usually mild, severe infections and fatal outcomes although rare still occur. Bowel perforation is a rare complication of amebiasis, and unfortunately, it continues to be almost fatal. We present a case of an Ecuadorian patient who presented to the emergency room with an acute abdomen, despite adequate surgery and critical care, the patient regrettably died. Bowel perforation due to Entamoeba histolytica was the final diagnosis.
INTRODUCTION
Amebiasis is the second leading cause of death from parasitic disease worldwide [1] and due to its great behavioral spectrum, this disease may appear as slight diarrhea up to fulminating events of the colon and liver. Transmission occurs predominantly by a lack of sanitary-hygienic conditions [1, 2]. Bowel perforation is a rare complication of colonic amebiasis and is associated with a high mortality despite specific treatment [1, 3]. Prompt surgical intervention seems to be the best treatment for this unusual complication [1, 4]. We present a case of a 70-year-old female who presented to the emergency room with acute abdominal pain and tenderness. After a prompt evaluation, a colonic perforation was encountered. Despite successful surgery, the patient regretfully died. Bowel perforation due to Entamoeba histolytica was the final diagnosis.
CASE REPORT
Patient is a 70-year-old female, with past medical history of hypertension, hypothyroidism, rheumatoid arthritis and hysterectomy. She presented to the emergency room with asthenia and severe lower abdominal pain. Having experienced a week of dizziness, stomach cramping, frequent watery diarrheas and a general feeling of unwellness.
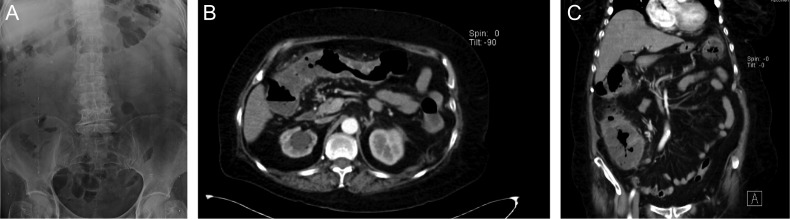
On clinical examination a tachycardic, febrile and dehydrated patient with diffuse abdominal tenderness and guarding was encountered. After proper reanimation, laboratory exams were requested. Complete blood count and abdominal x-ray appeared normal (Fig. 1A), yet stool examination revealed multiples cysts and trophozoites of E. histolytica. Since pain persisted and became more intense, a contrast-enhanced abdominal computed tomography revealed the presence of diffuse colonic mural thickening and enhancement (Fig. 1B) along with pericolonic stranding. No free air under the diaphragm was found (Fig. 1C).
Figure 1:
(A) Abdominal x-ray, without signs of pneumoperitoneum. (B) Abdominal CT, with diffuse colonic mural thickening and enhancement. (C) Abdominal CT with pericolonic stranding.
Due to pain and clinical condition, intravenous antibiotics were initiated and surgery was decided.
At exploratory laparoscopy, the greater omentum was firmly attached to caecum and multiple large areas of necrosis in the ascending and transverse colon were encountered along with inflammatory fluid in the pelvic space. To ensure complete resection and better exposure a conversion to an exploratory laparotomy was performed. Almost the full length of the colon was covered by necrotic patches and multiples colonic perforations were discovered within those patches from which purulent and fecaloid fluid drained into the abdominal cavity (Fig. 2). With this findings, a total colectomy with a proximal ileostomy was performed without any complications.
Figure 2:

Total colectomy, with multiple areas of necrosis.
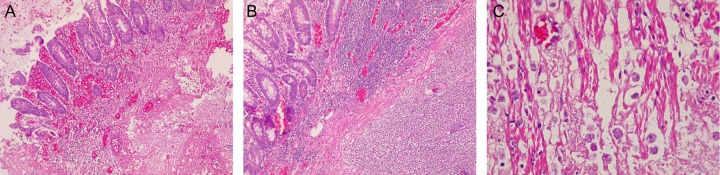
Histopathological examination of the resected bowel revealed, multiples ulcers in the colonic wall along with necrosis and perforation in most of them. The ulcers were covered with an inflammatory exudate and necrotic material (Fig. 3A). Trophozoites of E. histolytica were found within the ulcers and many of them invaded the colonic wall causing a severe inflammatory reaction (Fig. 3B and C).
Figure 3:
(A) Colonic ulcer, with inflammatory reaction, and hemorrhage. (B) Severe inflammatory reaction on the bowel wall. (C) Trophozoites of Entamoeba histolytica invading the colonic wall.
Colonic perforation with necrotizing amoebic colitis was the final diagnosis.
The patient had a grim postoperative course in the Intensive Care Unit. She needed inotropic support, vasoactive agents and ventilator support. However, despite all these efforts, the patient persisted in a hypotensive status that caused a refractory shock and ultimately provoked a severe organ dysfunction and death on the 15th postoperative day.
DISCUSSION
Entamoeba is a protozoan parasite and is the second most common parasitic cause of death in the world [1] and it affects ~10% of the general population [1–3]. Infections are more common in developing countries, mostly due to poor sanitary conditions [4]. Entamoeba exists as two genetically distant species Entamoeba dispar, a non-pathogen species, and E. histolytica a true pathogen [4, 5]. Entamoeba histolytica comprise two forms; an invasive motile stage (trophozoites) and an infective non-motile cyst resistant to gastric secretions [5, 6]. Infection usually begins with the ingestion of cysts from contaminated food or water. But it can occur due to poor oral and anal hygiene, oral sex and promiscuity [5]. Our patient had limited access to clean water, as her house did not have any kind of sewerage, which probably contributed to her infection.
Once ingested, the cyst hatch in the small bowel and releases the trophozoites into the colon [6]. These organisms can live in the colon and feed on mucosal cells and colonic bacteria [1]. In some cases, the parasite invades the bowel wall and create an inflammatory reaction that can be mild, or at times be indistinguishable from an ulcerative colitis with necrosis of the submucosa and muscularis of the colon [7]. These changes are believed to occur from the invasion of the segmental arteries with consequent thrombotic occlusion and necrosis [5, 7]. When a perforation happens, it usually appears in the cecum and ascending colon, yet, any part of the colon can be affected. Fortunately, when the perforation is small the omentum usually seals them, nonetheless, free perforation can still occur [1, 2]. Occasionally, the trophozoites enter the portal circulation and might travel to the liver and brain creating abscess or can travel to the perineum, skin, and genitalia forming ulcers [5]. Due to this great variability, E. histolytica have a broad behavioral spectrum from asymptomatic carriers patients to severely ill patients with fulminant colitis with peritonitis, tachycardia, hypotension, perforation and death [1, 2]. When symptoms do occur, infected patients usually develop fever, weight loss, diarrhea, dehydration and anorexia [8]. These symptoms can persist for months to years with asymptomatic intervals before the patients seek any medical attention [1, 4]. Diagnosis is based usually on the presence of a cyst or trophozoites in the stool [1, 9], however, plain radiographs, endoscopy, ultrasound and CT can be helpful especially when complications arise [6, 7]. Intestinal perforation due to E. histolytica is rare and happens in only 1.9–9.1% of the cases [4]. Perforation usually happens in children, as adults develop other complications as colitis, hemorrhage and even granuloma [4, 5]. Pregnancy, immunodeficiency, steroid use, diabetes and alcohol abuse are risk factors for perforation [5, 10]. The management of amebic perforation of bowel is a challenging issue because when detected the prognosis becomes grim with a mortality as high as 75% [4]. Early surgical treatment is the treatment of choice for perforations [6]. When faced with extensive involvement, multiple perforations and gross contamination, total or subtotal colectomy with ileostomy and mucous fistula or Hartmann procedure must be performed [5]. In our patient, due to her condition, surgery was performed, and a total colectomy was achieved, even if at first surgery apparently controlled the infection, we must not forget that perforation was due to E. histolytica. Despite successful surgery, the patient, unfortunately, died.
Profound knowledge of amebic pathology along with an adequate use of antibiotics, complementary tests and surgical procedures are of vital importance for all surgeons. A high index of suspicion is crucial when faced with amebiasis, as it must be considered in the differential diagnosis for all patients presenting with colonic manifestations. Also, basic sanitary control and good hygiene habits will diminish mortality rates and complications.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1. Athié-Gutiérrez C, Rodea-Rosas H, Guízar-Bermúdez C, Alcántara A, Montalvo-Javé EE. Evolution of surgical treatment of amebiasis-associated colon perforation. J Gastrointest Surg 2010;14:82–7. 10.1007/s11605-009-1036-y. [DOI] [PubMed] [Google Scholar]
- 2. Alavi K. Amebiasis. Clin Colon Rectal Surg 2007;20:033–7. 10.1055/s-2007-970198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cox FE. History of human parasitic diseases. Infect Dis Clin North Am 2004;18:171–88. 10.1016/j.idc.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 4. Prakash A, Sharma LK, Pandit PN. Amoebic perforation of the colon. Br J Surg 1974;61:162–4. 10.1002/bjs.1800610224. [DOI] [PubMed] [Google Scholar]
- 5. Espinosa-Cantellano M, Martinez-Palomo A. Pathogenesis of intestinal amebiasis: from molecules to disease. Clin Microbiol Rev 2000;13:318–31. 10.1128/cmr.13.2.318-331.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hugelshofer S, Petermann D, Oraschc C, Liaudet. L. Toxic megacolon due to fulminant amebic colitis in a non endemic area. J Med Case 2013; 10.4021/jmc900w. [DOI] [Google Scholar]
- 7. Eggleston FC, Verghese M, Handa AK. Amoebic perforation of the bowel: diagnosis and management. Trop Doct 1980;10:160–8. 10.1177/004947558001000409. [DOI] [PubMed] [Google Scholar]
- 8. Ozdogan M, Baykal A, Aran O. Amebic perforation of the colon: rare and frequently fatal complication. World J Surg 2004;28:926–9. 10.1007/s00268-004-7503-4. [DOI] [PubMed] [Google Scholar]
- 9. Chen W. Colon perforation in amebiasis. Arch Surg 1971;103:676. 10.1001/archsurg.1971.01350. [DOI] [PubMed] [Google Scholar]
- 10. Ortiz-Castillo F, Salinas-Aragón LE, Sánchez-Aguilar M, Tapia-Pérez JH, Sánchez-Reyna M, Pierdant-Pérez M, et al. . Amoebic toxic colitis: analysis of factors related to mortality. Pathog Glob Health 2012;106:245–8. 10.1179/2047773212y.00000000. [DOI] [PMC free article] [PubMed] [Google Scholar]