Abstract
Introduction
Nurse-led triage, using the South African Triage Scale, was introduced to the emergency centre of the tertiary referral hospital in Freetown, Sierra Leone in early 2014 prior to the Ebola epidemic. The aim of this study was to measure the effectiveness of the process now that the country has been declared free of Ebola.
Methods
The study was conducted over a five-day consecutive period in the adult emergency centre of the main government teaching hospital in December 2015. The times from arrival to triage and medical assessment were recorded and compared for each triage category. We also assessed the inter-rater reliability of the process.
Results
111 patients were included during the study period. In terms of acuity, 6% were categorised as red, 27% were orange, 20% yellow and 47% green. Triage Early Warning Score was correctly calculated in 90% of cases and there was inter-rater agreement of colour code and triage category on 92% of occasions (k = 0.877, p < 0.001). Median time from triage to assessment was 15 min for red patients, 20 min for orange, 40 min for yellow and 72 min for green.
Discussion
The triage process is functioning effectively in the emergency centre after the Ebola epidemic and provides a reliable assessment of undifferentiated patients presenting to the hospital to ensure that they are seen in a timely manner based on acuity.
Abstract
Introduction
Le triage réalisé par les infirmières, qui se base sur l’Echelle de triage sud-africaine (SATS, South African Triage Scale), a été introduit au service des urgences de l’hôpital tertiaire de référence de Freetown, en Sierra Leone, au début d’année 2014, avant l’épidémie d’Ebola. L’objectif était d’évaluer l’efficacité du processus maintenant que le risque pour le pays a été déclaré inexistant.
Méthodes : L’étude a été menée sur une période consécutive de cinq jours au service des urgences du principal hôpital universitaire public en décembre 2015. Le temps écoulé entre l’arrivée et le triage et l’examen médical a été consigné et comparé pour chaque catégorie de triage. Nous avons également évalué le coefficient d’objectivité du processus.
Résultats
111 patients ont été inclus sur la période de l’étude. En termes de gravité, 6 % étaient classés en rouge, 27 % en orange, 20 % en jaune et 47 % en vert. La note accordée aux alertes rapides découlant du triage (TEWS, Triage Early Warning Score) a été correctement calculée dans 90 % des cas et la concordance inter-évaluateurs sur les codes couleurs et les catégories de triage a été observée dans 92 % des cas (k = 0,877, p < 0,001). Le temps moyen du triage à l’examen était de 15 minute pour les patients en catégorie rouge, de 20 minute en catégorie orange, 40 minute en catégorie jaune et 72 minute en catégorie verte.
Discussion
Le processus de triage fonctionne efficacement au service des urgences après l’épidémie d’Ebola et fournit une évaluation fiable des patients non différentiés se présentant à l’hôpital, afin de s’assurer qu’ils voient un médecin en temps opportun en fonction de la gravité de leur état.
African relevance
-
•
Triage is an integral component of an emergency care system.
-
•
Triage is a new concept in many African emergency centres.
-
•
The use of the South African Triage Scale has not been previously described in Sierra Leone.
-
•
Triage can contribute to health system strengthening after an epidemic.
Introduction
Triage is recognised as an essential first step in efficient and effective emergency care. The South African Triage Scale (SATS) is a physiology and symptom based scale that categorises patients into one of four colours to determine their illness severity. It was initially developed by the South African Triage Group (SATG) in 2004 and designed for the use of a non-specialist to help triage patients effectively in a resource-limited setting [1]. The SATS has proven to be a reliable and valid method of assessment for undifferentiated ill and injured patients in South Africa and has subsequently been validated in other African countries [2], [3] and Asia [4].
Sierra Leone is ranked 181 out of 188 countries in the most recent UN Development Index [5] and the 300 bed Connaught Hospital, Freetown, with 12,000 patients annually presenting to its Emergency Centre (EC) faces serious challenges and resource limitations in delivering quality care [6]. It has been placed under further strain by the recent Ebola epidemic from a reduction in health care workers and the temporary conversion of the EC into an Ebola holding and isolation unit. The King’s Sierra Leone partnership (KSLP) has had a partnership with the Connaught Hospital for the past four years, working with local leaders to strengthen health systems and improve health service delivery.
At Connaught Hospital, patients were seen on a first come, first served basis, and mean time from registration to doctor review was as long as 149 min for severe ‘red’ patients (unpublished data from observational research) and ‘minor’ cases were often observed to be consulted by a doctor first. Therefore, in early 2014, SATS was implemented into the EC with the aim of improving recognition and management of acutely unwell patients. A two-day practical SATS training course was delivered to eight nurses by accredited SATS trainers, followed by direct supervision for one week in the department with review of all cases and then reduced direct supervision thereafter by the in-country KSLP team. And indeed, a follow-up study of 101 patients in March 2014 demonstrated an improvement with median triage to physician review times of ten minutes for red, 57 for orange, 95 for yellow and 197 for green patients.
The Ebola epidemic, however, understandably led to deficiencies in the system and despite triaging admirably continuing throughout the outbreak, a further unpublished reliability study towards the end of the epidemic in May 2015, demonstrated that triage was being performed correctly in only 61% of cases. Subsequent to this, further one-to-one training and supervision took place with the triage staff, both in the triage room and through scenarios in the clinical skills department. The aim of this study was to assess the effectiveness and reliability of nurse-led triage following this further training in the post Ebola epidemic phase.
Methods
We conducted a prospective, single centre, observational study based at the urban EC of the government tertiary referral hospital in Freetown, Sierra Leone. The primary objective was to assess the ability of nurses to triage by examining the reliability of the process, and the secondary outcome was to evaluate effectiveness through time spent in the department; specifically, time from triage to assessment.
Data were collected from consecutive patients attending the EC during the early shift between 08 h 00 and 13 h 00 over a five-day period from 7th to 11th December 2015. The country was first declared free of Ebola on 7th November 2015. We included all new patients over the age of twelve years who attended the EC that were subsequently assessed by the triage staff. Patients over the age of twelve are assessed according to the Adults SATS chart. We excluded all patients that were attending for follow-up consultations.
Data were collected on baseline demographic characteristics. Times were recorded from point of registration through to discharge from the department or admission to the ward. Data were entered into a triage audit tool contemporaneously by two emergency physicians that were not involved in the assessment process. Triage Early Warning Score (TEWS) and colour classification were recorded by a Sierra Leonean nurse trained in the triage process and patients were subsequently reviewed by an experienced Medical Officer or Community Health Officer.
Triage was simultaneously conducted and scored by an expert Norwegian emergency centre nurse, experienced in the process and training of triage and the results were compared between the two assessors to examine the reliability of the process. The triage assessors were blinded to each other’s scoring. Agreement was based firstly on the two nurses calculating the same TEWS score from the physiological parameters recorded by a separate nurse, and secondly, their colour category allocation based on their individual assessment of clinical signs. Data was collected on outcome at 24 h and the diagnosis was taken from the EC medical records.
Data were managed and analysed using SPSS statistical V22 software package. Categorical data were expressed as percentage, while continuous data were expressed in terms of means and medians where appropriate. For the purpose of significance testing, a P-value less than 0.05 was considered statistically significant. The study was part of a service evaluation run by Connaught Hospital supported by King’s Sierra Leone Partnership aimed at improving patient care in the Emergency Centre.
Results
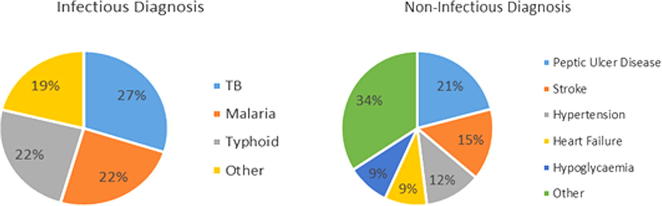
During the study period, a total of 115 patients were assessed at the triage point. Four were excluded, as they were under the age of twelve years, leaving 111 patients that were included in the analysis. Of these patients, 52% were male and 48% were female. The mean age for all patients was 41 years (range 17–82). Nine patients were uncertain of their exact age and were classed as adult (Fig. 1).
Fig. 1.
Age distribution of patients.
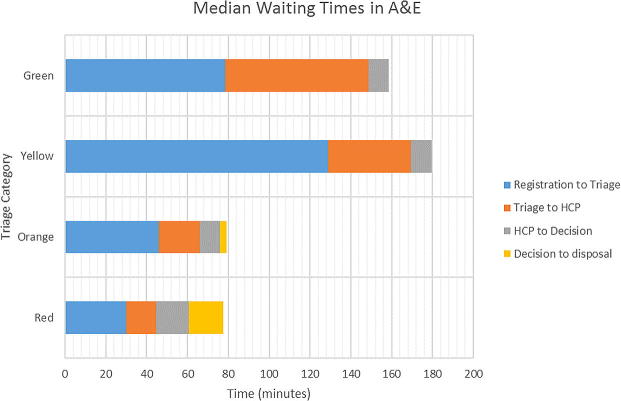
Sixty-eight percent of diagnoses were medical conditions, followed by surgical (12%), trauma (12%) and gynaecology (4%) (Fig. 2). The remainder were made up of dermatology and ENT conditions while one patient was triaged but not seen by a clinician, the assumption being that they did not wait to be seen. HIV is currently not routinely tested in the EC so the prevalence in this cohort is uncertain.
Fig. 2.
Medical diagnoses. TB, tuberculosis.
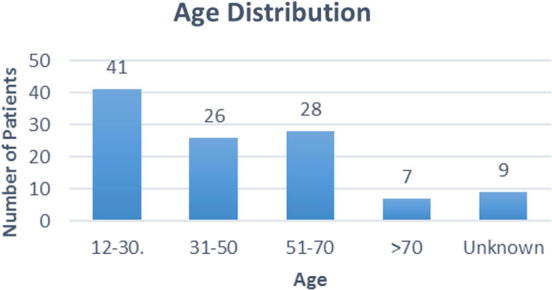
In terms of acuity breakdown, 6% of cases were red, 27% orange, 20% yellow and 47% green. The median waiting times and ranges for each triage category are shown in Table 1.
Table 1.
Patient wait from registration to triage and review by health care practitioner according to triage category.
| Acuity | Registration to Triage Time Median (Range) in minutes |
Triage to HCP Review Median (Range) in minutes |
|---|---|---|
| Red (n = 7) | 30 (5–148) | 15 (5–34) |
| Orange (n = 30) | 46 (3–165) | 20 (8–126) |
| Yellow (n = 22) | 129 (30–190) | 40 (12–157) |
| Green (n = 52) | 80 (11–192) | 72 (6–138) |
HCP, health care practitioner.
TEWS was correctly calculated on 90% of occasions and the correct triage colour code was assigned 92% of the time when the triage nurse form was compared with that of the nurse expert observer (k = 0.877, p < 0.001). TEWS scores were calculated differently between the nurse and expert in ten cases but this only led to a different colour category on four occasions, two patients were under-triaged by one colour category and the other two were over-triaged. The other discrepancy in colour category between the two assessors resulted from different interpretations of pain severity.
After assessment by a health care practitioner, 80% of patients were subsequently discharged. Nineteen percent were admitted and one patient was transferred to another hospital. The majority (60%) were admitted to the acute medical unit, 15% were admitted to the surgical admissions unit, and of the rest, one was admitted to the private wing and the others were admitted directly to a hospital general ward. Of the patients admitted, 90% (n = 18) were category red or orange.
Time from health care practitioner assessment to discharge from the doctor’s office or ward admission are shown in Table 2.
Table 2.
Time from review by health care practitioner to disposal decision and subsequent departure from the emergency centre according to triage category.
| Acuity | HCP Review to Decision Time Median (Range) in minutes |
Decision to Disposal Time Median (Range) in minutes |
|---|---|---|
| Red (n = 7) | 16 (6–105) | 17 (0–88) |
| Orange (n = 30) | 10 (2–83) | 3 (0–1454) |
| Yellow (n = 22) | 10 (6–22) | 0 (0–20) |
| Green (n = 52) | 10 (0–38) | 0 (0–73) |
HCP, health care practitioner.
For those admitted to medical observation, the median wait for a bed after decision to admit was 16 min (range 5–1445). One patient waited overnight in the EC for a bed to become available and was admitted from the resus bed in triage the following day. Time of decision was recorded when the health care practitioner informed the nursing staff of the plan, subsequent to which, many patients immediately left the department if they were discharged. This explains why many patients had a decision to disposition time of zero minutes (Fig. 3).
Fig. 3.
Median waiting times for patients during emergency centre attendance. HCP, health care practitioner.
All 21 patients admitted were followed up at 24 h. At this stage, one patient had died, one patient had been transferred to intensive care, three had been discharged and the rest were still on the wards. The patient that died was a 65-year-old female brought in unconscious, diagnosed with stroke and had initially been triaged as a category orange patient (TEWS 5).
Discussion
It can be seen that the majority of patients attending the Emergency Centre are from a young demographic, with a mean age of 41 years. This is consistent with the population spread in which the majority are below the age of 55 years [7]. There is a high acuity of illness amongst those that present. One-third of patients were in triage category orange or red and 90% of the hospital admissions came from this group of patients, suggesting that the TEWS score and colour category are reasonable predictors of patients that will require inpatient management.
In terms of the triage system; with 92% inter-observer agreement on colour category, the system appears reliable. It is also functioning effectively as far as ensuring that the higher acuity patients are prioritised after triage assessment. Red patients are seen in the quickest time after triage, followed by orange, then yellow and green. The median waiting times for red and orange patients are shorter for triage and health care practitioner assessment than yellow and green patients. Once triaged, category red patients wait a median of 15 min to see a health care practitioner, while orange wait 20 min. This is considerably faster than 40 min for yellow and 72 min for green.
Once patients are seen by a health care practitioner, a decision is generally made quickly as to further management i.e. discharge or admit. During the study period, patients on the whole do not wait for long periods of time for a bed. Although not specifically looking at the triage effectiveness, it is important to note that the main wait patients have is from registration to triage assessment and this is a concern because it may mean that high acuity patients stay in the waiting room un-assessed for prolonged periods of time. Red and orange patients do, however, experience a shorter wait from registration to triage than yellow and green and this is most likely to be due to triage nurses and registration officers identifying sicker looking patients for triage assessment, possibly due to greater awareness of the need to prioritise these patients subsequent to training.
As a result of this study, several changes to service have been made. These include the implementation of 24-h triage, where it previously finished at 20h00, a designated area for triage and resuscitation, and refurbishment of the department with increased capacity to manage the large volume of high acuity patients that present. In addition, training through the use of simulation, triage refreshers and guideline production has begun to improve recognition and management of sick patients, with an emphasis on communication between staff. There is a plan in place for regular audit of the process.
When compared to others studies of triage conducted in the African context, our study supports previously obtained results indicating the improved quality in service delivery utilising the triage tool. The effectiveness of the SATS has been measured in several studies that conclude that it is a valid method of assessment by nurses for undifferentiated ill and injured patients in both urban and rural, low-resource settings [2], [3], [8]. In addition, it has been proven to significantly reduce waiting times of critically ill patients [9].
In a cross-sectional reliability study in a South African urban emergency centre in 2012, inter-rater reliability between expert triagers and the study group was measured and the average exact agreement was 84% [2]. In an urban hospital in Pakistan, inter-rater reliability measures demonstrated 87% reliability between nurses and expert triagers [4]. Our figure of 92% inter-rater agreement compares favourably with these results. Although SATS has been assessed in certain low-income settings, its utilisation has never been described immediately after a major epidemic, such as Ebola.
Emergency care capacity in Freetown is extremely limited [10] and Connaught is the first government hospital in the country to use a validated triage tool. This study is of great importance for several reasons. It demonstrates that triage using the SATS is not only reliable but valid in this context. It also supports the need for triage and emergency care services in this setting, with a burden of red and orange cases at 33% and a high admission rate. Furthermore, this study is of interest as SATS was implemented prior to the Ebola epidemic and was maintained throughout, which is unique in the reported literature. In addition, a study of attendances at Connaught during the epidemic [11] demonstrated that although the number of attendances decreased during the height of the outbreak, the proportion of high acuity cases increased supporting the need for an effective triage system even during the height of an outbreak.
The main limitations of the study are the small numbers involved and the fact that it was only conducted during the early shift in a single centre. We decided to study this time as the early shift is the busiest period that sees the majority of attendances. Connaught is the only site in the city that uses SATS currently. It is not possible to draw conclusions on the validity and reliability of triage during the late shift that has less manpower. Now that triaging occurs over 24 h, we plan to conduct a further, extended review in a future study. In addition, it is possible that access to beds becomes more difficult later in the day so waiting times and exit block may become an issue that was not identified during this study. Finally, we collected data contemporaneously, so the presence of the investigators may have had an effect on performance; but it was felt that this was the best method of obtaining reliable data.
A secondary non-measured, but observed positive outcome from this study has been the improved capacity amongst the staff to work independently with confidence and enthusiasm for their own professional development, creating much needed role models. The hard-working and dedicated staff have not only ensured that this process has continued throughout the Ebola epidemic but it has actually developed into a robust system which can serve as a model for adoption in other hospitals throughout the country.
Our data demonstrates a burden of disease and age spectrum consistent with other sub-Saharan African countries [12], suggesting that the validity could be generalised to other urban low-income settings. Emergency care has been recognised by the Ministry of Health and Sanitation in Sierra Leone as an essential healthcare service [13] and triage should form an integral component of the system. This study should lead to expansion and national roll-out of triage training across Sierra Leone with accompanying research to test the validity and reliability of the SATS in other settings. The aim would be to inform national policy development with the ultimate hope of reducing morbidity and mortality. In the post-Ebola recovery period, with the emphasis on health system strengthening, there is no better time.
Conflicts of interest
The authors declare no conflicts of interest.
Dissemination of results
Results of this study were presented to the department staff at the weekly training meeting. A written report was also prepared for the hospital management committee. The Sister in charge presented the study at the National Health and Biomedical Sciences Research Conference in Freetown.
Authors’ contributions
HLH and CK conceived the original idea. HLH, RL and HN designed the study. HN, NW, MK collected the data along with HLH and RL. All authors contributed to drafting the manuscript with critical revision from MB. All authors approved the final version that was submitted.
Acknowledgements
The authors would like to thank Mohamed ElSherbiny, Paul Arkell, Daniel Youkee, James Barnacle and Anna Davies for their contributions to data and triage development in Sierra Leone. This work has only been possible due to the work of all the triage nurses at Connaught Hospital, especially Sister Hajara Serry who was instrumental in developing the system prior to the outbreak.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
References
- 1.Gottschalk S., Wood D., DeVries S., Wallis L.A., Bruijins S., on behalf of the Cape Triage Group The cape triage score: a new triage system South Africa. Proposal from the Cape triage group. Emerg Med J. 2006;23:149–153. doi: 10.1136/emj.2005.028332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Twomey M., Wallis L., Thompson M.L., Myers J.E. The South African triage scale (adult version) provides valid ratings when used by doctors and enrolled nursing assistants. Afr J Emerg Med. 2012;2(1):3–12. doi: 10.1016/j.ienj.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Rominski S. The validity of the South African Triage Scale at a tertiary care centre, Kumasi, Ghana. Afr J Emerg Med. 2013;3(4):S8–S9. [Google Scholar]
- 4.Dalwai M., Twomey M., Maikere J., Said S., Wakeel M., Jemmy J.P. Reliability and accuracy of the South African Triage Scale when used by nurses in the emergency department of Timergara Hospital, Pakistan. S Afr Med J. 2014;104(5):372–375. doi: 10.7196/samj.7604. [DOI] [PubMed] [Google Scholar]
- 5.United Nations. Human Development Report 2015. Work for human development. United Nations Development Program. [Internet] <http://hdr.undp.org/sites/default/files/2015_human_development_report.pdf> (accessed July 2016).
- 6.Ministry of Health and Sanitation. Connaught Hospital Taskforce Report. Government of Sierra Leone 2013.
- 7.Nationmaster. Sierra Leone Age Structure Stats. [Internet] <http://www.nationmaster.com/country-info/profiles/Sierra-Leone/People/Age-structure> (accessed July 2016).
- 8.Mullan P., Torrey S., Chandra A., Caruso N., Kestler A. Reduced overtriage and undertriage with a new triage system in an urban accident and emergency department in Botswana: a cohort study. Emerg Med J. 2014;31:356–360. doi: 10.1136/emermed-2012-201900. [DOI] [PubMed] [Google Scholar]
- 9.Bruijns S.R., Wallis L.A., Burch V.C. Effect of introduction of nurse triage on waiting times in a South African emergency department. Emerg Med J. 2008;25(7):395–397. doi: 10.1136/emj.2007.049411. [DOI] [PubMed] [Google Scholar]
- 10.Coyle R., Harrison H. Emergency care capacity in Freetown, Sierra Leone: a service evaluation. BMC Emerg Med. 2015;15:2. doi: 10.1186/s12873-015-0027-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Youkee D., Williams N., Laggah M. The impact of the 2014–15 Ebola virus disease epidemic on emergency care attendance and capacity at a tertiary referral hospital in Freetown, Sierra Leone: a retrospective observational study [abstract] Lancet. 2016;387:S109. [Google Scholar]
- 12.Wachira B., Wallis L.A., Geduld H. An analysis of the clinical practice of emergency medicine in public emergency departments in Kenya. Emerg Med J. 2012;29:473–476. doi: 10.1136/emj.2011.113753. [DOI] [PubMed] [Google Scholar]
- 13.Ministry of Health and Sanitation . Government of Sierra Leone; 2015. Sierra Leone basic package of essential health services 2015–2020. [Google Scholar]