Abstract
Objective
To examine the long‐term reliance on outpatient care at the population (i.e., system) level among fee‐for‐service Medicare‐enrolled elderly veterans in the Department of Veterans Affairs (VA) health care system and Medicare from 2003 to 2014.
Data Sources/Study Setting
We analyzed a 5 percent random sample, stratified by facility, age, gender, and race, of Medicare‐enrolled veterans enrolled in a VA primary care panel using VA administrative data and Medicare claims.
Study Design
We performed a repeated cross‐sectional analysis over 48 quarters. VA reliance was defined at the system level as the proportion of total visits (VA + Medicare) that occurred in VA. We examined four visit types and seven high‐volume medical subspecialties. We applied direct standardization adjusting for age, gender, and race using the 2010 population distribution of Medicare‐enrolled veterans.
Principal Findings
Over the 12‐year period, VA provided the vast majority of mental health care. Conversely, veterans received slightly more than half of their primary care and most of their specialty care, surgical care, and seven high‐volume medical subspecialties through Medicare. However, reliance on VA outpatient care steadily increased over time for all categories of care.
Conclusions
Despite the controversies about VA access to care, Medicare‐enrolled veterans, who have a choice of using VA or Medicare providers, appear to increase their use of VA care prior to the Choice Act.
Keywords: VA, Medicare, primary care
The Department of Veterans Affairs (VA) health care system is one of the largest integrated health care systems in the United States having served 8.4 million veteran enrollees in 2016 (Huang et al. 2017). In recent years, demand for care has exceeded the VA's capacity, resulting in reports of veterans experiencing long wait times for care being sought at VA health care facilities. In 2014, VA implemented the Veterans Choice Program as part of the Veterans Access, Choice, and Accountability Act (“Choice Act”), allowing veterans to receive care from community providers if the expected wait time for a VA appointment is greater than 30 days or if the nearest VA provider is greater than 40 miles away. VA is currently working on a new community care program to succeed the Choice Program that will continue to provide timely care through community providers with an emphasis on coordination of VA and community care through the new Mission Act (Isakson 2018).
Veterans Affairs has a long history of providing community care to veterans based on clinical needs through the fee‐basis program. The current community care program allows veterans to choose whether to see a community or VA provider for their care (U.S. Department of Veterans Affairs 2018). One unanswered question is how veterans will choose between VA and community providers when given the choice.
In an era of increasing community care options, understanding how Medicare‐enrolled veterans choose between VA and Medicare can help policy makers predict expected use of VA and non‐VA care through programs such as Choice Program. Dual VA‐Medicare enrollees have historically had the choice of using services from VA, community providers via Medicare, or both. Prior research has demonstrated dual use of outpatient services has been common (Hynes et al. 2007; Liu et al. 2010; Humensky et al. 2012). In 2016, 52 percent of all VA enrollees were also covered by Medicare, including 92 percent of enrollees age 65+ (Huang et al. 2017). However, prior studies in dual use of VA and Medicare are mostly cross‐sectional, use data from late 1990s to early 2000s (Hynes et al. 2007; Humensky et al. 2012), or are focused on subpopulations (Zhu et al. 2009; Fischer et al. 2010; Radomski et al. 2016). No research has assessed population‐ or system‐level changes in VA reliance on outpatient care among Medicare‐enrolled veterans over an extended time period (≥5 years) and across an extensive array of outpatient service types.
We sought to examine long‐term trends in reliance on VA outpatient care at the system level among Medicare‐enrolled veterans from the fiscal year (FY) 2003 to FY2014. We separately examined four visit types (primary care, mental health, specialty care, and surgery) and seven high‐volume medical subspecialties (cardiology, ophthalmology, critical care/pulmonology, nephrology, dermatology, gastroenterology, and hematology oncology).
Methods
Data Linkage
The data sources included VA administrative datasets from the VA Corporate Data Warehouse (CDW) (U.S. Department of Veterans Affairs 172VA10P2 2012; Fihn et al. 2014) and Medicare claims (Hynes et al. 2007; US Department of Veterans Affairs 2015). The VA Information Resource Center (VIReC) provided linked Medicare and VA enrollee files for FY 2003–2014 (Hynes et al. 2007). Patients who were on a VA primary care panel were identified from the Primary Care Management Module (PCMM) within CDW. Data on VA health care use were obtained from the outpatient visit tables within the VA CDW. These data contain encounter‐level records that track the services and procedures delivered at a visit defined by Common Procedure Terminology (CPT) codes, provider type, and place of service captured in VA using clinic stop codes representing the type of care provided at a given outpatient clinic (e.g., primary care and cardiology). Data on Medicare eligibility and coverage were obtained from the Medicare Master Beneficiary Summary file. Data on Medicare health care use were derived from the physician/supplier files, which also include CPT codes and codes to identify the type of provider and place of service. Place of service codes was restricted to noninstitutional, nonhospital settings and excluded emergency department (ED) or ambulance claims. We used the VA scrambled social security number to link datasets.
Study Sample
We employed a repeated cross‐sectional design. Our sampling frame comprised 24 million patient‐years of elderly veterans who were 65 years or older and listed on a VA primary care panel from FY2003 to FY2014 (Figure 1), with a total of 5 million unique patients over the time period. A 5 percent stratified random sample of patients was independently drawn in each facility and each year. First, we stratified patients by gender and seven race categories (American Indian/Alaskan Native, Asian, black, multiple race, Native Hawaiian/Pacific Islander, white, and other/unknown). We excluded the cells with fewer than 20 patients with a total of 39,109 patient‐years excluded during the entire study period. Then, we drew a 5 percent random sample from each of the 14 cells resulting from stratification. Random sampling yielded 1,186,148 patient‐years. We excluded patients not enrolled in Medicare Part B (n = 93,874 patient‐years) or enrolled in Medicare Advantage plans (n = 219,983 patient‐years). The final sample included 872,291 patient‐years of elderly veterans who enrolled in VA primary care and had Medicare fee‐for‐service (FFS) coverage. We constructed our analytic dataset by calendar quarter, which included 63,000 to 87,000 elderly Medicare‐enrolled veterans per quarter.
Figure 1.
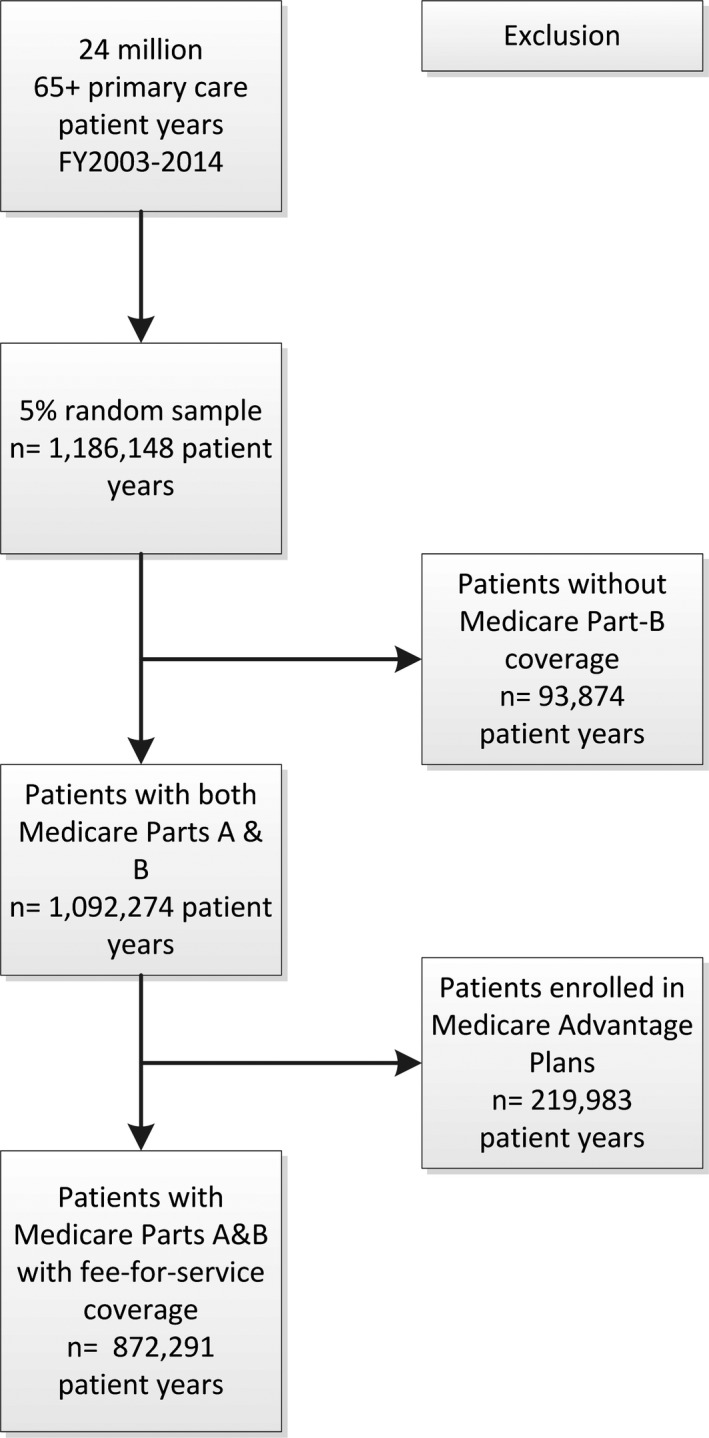
Study Sample Selection
Classification of Outpatient Services
We adapted a hierarchical classification algorithm developed by Burgess et al. (2011) to measure the outpatient use in VA and Medicare. This algorithm uses common data elements present in administrative data, including CPT codes and provider specialty, to preserve comparability in measures between systems. We included face‐to‐face encounters with physicians, nurse practitioners (NPs), physician assistants (PAs), and nonphysician mental health providers (e.g., psychologists and social workers). We excluded all encounters that occurred in EDs indicated by the location of care due to a data capture issue in VA ED visits prior to 2008 (Hebert et al. 2014).
Briefly, a visit was defined as a unique combination of date, CPT code, and provider specialty. First, visits were defined as primary care if a visit was rendered by a general internal medicine, family medicine, or geriatric provider. Second, any remaining visits were defined as mental health if the corresponding CPT code was considered a psychiatry evaluation and management office visit or if the provider of record was classified as mental health specialist (e.g., psychiatrist, psychologist, and social worker). Third, remaining records after excluding primary care and mental health visits that indicated the provider of record was a surgeon were classified as surgery care. Fourth, unclassified visits from the first three steps where care was provided by a medical subspecialist were defined as specialty care. Finally, we distributed NP/PA visits across the four visit types, because NPs/PAs can practice in different specialties and the NP/PA specialty codes were not available during the study period. In the VA, we assigned an NP/PA visit to the specialty according to the clinic stop code that identified the clinic specialty. Because no equivalent of VA clinic stop code existed in Medicare claims, we attributed NP/PA visits based on the ratio of physician specialties within the medical group where NPs/PA practiced. A medical group was defined as a group of providers within the same tax identification number according to the Medicare carrier claims (Center for Medicare & Medicaid Services).
Finally, if records showed a patient made two or more visits to a primary care provider on the same day, we counted only one primary care visit. If records showed a patient made one visit to a primary care provider and one visit to a cardiology on the same day, it was counted as one primary care visit and one cardiology visit.
For specialty care, we further examined VA reliance time trends for the top seven high‐volume medical subspecialties based on the total number of VA and Medicare visits including cardiology, ophthalmology, critical care/pulmonology, nephrology, dermatology, gastroenterology, and hematology oncology. Visits to these specialties were identified through the provider specialty code.
VA Reliance Measure
We measured VA reliance at the system level for each visit type by calculating the proportion of all visits (VA + Medicare) that occurred in VA in a quarter. The VA reliance measure ranged from 0 to 1, with 0 indicating 100 percent of visits occurred in Medicare and 1 indicating 100 percent of visits occurred in VA. We repeated this calculation for each calendar quarter and derived trajectories using the 48 quarterly reliance measures. Reliance trajectories were separately calculated for each visit type and for the seven medical subspecialties.
To further discern whether trajectories in VA reliance were due to changes in the proportion of visits sought from VA versus Medicare or changes in the overall use of a given visit type, we constructed three variables for each visit measure in each quarter: (1) the VA/Medicare user status (VA‐only user, Medicare‐only user, and dual user), (2) the number of VA visits per VA user, including VA‐only users and dual users, and (3) the number of Medicare visits per Medicare user, including Medicare‐only users and dual users.
Statistical Analysis
We performed a repeated cross‐sectional analysis by 48 calendar quarters to describe time trends in VA reliance. As the reliance measure was at the system level, we applied a direct standardization to adjust for age, gender, and race using the population distribution of elderly Medicare‐enrolled veterans in 2010, the year when the VA implemented the patient‐centered medical home model systemwide. We grouped age into five categories (65–69, 70–74, 75–79, 80–84, and 85+), gender into two categories (male and female), and race into seven categories (American Indian/Alaskan Native, Asian, black, multiple race, Native Hawaiian/Pacific Islander, white, and other/unknown).
Results
Elderly Medicare‐Enrolled Veterans
The number of elderly veterans enrolled in VA and FFS Medicare was 1.7 million in 2003Q1, which gradually decreased to 1.3 million in 2009Q1 and then gradually increased to 1.5 million in 2014Q4 (Table 1). About 90 percent of veterans per quarter had at least one VA or Medicare outpatient visit, including any primary care, mental health, specialty care, or surgical visit. The proportion of veterans in any VA visit increased from 55 percent in 2003Q1 to 62 percent in 2014Q4. In contrast, the proportion of veterans in any Medicare visit decreased from 63 percent in 2003Q1 to 52 percent in 2014Q4. The proportion of dual use in VA and Medicare was about 30 percent per quarter.
Table 1.
Population Distribution by Age, Gender, and Race
| 2003Q1 | 2006Q1 | 2009Q1 | 2012Q1 | 2014Q4 | |
|---|---|---|---|---|---|
| Sample size | 86,053 | 77,617 | 63,409 | 68,793 | 73,087 |
| Estimated population size (in millions) | 1.7 | 1.6 | 1.3 | 1.4 | 1.5 |
| Mean age (year, SD) | 75.7 (6.0) | 76.8 (6.5) | 77.2 (7.3) | 75.8 (7.9) | 73.7 (8.10) |
| Any use in VA or Medicare* % | 88 | 89 | 90 | 88 | 86 |
| Any use in VA % | 55 | 58 | 58 | 61 | 62 |
| Any use in Medicare % | 63 | 66 | 65 | 58 | 52 |
| Dual use of VA and Medicare % | 30 | 34 | 34 | 31 | 29 |
| Age (%) | |||||
| 65–69 | 18 | 16 | 20 | 33 | 45 |
| 70–74 | 27 | 24 | 19 | 17 | 18 |
| 75–79 | 27 | 23 | 16 | 12 | 11 |
| 80–85 | 20 | 23 | 20 | 16 | 12 |
| 85+ | 8 | 11 | 19 | 19 | 14 |
| Gender (%) | |||||
| Male | 98 | 98 | 98 | 98 | 98 |
| Female | 2 | 2 | 2 | 2 | 2 |
| Race (%) | |||||
| American Indian/Alaskan Native | 0 | 0 | 0 | 1 | 1 |
| Asian | 0 | 0 | 0 | 0 | 1 |
| Black | 7 | 7 | 7 | 8 | 9 |
| Multiple race | 0 | 0 | 1 | 1 | 1 |
| Native Hawaiian/Pacific Islander | 0 | 1 | 1 | 1 | 1 |
| White | 91 | 91 | 90 | 89 | 87 |
| Other/unknown | 1 | 1 | 1 | 1 | 1 |
Including outpatient visits in primary care, mental health, specialty care, and surgical care.
Demographic characteristics of elderly‐enrolled veterans varied substantially over time, specifically regarding age and race (Table 1). The mean age was 75.7 years in 2003Q1, which increased to 77.2 years in 2009Q1 and then decreased to 73.7 years in 2014Q4. The decrease in age stemmed from the increase in the number of veterans aged 65–69 (18 percent in 2003Q1 to 45 percent in 2014Q4). The proportion of white veterans decreased from 91 percent in 2003Q1 to 87 percent in 2014Q4. Conversely, the proportion of black veterans increased from 7 percent in 2003Q1 to 9 percent in 2014Q4.
VA Reliance by Visit Type after Direct Standardization
Most Medicare‐enrolled veterans relied on VA for most of their mental health care with a stable time trend from 2003Q1 (75 percent) to 2014Q4 (77 percent). Conversely, veterans relied on Medicare for most of their primary care, specialty care, and surgical care (Figure 2). However, time trends from 2003Q1 to 2014Q4 showed VA reliance increased for primary care (25 percent to 35 percent), specialty care (14 percent to 22 percent), and surgical care (15 percent to 22 percent).
Figure 2.
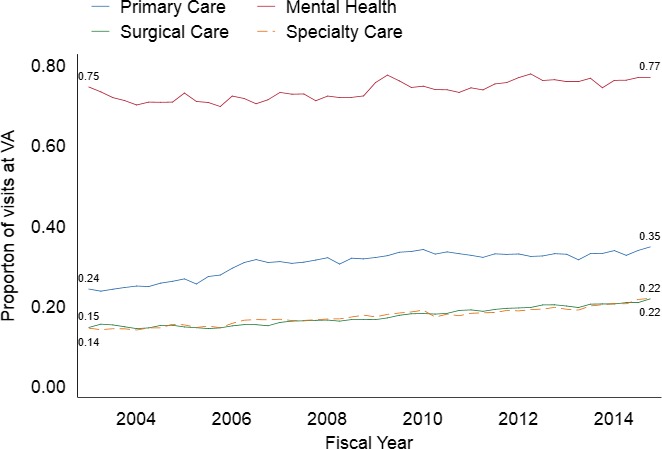
Veterans Affairs Reliance by Visit Type After Direct Standardization, FY2003–FY2014 [Color figure can be viewed at http://wileyonlinelibrary.com]
VA/Medicare User Status by Visit Type After Direct Standardization
Similar time trends in VA/Medicare user status were observed for all visit types. There was a decrease in Medicare‐only users, an increase in VA‐only users, and a small and stable number of dual users (Figure 3). Further, the number of Medicare visits per Medicare user and the number of VA visits per VA user were stable over time for all visit types.
Figure 3.
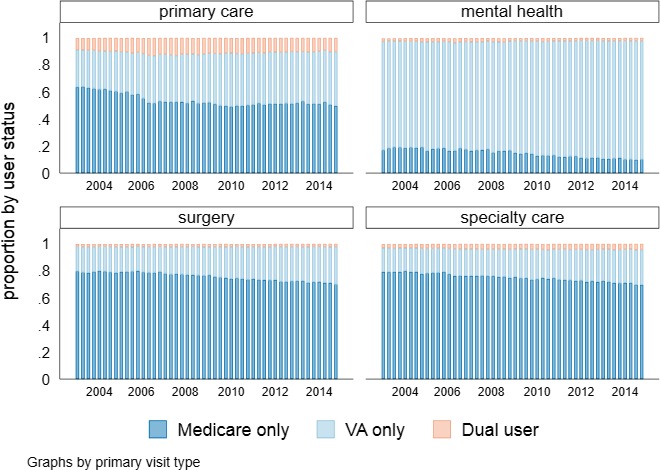
Veterans Affairs/Medicare User Status Among Users by Visit Type After Direct Standardization, FY2003–FY2014 [Color figure can be viewed at http://wileyonlinelibrary.com]
Primary Care
More than two‐fifths of Medicare‐enrolled veterans used any primary care in a quarter, ranging from 41 percent to 46 percent. Among primary care users, Medicare‐only users decreased over time from 64 percent in 2003Q1 to 50 percent in 2014Q4, VA‐only users increased from 28 percent to 40 percent, and dual users were stable over time around 9–13 percent (Figure 2). The number of primary visits per user was stable over time. The numbers of Medicare primary care visits per Medicare user were in the range of 1.6–1.8 visits, while the numbers of VA visits per VA user were in the range of 1.1–1.2 visits.
Mental Health
While only a small proportion of Medicare‐enrolled veterans had any mental health utilization, the overall percentage increased from 6 percent in 2003Q1 to 12 percent in 2014Q4. Among mental health care users, Medicare‐only users decreased over time from 17 percent to 10 percent, while VA‐only users increased from 80 percent to 88 percent (Figure 3). The proportion of dual users was small and stable over time, around 2 percent to 3 percent. The number of Medicare mental health care visits per Medicare user was in the range of 2.7 to 3.3 visits, while the number of VA visits per VA user was in the range of 2.0 to 2.4 visits.
Surgical Care
About a quarter of Medicare‐enrolled veterans used surgical care over the study period (23–25 percent). Among surgical care users (Figure 3), Medicare‐only users decreased from 80 percent in 2003Q1 to 70 percent in 2014Q4, while VA‐only users increased from 18 percent to 28 percent. The proportion of dual users was small and stable at about 1 percent to 2 percent. The numbers of Medicare surgical visits per Medicare user were about two visits, and the numbers of VA visits per VA user were about 1.5 visits over time.
Specialty Care
The proportion of Medicare‐enrolled veterans who used specialty care in each quarter increased from 29 percent in 2003Q1 to 35 percent in 2014Q4. Among specialty care users, Medicare‐only users decreased from 79 percent to 70 percent, while VA‐only users increased from 18 percent to 26 percent (Figure 3). The proportion of dual users was small, around 3 percent to 4 percent. The numbers of Medicare specialty care visits per Medicare user were in the range of 1.8 to two visits, while the numbers of VA visits per VA user were in the range of 1.3 to 1.4 visits.
VA Reliance by Medical Subspecialty after Direct Standardization
Elderly Medicare‐enrolled veterans relied mostly on Medicare for the seven high‐volume medical subspecialties. However, time trends in VA reliance increased for all specialties from 2003Q1 to 2014Q4, including cardiology (12 percent to 25 percent), ophthalmology (15 percent to 32 percent), dermatology (14 percent to 26 percent), oncology (19 percent to 30 percent), critical care/pulmonology (23 percent to 33 percent), gastroenterology (20 percent to 31 percent), and nephrology (21 percent to 35 percent) (Figure 4).
Figure 4.
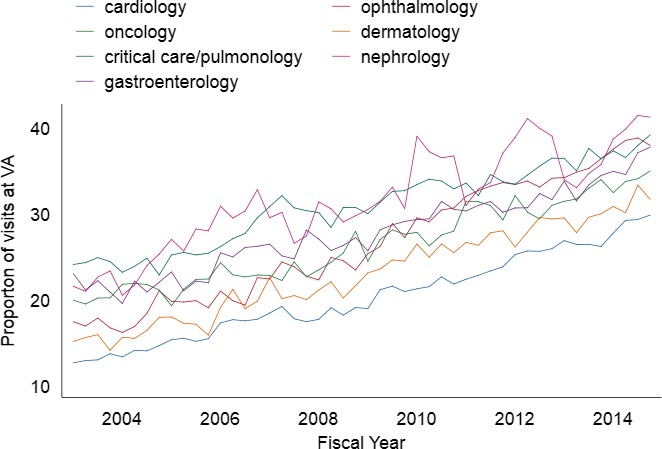
Veterans Affairs Reliance by Medical Subspecialty After Direct Standardization, FY2003–FY2014 [Color figure can be viewed at http://wileyonlinelibrary.com]
VA/Medicare User Status by Medical Subspecialty after Direct Standardization
The similar time trends in VA/Medicare user status for visit types were also observed in the seven medical subspecialties. Specifically, we identified a decrease in Medicare‐only users, an increase in VA‐only users, and a small and stable proportion of dual users (Figure 5). Further, the number of Medicare visits per Medicare user and the number of VA visits per VA user were stable over time for all medical subspecialties.
Figure 5.
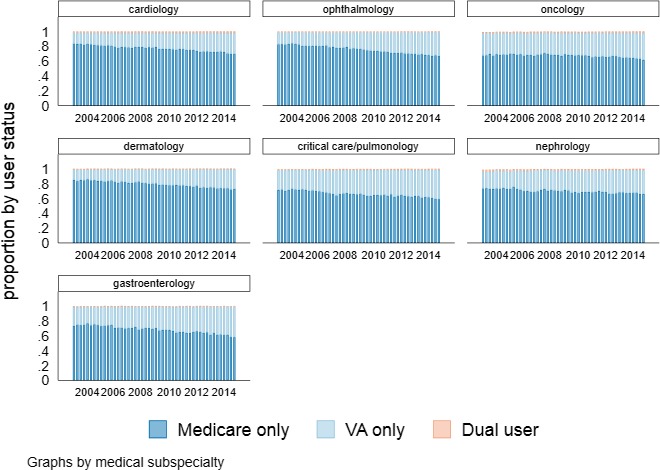
Veterans Affairs/Medicare User Status Among Users by Medical Subspecialty After Direct Standardization, FY2003–FY2014 [Color figure can be viewed at http://wileyonlinelibrary.com]
Cardiology
About one‐fifth of Medicare‐enrolled veterans used cardiology care in a quarter (17 percent to 20 percent). Among cardiology users, Medicare‐only users decreased from 83 percent in 2003Q1 to 67 percent in 2014Q3, while VA‐only users increased from 15 percent to 28 percent (Figure 5). The number of Medicare visits per Medicare user was about 1.8 to 2, and the number of VA visits per VA user was about 1.3 to 1.5.
Ophthalmology
About 13 percent to 14 percent of Medicare‐enrolled veterans used ophthalmology in a quarter. Among ophthalmology users, Medicare‐only users decreased from 84 percent in 2003Q1 to 70 percent in 2014Q3, while VA‐only users increased from 16 percent to 31 percent (Figure 5). The number of Medicare visits per Medicare user was about 1.4 to 1.6 visit, and the number of VA visits per VA user was about 1.2 to 1.6.
Dermatology
About 7 percent to 10 percent of Medicare‐enrolled veterans used dermatology in a quarter. Among dermatology users, Medicare‐only users decreased from 85 percent in 2003Q1 to 73 percent in 2014Q3, while VA‐only users increased from 15 percent to 27 percent (Figure 5). The number of Medicare visits per Medicare user was about 1.6, and the number of VA visits per VA user was about 1.2.
Oncology
About 13 percent to 14 percent of Medicare‐enrolled veterans used oncology in a quarter. Among oncology users, Medicare‐only users decreased from 68 percent in 2003Q1 to 61 percent in 2014Q3, while VA‐only users increased from 30 percent to 36 percent (Figure 5). The number of Medicare visits per Medicare user was about 2.8 to 3.6, and the number of VA visits per VA user was about 1.7 to 2.3.
Critical Care/Pulmonology
About 4 percent to 5 percent of Medicare‐enrolled veterans used critical care/pulmonology in a quarter. Among critical care/pulmonology users, Medicare‐only users decreased from 71 percent in 2003Q1 to 59 percent in 2014Q3, while VA‐only users increased from 27 percent to 39 percent (Figure 5). The number of Medicare visits per Medicare user was about 1.5 to 1.7, and the number of VA visits per VA user was about 1.4.
Gastroenterology
About 4 percent to 5 percent of Medicare‐enrolled veterans used gastroenterology in a quarter. Among gastroenterology users, the Medicare‐only users decreased from 73 percent in 2003Q1 to 58 percent in 2014Q3, while VA‐only users increased from 26 percent to 41 percent (Figure 5). The number of Medicare visits per Medicare user was about 1.5, and the number of VA visits per VA user was about 1.3.
Nephrology
About 2 percent to 3 percent of Medicare‐enrolled veterans used nephrology in a quarter. Among nephrology users, Medicare‐only users decreased from 74 percent in 2003Q1 to 66 percent in 2014Q3, while VA‐only users increased from 23 percent to 33 percent (Figure 5). The number of Medicare visits per Medicare user was about 1.6 to 2.6, and the number of VA visits per VA user was about 1.8 to 2.6.
Finally, similar time trends were observed when applying direction standardization to 2003, 2007, and 2014 for all outpatient use measures.
Discussion
This study examined long‐term (2003–2014) time trends in reliance on VA outpatient services at the system level among elderly veterans enrolled in VA and FFS Medicare. These time trends predate the implementation of the Choice Act. Over the 12‐year period, VA provided the vast majority of mental health visits. In contrast, veterans received the majority of primary care, surgical care, and specialty care (including the seven high‐volume medical subspecialties) through Medicare. However, the proportion of visits obtained from VA increased steadily over time. The results indicate the increase in VA reliance over time was driven by an increase in the proportion of veterans seeking outpatient care exclusively from VA, in conjunction with a decrease in the number of exclusive Medicare users.
This study shows that the population of elderly Medicare‐enrolled veterans, who have the option of using community providers independent of VA, are increasingly reliant on VA outpatient care at the life stage of growing health care needs across a diverse range of outpatient services. The increasing VA reliance may reflect greater satisfaction with VA care for this population. Further, while the fast‐growing VA enrollment may be contributing to long wait times in VA (Hebert and Hernandez 2016), the increasing VA reliance among elderly VA‐Medicare‐enrolled veterans may have also contributed to the increase in demand for VA care. With the ongoing commitment to expanding veterans’ access to community providers through the Choice Program and the new Mission Act (Isakson 2018), the VA policy makers should consider veterans’ preferences for VA providers even when the option of community providers is available. Notably, VA providers have specialized experience delivering care specific to the complex health care needs of veterans including service‐connected injuries, traumatic brain injuries, and post‐traumatic stress disorder.
Research examining reliance on VA relative to other systems of care, including Medicare, is limited. In addition, existing studies are from the late 1990s to early 2000s when the demographics of the VA population were different. These studies only focused on a short time period and did not measure reliance across a broad set of service types. Two studies examine VA reliance based on health care expenditures among Medicare‐eligible veterans (Hynes et al. 2007; Petersen et al. 2010). Based on the outpatient expenditure incurred in VA in 1999 among elderly FFS Medicare‐enrolled VA users in 1997–1999, Hynes et al. showed that 18 percent were VA‐only users (100 percent of expenditure in VA), 12 percent were mostly VA users (75–99 percent of expenditure in VA), 16 percent were equally dual users (26 percent–74 percent of expenditure in VA), 18 percent were mostly Medicare users (1–25 percent of expenditure in VA), and 36 percent were Medicare‐only users (0 percent of expenditure in VA) (Hynes et al. 2007). Petersen et al. (2010) found that among Medicare‐eligible veterans in 2003–2004, VA health care expenditures accounted for 51 percent of total expenditures in the 65+ population and 80 percent in the under‐65 population. A longitudinal study of a cohort of Medicare‐enrolled VA primary care users in 2000 showed veterans relied mostly on VA for their mental health care (Liu et al. 2010) and their reliance on VA primary care and specialty care decreased as they aged (Liu et al. 2011).
Compared to prior studies (Liu et al. 2010, 2011), this study showed lower overall levels of reliance on VA primary care and specialty care. In addition, these two prior studies showed that VA reliance time trends in primary care and specialty care decreased over time, and there was a smaller proportion of dual users of VA and Medicare from a longitudinal cohort of primary care patients. There are several potential explanations for these differences in terms of study design. First, we measured VA reliance by quarter, while prior studies used annual measures. Second, the prior studies used a longitudinal cohort to examine VA reliance at the patient level, while this study was a repeated cross‐sectional analysis examining reliance at the system level. Finally, the study samples from prior studies were VA primary care users, while this study randomly sampled veterans on a primary care panel, which included both VA users and nonusers. Consistent with prior studies, this study showed Medicare‐enrolled veterans relied on VA for most of their mental health care (Liu et al. 2010; Petersen et al. 2010).
Further, the results of this study provide aggregate VA reliance at the system level and do not represent the reliance at the individual level. Reliance on VA care at the individual level has been shown to be bimodal, with a high density of mostly VA‐reliant or mostly Medicare‐reliant veterans (Liu et al. 2011). Future studies should explore long‐term VA reliance at the patient level as well as the impact of patient factors and events in changing the trajectory of reliance.
This study showed significant changes in demographic characteristics among elderly Medicare‐enrolled veterans over time, which reflected fundamental changes in the period of service of the veteran population. Vietnam War veterans account for the largest proportion of the veteran population across different periods of services (U.S. Department of Veterans Affairs 2017) with an average age of 70 (Davey and Uchendu 2017). We identified a marked increase in veterans in age group 65–69 in conjunction with a decrease in white veterans over time. These demographic changes are coincident with most Vietnam era veterans aging into Medicare during the period 2000 through 2010.
The increasing reliance on VA outpatient services may be in part due to the changes in demographics and the period of service among elderly Medicare‐enrolled veterans. Veterans’ comorbidity and health care needs vary by period of service (Davey and Uchendu 2017). Vietnam War veterans have shown to incur higher VA expenditures compared to veterans in other periods of service (Davey and Uchendu 2017). Vietnam War veterans may also have different health care use patterns and care‐seeking behaviors compared to those in other periods of services. Given that the Vietnam War veterans constitute the largest proportion of elderly Medicare‐enrolled veterans, further research should examine how they use VA and Medicare services.
The study did not include veterans who were under 65 years of age and enrolled in Medicare due to disability, who have different utilization patterns compared to elderly Medicare‐enrolled veterans (Petersen et al. 2010; Liu et al. 2012). Further analysis should examine the VA reliance time trends for nonelderly Medicare‐enrolled veterans. Furthermore, we did not include outpatient visits from the VA fee‐basis program because of lack of information regarding provider specialty (Gidwani, Hong, and Murrell 2015). However, we conducted a sensitivity analysis by classifying fee‐basis visits using CPT codes only. The analysis shows that fee‐basis visits only accounted for a very small portion of total VA visits and had very little impact on VA reliance measures.
With the majority of veterans able to seek care in VA or Medicare (Huang et al. 2017), linking VA and Medicare data to understand care‐seeking behavior is essential for VA policy, planning for resource allocation to meet health care needs and coordinating care among dual users. Further, veterans’ care‐seeking behaviors change over time according to numerous factors, such as comorbid conditions, health care needs, ability to access different health care services, and changes in health care systems and health policies. Linking VA and Medicare data longitudinally are vital to observe the changes of care‐seeking behaviors over time to inform policy decisions. Observing the long‐term reliance time trends in this study provides important insight into veterans’ shifting utilization patterns between the two systems and changes in veterans’ demographics. This study focused on VA reliance at the system level, but did not assess reliance at the patient level or patient‐level factors associated with long‐term VA reliance, such as age, illness burden, exemption from VA copayments, or distance to VA facilities, which have been shown to be related to the choice of using VA and/or Medicare in prior studies (Weeks et al. 2005; Hynes et al. 2007; Liu et al. 2010, 2011; Petersen et al. 2010; Wong et al. 2016). This linked VA‐Medicare dataset from 2003 to 2014 will allow us to examine longitudinal changes in VA reliance on a broad range of services both at the system and at the patient levels.
Despite the controversies of access to VA care, elderly VA‐Medicare enrollees, who have a choice of whether to use VA or Medicare providers, appeared to have voted with their feet to increase their use of VA care prior to the implementation of the Choice Act. This study showed, over the 12‐year period, that reliance on VA outpatient care increased for primary, specialty, and surgical care, as well as the seven high‐volume medical subspecialties among elderly Medicare‐enrolled veterans. The increase in VA reliance resulted from a decrease in Medicare‐only users and an increase in VA‐only users. The changes in VA reliance may reflect several factors, including increasing preference and satisfaction for VA services, Vietnam War veterans aging into the age 65+ population, and changes in comorbidity and health care needs of veterans. In summary, the study shows that VA is the main source of mental health care and has become an increasingly important source of outpatient care for elderly Medicare‐enrolled veterans. Future research should explore the reasons for the increase in VA reliance to help VA inform policy planning around the provision of outpatient services, including the decision to expand internal VA capacity versus non‐VA community care programs.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This study was funded by the Veterans Health Administration (VHA) Patient‐Centered Medical Home Demonstration Laboratory Coordination Center (XVA‐61‐041) and VHA Investigator Initiated Grant (IIR 10‐150 Hebert). Dr. Wong is supported by a VA Health Services Research and Development Career Development Award (CDA 13‐024). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. government, the Department of Veterans Affairs, and the University of Washington.
Disclosure: None.
Disclaimer: None.
References
- Burgess, J. F. , Maciejewski M. L., Bryson C. L., Chapko M. K., Fortney J. C., Perkins M. W., Sharp N. D., and Liu C. F.. 2011. “Importance of Health System Context for Evaluating Utilization Patterns Across Systems.” Health Economics 20 (2): 239–51. [DOI] [PubMed] [Google Scholar]
- Center for Medicare & Medicaid Services . “Physician and Other Medical Provider Grouping and Patient Attribution Methodologies” [accessed on November 30, 2017]. Available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/GEM/downloads/GEMMethodologies.pdf
- Davey, V. J. , and Uchendu U. S.. 2017. “Focus on Health Equity and Action: New Vietnam Veteran Studies on Health and Mortality” VA HSR&D Cyberseminar on October 26, 2017 [accessed on August 3, 2018]. Available at https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/2383-notes.pdf [Google Scholar]
- Fihn, S. D. , Francis J., Clancy C., Nielson C., Nelson K., Rumsfeld J., Cullen T., Bates J., and Graham G. L.. 2014. “Insights From Advanced Analytics at the Veterans Health Administration.” Health Affairs 33 (7): 1203–11. [DOI] [PubMed] [Google Scholar]
- Fischer, M. J. , Stroupe K. T., Kaufman J. S., O'Hare A. M., Browning M. M., Huo Z., and Hynes D. M.. 2010. “Predialysis Nephrology Care Among Older Veterans Using Department of Veterans Affairs or Medicare‐Covered Services.” American Journal of Managed Care 16 (2): e57–66. [PubMed] [Google Scholar]
- Gidwani, R. , Hong J., and Murrell S.. 2015. Fee Basis Data: A Guide for Researchers. Menlo Park, CA: VA Palo Alto, Health Economics Resource Center. [Google Scholar]
- Hebert, P. L. , and Hernandez S. E.. 2016. “Providing Patient‐Centered Care to Veterans of all Races: Challenges and Evidence of Success.” Journal of General Internal Medicine 31 (12): 12–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert, P. L. , Liu C. F., Wong E. S., Hernandez S. E., Batten A., Lo S., Lemon J. M., Conrad D., Grembowski D., Nelson K., and Fihn S. D.. 2014. “Patient‐Centered Medical Home Initiative Produced Modest Economic Results for Veterans Health Administration, 2010–12.” Health Affairs 33: 980–7. [DOI] [PubMed] [Google Scholar]
- Huang, G. , Kim S., Gasper J., Xu Y., Bosworth T., and May L.. 2017. 2016 Survey of Veteran Enrollees’ Health and Use of Health Care. Washington, DC: Department of Veterans Affairs. Rockville, Maryland Westat. [Google Scholar]
- Humensky, J. , Carretta H., de Groot K., Brown M. M., Tarlov E., and Hynes D. M.. 2012. “Service Utilization of Veterans Dually Eligible for VA and Medicare fee‐for‐Service: 1999–2004.” Medicare & Medicaid Research Review 2 (3): E1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hynes, D. M. , Koelling K., Stroupe K., Arnold N., Mallin K., Sohn M. W., Weaver F. M., Manheim L., and Kok L.. 2007. “Veterans’ Access to and Use of Medicare and Veterans Affairs Health Care.” Medical Care 45 (3): 214–23. [DOI] [PubMed] [Google Scholar]
- Isakson, J. 2018. The VA Mission Act of 2018: The VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act. Washington, DC: U. S. Senate. [Google Scholar]
- Liu, C. F. , Chapko M. K., Bryson C. L., Burgess J. F., Fortney J. C., Perkins M. W., Sharp N. D., and Maciejewski M. L.. 2010. “Use of Outpatient Care in VA and Medicare Among Veterans Receiving Primary Care in Community‐Based and Hospital Outpatient Clinics.” Health Service Research 45 (5): 1268–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, C. F. , Manning W. G., Burgess J. F., Hebert P. L., Bryson C. L., Fortney J. C., Perkins M. W., Sharp N. D., and Maciejewski M. L.. 2011. “Reliance on VA Outpatient Care Among Medicare‐Eligible Veterans.” Medical Care 49 (10): 911–7. [DOI] [PubMed] [Google Scholar]
- Liu, C. F. , Bryson C. L., Burgess J. F., Sharp N. D., Perkins M. W., and Maciejewski M. L.. 2012. “Use of Outpatient Care in VA and Medicare Among Disability‐Eligible and Age‐Eligible Veterans.” BMC Health Services Research 12 (1): 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen, L. A. , Byrne M. M., Daw C. N., Hasche J., Reis B., and Pietz K.. 2010. “Relationship Between Clinical Conditions and use of Veterans Affairs Health Care Among Medicare‐Enrolled Veterans.” Health Services Research 45 (3): 762–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radomski, T. R. , Zhao X., Thorpe C. T., Thorpe J. M., Good C. B., Mor M. K., Fine M. J., and Gellad W. F.. 2016. “VA and Medicare Utilization Among Dually Enrolled Veterans With Type 2 Diabetes: A Latent Class Analysis.” Journal of General Internal Medicine 31 (5): 524–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs . 2015. System of Records Notice 97VA10P1: Consolidated Data Information System‐VA. [Google Scholar]
- U.S. Department of Veterans Affairs . 2017. “VA Utilization Profile FY 2016” [accessed on October 30, 2017]. Available at https://www.va.gov/vetdata/docs/Quickfacts/VA_Utilization_Profile.pdf
- U.S. Department of Veterans Affairs . 2018. “Veterans Choice Program” [accessed on August 3, 2018]. Available at https://www.va.gov/COMMUNITYCARE/programs/veterans/Choice_Program.asp
- U.S. Department of Veterans Affairs 172VA10P2 . 2012. “VHA Corporate Data Warehouse – VA. 79 FR 4377.”
- Weeks, W. B. , Bott D. M., Lamkin R. P., and Wright S. M.. 2005. “Veterans Health Administration and Medicare Outpatient Health Care Utilization by Older Rural and Urban New England Veterans.” Journal of Rural Health 21 (2): 167–71. [DOI] [PubMed] [Google Scholar]
- Wong, E. S. , Rinne S. T., Hebert P. L., Cook M., and Liu C. F.. 2016. “Hospital Distance and Readmissions Among VA‐Medicare Dual Eligible Veterans.” Journal of Rural Health 32 (4): 377–86. [DOI] [PubMed] [Google Scholar]
- Zhu, C. W. , Penrod J. D., Ross J. S., Dellenbaugh C., and Sano M.. 2009. “Use of Medicare and Department of Veterans Affairs Health Care by Veterans With Dementia: A Longitudinal Analysis.” Journal of the American Geriatrics Society 57 (10): 1908–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


