This text is excerpted from the complete document, which includes the Consortium Member Organizations and Steering Committee Representatives, Acknowledgments, Reviewers, Glossary, and Appendix (Search Strategies).
Administrative and financial support provided by Paralyzed Veterans of America.
Reprinted with permission from the Paralyzed Veterans of America (PVA) Consortium for Spinal Cord Medicine Clinical Practice Guidelines Consumer Guide: “Cardiometabolic Risk after Spinal Cord Injury: A Clinical Practice Guideline for Health Care Providers.” Washington, DC: © 2018 Paralyzed Veterans of America. Copies of the PVA's Guidelines are available at www.pva.org.
These guidelines have been prepared based on scientific and professional information available in 2018. Users should periodically review this material to ensure that the advice herein is consistent with current reasonable clinical practice. The websites noted in this document were current at the time of publication; however, because web addresses and the information contained therein change frequently the reader is encouraged to stay apprised of the most current information.
Preface
Cardiometabolic disease (CMD) can be thought of as a silent killer. The clinical manifestations of this secondary complication of spinal cord injury (SCI) may not be apparent until too late to intervene. Until now, CMD has been less of a focus of the SCI community as a whole, compared to the other major secondary conditions of neurogenic bowel and bladder, autonomic dysfunction, respiratory insufficiency, depression, sexual dysfunction, pressure injuries, and venous thromboembolism, which are overt in their presentation and have been addressed in previous guidelines.
The recommendations of this Clinical Practice Guideline (CPG) regarding identifying and managing CMD risks are in line with current recommendations for identifying and managing CMD risks in people without SCI, which have also been recently updated. However, these recommendations also take into consideration the differences between the body composition and physiology of those with SCI and those without SCI, and the risks of certain interventions for persons with SCI, given the presence of other secondary conditions such as neurogenic bowel, and also acknowledge the challenges to implementing the recommendations within the SCI community.
We were fortunate in the development and peer review of this CPG to have representation from all the various stakeholders and subspecialties impacted by these recommendations, including a range of experts in nutrition, exercise, cardiology, endocrinology, internal medicine, and rehabilitation. This wide-ranging representation will hopefully translate into uniform, quality practice through the widespread use of this CPG to guide CMD prevention and treatment in all settings, which can only result in the best outcomes and least amount of morbidity and mortality for those who experience SCI.
On behalf of the consortium steering committee, I want first to acknowledge the leadership of the guideline panel, namely the Chair, Mark Nash, and Co-Chair Suzanne Groah, in guiding this panel through the ups and downs of a development process which spanned five years. The panel members themselves, who kept to task for so long, and the many reviewers who provided valuable feedback from all areas, are to be commended. Everyone, including the panel Chair and Co-Chair, volunteered their time to help produce this superb document. In addition, I wish to acknowledge the ongoing support of Paralyzed Veterans of America (Paralyzed Veterans), especially President David Zurfluh, Executive Director Carl Blake, and Director of Research and Education Cheryl Vines, as well as the rest of the leadership team, without whose support these guidelines would not exist.
Thomas N. Bryce, MD
Chair, Steering Committee
Consortium for Spinal Cord Medicine
Foreword
The following Guideline is the first from the Consortium for Spinal Cord Medicine to address CMD after SCI. In doing so, it reports the emergence of all-cause cardiovascular diseases (CVD) and CVD-related risks as significant health hazards for persons with SCI and establishes a foundational standard for identification and management of cardiometabolic risks. The spinal cord community was first made aware of these risks in the early 1980s. Since then, hundreds of scholarly articles have examined antecedents, causes, personal and population characteristics, co-morbidities and treatments for these hazards. These studies have confirmed that persons with SCI are frequently sedentary, overweight, dyslipidemic and at elevated risk for insulin resistance, thus placing them in jeopardy of developing CMD. None of the health hazards imposed by the five archetypical CMD risk components foretells the long, active, productive, and healthy life we seek for persons with SCI. These conditions may also prohibit persons with SCI from undergoing, or ultimately benefiting from, the restorative therapies in clinical trials, or from using rehabilitation technologies that require a relatively lean and healthy body for their efficient use.
Unlike some diseases and disorders addressed by other Consortium Guidelines, CMD typically develops slowly and without overt symptoms. Unless routinely surveilled in the SCI population, CMD may be irreversible once clinically detected. The panel seriously considered the possibility that CMD and its component risks, once identified, will be far more challenging to treat in persons with SCI than their non-disabled counterparts. For these reasons, this guideline will favor scheduled surveillance, early risk assessment, timely symptom recognition, and prudent interventional care. In arriving at these recommendations, the Panel asserts that an enlightened and compassionate health care system, and a caring society, will unquestionably favor early assessment and aggressive preemptive care when not doing so might result in early morbidity and uncertain mortality.
The consumers of this guideline – health professionals and stakeholders with SCI– will note that its evidence and opinions may sometimes point to persons with SCI being at no greater risk for a diagnosis of CMD or its component risks than their non-disabled cohorts. It should be emphasized, however, that all-cause CVD and related conditions are among the most prevalent, life threatening, function compromising and costly of known medical hazards. In making recommendations, the Panel has also taken into consideration that our health care system is even less prepared to effectively treat CMD in those with SCI than to prevent it. Given these circumstances, we believe it is practical to embrace primary prevention as a best-practice, strategic approach. In some instances, the Panel found no evidence or clinical intuition to sidestep the adoption of several recommendations that currently exist for CMD diagnosis and management in the general population. These strategic guidelines provide an extensively vetted, evidence-based standard in cases where no such guideposts have been fashioned or applied for the benefit of the SCI population. When adopting standards used for the general population, we have also identified areas in need of investigation so that the foundational evidence for CMD identification and management can become even more representative of, and relevant for, the SCI population.
In publishing the Guideline, we extend our sincerest thanks for the dedicated work and meaningful contributions of Panel Members, Drs. Trevor Dyson-Hudson, David Gater, Jesse Lieberman, Jonathan Myers, Sunil Sabharwal and Allen Taylor. We further note with appreciation the contributions of Ms. Cheryl Vines, Dr. Thomas Bryce, the Paralyzed Veterans CPG Steering Committee, and the Consortium Partners who collectively recognized the importance of this topic and unfailingly supported the Panel's activities to their completion.
Mark S. Nash, PhD, FACSM, Panel Chair
Leonard M. Miller School of Medicine,
The University of Miami
Miami, FL
Suzanne L. Groah, MD, MPH, Panel Co-Chair
Medstar National Rehabilitation Hospital
Georgetown University Medical Center
Washington, DC
Summary of Recommendations
The overall objective of this guideline is to improve the care of patients with spinal cord injury by guiding clinicians and policymakers with its recommendations. The following recommendations use available evidence and – where evidence is limited – Panel experience and consensus. The Panel based its evidence ratings primarily on research in which the focus of the study was SCI. This information was supplemented using evidence from trials, guidelines, and expert opinions contained in the scientific literature of non-SCI populations.
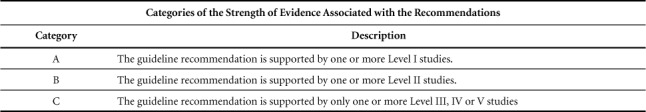
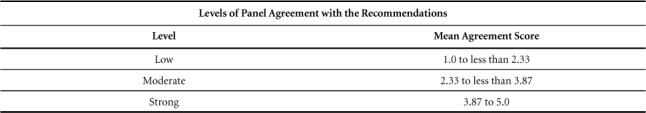
For individual patients, decisions are best made by considering these recommendations combined with clinical judgment, the latter based on specific knowledge about each patient's risk factors for cardiometabolic disease, the potential for adverse effects, and the availability of various options within one's center. The bracketed rating refers to the level of scientific evidence, the strength of the evidence, and the level of panel agreement with the recommendations.1
Summary of CMD and Component Risks Accompanying SCI
CMD
Recommendations:
-
Use the American Heart Association (AHA) definition, and the five constituent hazards of obesity, insulin resistance, dyslipidemia (including individual risks of low high-density lipoprotein cholesterol (HDL-C) and elevated Triglycerides (TG), and hypertension as CMD risk components for persons with SCI.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Evaluate all adults with SCI for CMD at the time of discharge from rehabilitation. For those already discharged from rehabilitation, evaluate at the earliest opportunity.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Obesity
Recommendations:
- Assess obesity beginning at the time of discharge from rehabilitation:
- Where possible, measure body composition using 3- or 4-compartment models to report obesity in adults with SCI until validated, clinically appropriate equations become available. Classify adult men with >22%BF and adult women with >35%BF as obese, and at high risk for CMD.
-
A BMI ≥22 kg/m2 is the cutoff point when used as a surrogate marker for obesity in persons with SCI. Adult men and women with BMI ≥22 kg/m2 are at high risk for CMD.(Scientific evidence: III; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Test at least every three years following initial assessment when tests are normal in asymptomatic adults with SCI.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation:Strong)
Impaired Fasting Glucose, Pre-Diabetes, and Diabetes
Recommendations:
-
Screen adults with SCI for diabetes and pre-diabetes, and repeat testing at least every three years if tests are normal.
(Scientific evidence: IV; Grade of recommendation: C: Level of Panel Recommendation: Strong)
-
Adopt American Diabetes Association (ADA) guidelines to diagnose diabetes and pre-diabetes based on either fasting plasma glucose (FPG), the 2-hour plasma glucose (2-h PG) value after a 75-g OGTT, or A1C criteria.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Hypertension
Recommendations:
-
Adopt AHA guidelines as the primary methods of assessment for BP measurement in persons with SCI. Measure blood pressure at every routine visit – and at least annually. Confirm elevated BP readings on a separate patient visit to diagnose hypertension.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Account for the unique challenges in making a diagnosis of hypertension in individuals with SCI, including postural influences and blood pressure variability due to autonomic instability.
(Scientific evidence: III; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Dyslipidemia
Recommendations:
-
Surveil asymptomatic adults with SCI for fasting LDL (estimated using the Friedewald equation105 when fasting TG levels are <200mg/dL, or, by direct measurement when higher), TC, TG, and HDL-C at least every three years when tests are first normal.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Perform annual screening of persons with SCI in the presence of multiple risk factors, or when evidence of dyslipidemia is confirmed or treatment initiated.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Summary of Management of CMD Risk Components after SCI
Lifestyle Intervention
Nutrition
Recommendations:
-
Conduct caloric assessment using indirect calorimetry to estimate energy expenditure and assess energy needs.
(Scientific evidence: III; Grade of recommendation: C; Level of Panel Recommendation: Strong)
- Institute the following nutritional measures after the post-acute period:
- For all individuals, adopt a heart-healthy nutrition plan focusing on fruits, vegetables, whole grains, low-fat dairy, poultry, fish, legumes, non-tropical vegetable oils and nuts, while limiting sweets and sugar-sweetened beverages, and red meats.
- Adopt the Dietary Approach to Stopping Hypertension (DASH) nutritional plan or Mediterranean nutritional plan if hypertension or additional cardiometabolic risk factors are present.
- Limit saturated fat to 5–6% of total caloric intake.
-
Limit daily sodium intake to ≤ 2400 mg for individuals with hypertension.(Scientific evidence IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Physical Activity
Recommendation:
-
Individuals with SCI should participate in at least 150 minutes of physical exercise per week, according to their ability, beginning as soon as possible following acute spinal cord injury. The 150-minutes-per-week guideline can be satisfied by sessions of 30–60 minutes performed 3–5 days per week, or by exercising for at least three, 10-minute sessions per day. When individuals with SCI are not able to meet these guidelines, they should engage in regular physical activity according to their abilities and should avoid inactivity. They should consult their health-care provider about the amount and types of physical activity that are appropriate for their abilities.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Pharmacotherapy and Surgery for Cardiometabolic Risk
Pharmacotherapy for Obesity
Recommendations:
-
Do not use prescription medications, nutraceuticals, and herbals for the management of obesity in persons with SCI.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Warn healthcare professionals and stakeholders with SCI about unsupervised use of over-the-counter and herbal anorexigenics, diuretics, and nutrient-uptake inhibitors for body fat or mass reduction.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Pharmacotherapy for Dysglycemia, Type-2 Pre-Diabetes, and Type-2 Diabetes
Recommendations:
-
Use a threshold of risk for HbA1c levels greater than 7%, as a criterion to emphasize lifestyle intervention.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
- The selection of an anti-hyperglycemic agent (or agents) should conform to the most recent treatment guidelines when glycemic targets are not met through lifestyle intervention
- Metformin is the primary agent for treatment of HbA1c >7% unless contraindicated or poorly tolerated. If the maximum tolerated dosage of metformin fails to achieve treatment goals, the addition of a second – and possibly a third agent – should conform to the most recent treatment guidelines.
- Use caution when using multi-therapy approaches, which are more likely to precipitate hypoglycemia. Consider patient-specific characteristics where drug selection may invoke hypoglycemia, resting and postural hypotension, lymphedema, heart failure, and urinary tract infections.
-
Consider referral to an endocrinologist.(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Pharmacotherapy for Dyslipidemia
Recommendations:
-
Exercise caution in the use of integrated cardiovascular risk equations for the selection of SCI patients for treatment with lipid-lowering therapies, due to the lack of calibration in SCI and the potential under-recognition of cardiovascular risk.
(Scientific evidence: III; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Guide patient selection for pharmacotherapy by other factors commonly seen in SCI, such as low levels of HDL-C and high levels of C-reactive protein. Initiate statin monotherapy using at least a moderate-intensity statin (e.g., rosuvastatin 10–20 mg/day).
(Scientific evidence: III; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Pharmacotherapy for Hypertension
Recommendations:
-
Apply evidence-based guidelines for treating hypertension in the general population of individuals with SCI. For most adults, a threshold for initiating pharmacological treatment and treatment target of 140/90 mm Hg is reasonable, although consider different targets in certain individuals and sub-populations.
(Scientific evidence- IV; Grade of recommendation- C; Level of Panel Recommendation: Strong)
-
Consider SCI-related factors when selecting an antihypertensive agent, such as the effect of thiazide diuretics on bladder management.
(Scientific evidence- IV; Grade of recommendation- C; Level of Panel Recommendation: Strong)
Bariatric Surgery for CMD Risk
Recommendations:
-
Consider bariatric surgery as a last resort for persons with morbid obesity and spinal cord injury, due to the significant peri- and postoperative risks. If bariatric surgery is considered, an SCI specialist should provide preoperative, perioperative, and postoperative consultative services to the surgical and anesthesia teams to alert them to unique risks associated with SCI.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
The Consortium of Spinal Cord Medicine
The Consortium of Spinal Cord Medicine is a collaboration of professional and consumer organizations with a common interest in healthcare for individuals living with spinal cord injury. The Consortium's mission is to direct the development and dissemination of evidence-based clinical practice guidelines (CPGs) and companion consumer guides. This mission is solely directed to improving the health care and quality of life for persons with SCI.
The Consortium is funded and administered by Paralyzed Veterans of America (Paralyzed Veterans). The Steering Committee, administratively supported by Paralyzed Veterans's Research and Education Department, is made up of one representative from each consortium-member organization.
Summary of Guidelines Development Process
The development of these guidelines involved the following major steps: creating a list of formal, key questions to be addressed, systematic searches of published literature related to these questions, critical appraisal of the quality of the retrieved studies, abstraction of relevant study results, creation of evidence-based recommendations, development of rationale that explain the recommendations, and review and agreement by panel members. The SCI Consortium's CPG development process also involved extensive field review and a legal review.
Funding and Potential Conflicts of Interest
Paralyzed Veterans contracted the literature searches and evidence reviews to an independent firm and provided administrative support for the process. Panel members received no compensation for their participation and declared all potential financial or other conflicts of interest.
Summary of Methods for CMD Diagnosis and CMD Risk Determination after SCI
Literature Search
A medical librarian searched Ovid MEDLINE® (1980 through September, Week 2 2015), the Cochrane Central Register of Controlled Trials® (1980 through September 22, 2015), Cochrane Health Technology Assessments (searched September 22, 2015), and the Cochrane Database of Systematic Reviews® (2005 through September 2015) using search terms related to chronic spinal cord injury. We also searched Ovid MEDLINE for names of authors known to have published in this area (on September 22, 2015). See the Appendix for complete search strategies. We attempted to identify additional studies through hand searches of reference lists of included studies and reviews. All citations were imported into an electronic database (Endnote® X7, Thomson Reuters).
Study Selection
Selection of included studies was based on the inclusion criteria created in consultation with Paralyzed Veterans. Two reviewers independently assessed titles and abstracts of citations identified through literature searches for inclusion, using the criteria below. Full-text articles of potentially relevant citations were retrieved and were assessed for inclusion by both reviewers. Disagreements were resolved by consensus. Results published only in abstract form were not included because inadequate details were available for quality assessment (risk of bias). Abstracts that had additional information available in slide sets from conference presentations, or those that provided supplemental data from published studies, were considered for inclusion.
Inclusion Criteria
In consultation with Paralyzed Veterans, 14 key questions were formulated relating to the prevalence of CMD and risk factors for disease, screening for CMD, CMD diagnosis methods, and the comparative effectiveness of treatment for CMD in the SCI population. Key questions 13 and 14 regarding CMD guidelines were not part of the systematic review, but they provide information on relevant guideline recommendations. Key questions and inclusion criteria are below.
Key Questions
Prevalence
What is the prevalence of individual CMD risk factors (e.g., obesity, glucose dysregulation, hypertension, dyslipidemia) in the SCI population?
What is the prevalence of CMD (defined as the presence of three or more risk factors) in the SCI population?
What is the prevalence of diabetes and cardiovascular disease in the SCI population?
What are the mortality rates from diabetes and cardiovascular disease in the SCI population?
What are the associations between CMD risk factors – alone or in clusters – and the development of diabetes and/or cardiovascular disease in the SCI population?
Screening
What is the evidence that screening for risk factors for diabetes and cardiovascular disease among asymptomatic adults with SCI improves health outcomes (e.g., myocardial infarction, amputation, mortality, quality of life)?
Which risk-factor screening methods or cutoffs are most effective in improving health outcomes in the SCI population?
Are there subgroups within the SCI population, based on demographic characteristics (e.g., age, gender, ethnicity, socioeconomic status, comorbidities [to include patients with known diabetes or known cardiovascular disease], medications, degree or level of paralysis, etiology of paralysis), for which screening for CMD risk factors are more or less effective in improving health outcomes?
Diagnosis
What is the diagnostic accuracy in the SCI population of fasting blood glucose or the glucose tolerance test for current diabetes, defined as having an HbA1c > 6.5 percent?
What is the diagnostic accuracy of CMD risk factors for current heart disease in the SCI population?
Treatment
What is the evidence that interventions to improve CMD risk factors – alone or in clusters – improves health outcomes in the SCI population?
Are there subgroups within the SCI population, based on demographic characteristics (e.g., age, gender, ethnicity, socioeconomic status, comorbidities [to include patients with known diabetes or known cardiovascular disease], medications, degree or level of paralysis, etiology of paralysis), for which interventions to improve CMD risk factors are more or less effective in improving health outcomes?
Guidelines
What are the existing CMD guidelines, or sections of guidelines, focusing on the SCI population?
What are the recommendations from major guideline groups for screening and interventions for CMD risk factors in patients without paralysis?
PICOTS
Population
Patients with nonacute, traumatic, or atraumatic irreversible spinal cord injury or dysfunction resulting in paralysis (excluding patients with spinal stroke)
Interventions
- Screening
- ○ Obesity
- ○ Glucose dysregulation
- ○ Hypertension
- ○ Dyslipidemia (e.g., low HDL, high TG)
- ○ Markers of inflammation (i.e., CRP, IL6, TNF-α)
- Treatment
- ○ Lifestyle modification
- ▪ Diet
- ▪ Exercise (i.e., active exercise and electrical stimulation)
- ▪ Stress reduction
- ▪ Education and counseling
- ○ Medication
Comparators
Adults without SCI
Another included intervention (head-to-head study in SCI population)
Placebo
Usual care
Outcomes
Myocardial Infarction
Stroke
Amputation
Blindness
Chronic renal disease, including renal transplant)
Peripheral vascular disease
Pulmonary embolism or deep vein thrombosis
Quality of life
Timing
Chronic paralysis (paralysis of at least one year)
Setting
Outpatient
Study Designs
KQ 1–3: epidemiological database studies
KQ 4: epidemiological database studies, case-control studies
KQ 5–7: randomized trials, nonrandomized comparative studies (cohort, case-control)
KQ 8–9: diagnostic accuracy studies where all participants received the gold standard
KQ 10–11: randomized trials, nonrandomized comparative studies, case series
KQ 12–13: guidelines
Data Abstraction
Information was abstracted on population characteristics, interventions, subject enrollment, prevalence, results for efficacy, effectiveness, and harms outcomes for trials, observational studies, and systematic reviews. When reported, intent-to-treat results were recorded. Data abstraction was performed by one reviewer and independently checked by a second reviewer. Differences were resolved by consensus.
Validity Assessment (Risk of Bias)
We assessed the internal validity (risk of bias) of trials, observational studies, and systematic reviews based on predefined criteria. These criteria are based on the U.S. Preventive Services Task Force and the National Health Service Centre for Reviews and Dissemination (United Kingdom) criteria7–8 and the GRADE guidelines.9 We rated the internal validity of each trial based on the methods used for randomization, allocation concealment, blinding, the similarity of compared groups at baseline, loss to follow-up, and the use of intent-to-treat analysis. Trials that had a fatal flaw were rated at a high risk of bias, trials that met all criteria were rated at a low risk of bias, and the remainder were rated at a moderate risk of bias. As the moderate risk of bias category is broad, studies with this rating vary in their strengths and weaknesses. The results of some studies rated moderate risk of bias are likely to be valid, while others are only possibly valid. A fatal flaw is reflected by failure to meet combinations of items on the risk-of-bias checklist. An example would be a study with high attrition (e.g., 60%) combined with the inadequate handling of missing data, or one where details on randomization and/or allocation concealment were lacking, and there were baseline differences in important prognostic characteristics. Observational studies were rated on non-biased selection, loss to follow-up, pre- specification of outcomes, well-described and adequate ascertainment techniques, statistical analysis of potential confounders, and adequate duration of follow-up. Systematic reviews were rated on the clarity of review questions, the specification of inclusion and exclusion criteria, use of multiple databases and search for grey literature, sufficient detail of included studies, adequate assessment of the risk of bias of included studies, and adequate summarization of primary studies.
Two reviewers independently assessed the quality of each study and differences were resolved by consensus.
Grading the Quality of Evidence
We graded quality of evidence (QoE) based on the GRADE approach.10–14 Developed to grade the overall quality of a body of evidence, this approach incorporates four key domains: risk of bias (includes study design and aggregate risk of bias), consistency, directness, and precision of the evidence. It also considers other optional domains that may be relevant for some scenarios, such as a dose- response association, plausible confounding that would decrease the observed effect, the strength of association (magnitude of effect), and publication bias.
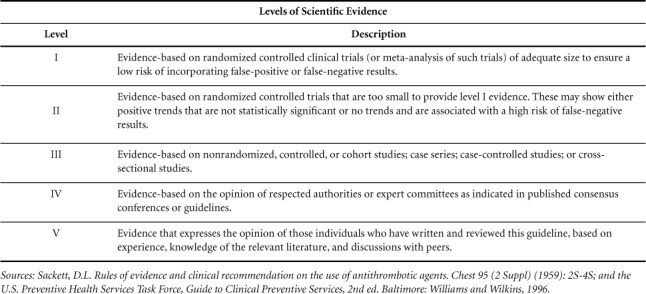
Table 1 describes the grades of evidence that can be assigned. Grades reflect the quality of the body of evidence to answer key questions. Grades do not refer to the general efficacy or effectiveness of treatments, for example. Two reviewers independently assessed each domain for each outcome and differences were resolved by consensus.
Table 1.
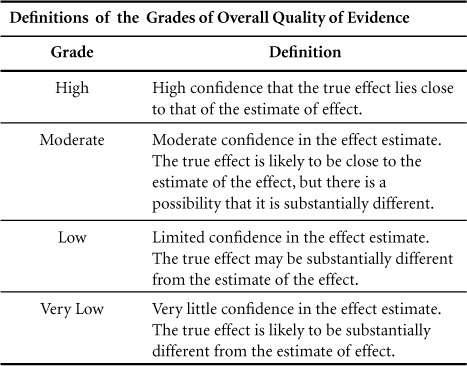
The quality of the body of evidence was evaluated for each outcome by key question.
Data Synthesis
We constructed evidence tables showing the study characteristics, quality ratings, and results for all included studies. We reviewed studies using a hierarchy of evidence approach, where the best evidence is the focus of our synthesis for each question, population, intervention, and outcome addressed.
CMD: Definition and Risks Accompanying SCI
Section Preamble
The following section addresses hazards for CMD and its risk components in persons with SCI.
Panel Findings
People with SCI have the same or greater degree of risk for CMD as the non-disabled population.
Specific factors may elevate CMD risk, including veteran status, age at onset of SCI, duration of injury, pre-injury health status, family medical history, ethnicity, and heritage.
The AHA's constituent CMD hazards of obesity, impaired fasting glucose, hypertension, and dyslipidemia (low HDL-C and elevated TG) are all considered risk components for CMD in persons with SCI.
Risks of a sedentary lifestyle, excessive caloric and fat intake respective to energy needs, and elevated blood-borne inflammatory biomarkers may be considered as SCI-specific supplementary risks for CMD.
Rationale
CMD is a coalescing of interrelated cardiovascular, renal,metabolic,pro-thrombotic,andinflammatory health hazards,1 and is recognized as a disease entity by the American Society of Endocrinology, the AHA, the International Diabetes Federation (IDF), the American Diabetes Association (ADA), and the World Health Organization (WHO).2 The AHA and the National Institutes of Health (NIH) National Heart Lung Blood Institute (NHLBI) define CMD as the co-occurrence of any three of the medical hazards described in Table 2.
Table 2.
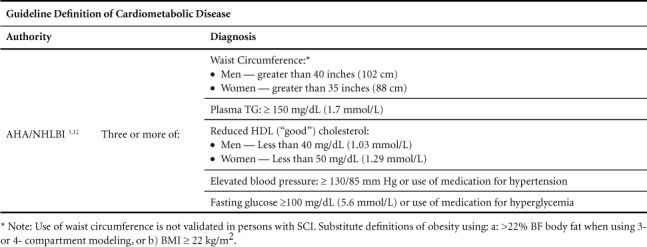
Abdominal (central) obesity, hypertension, hyperglycemia, hypertriglyceridemia, and low high-density lipoproteinemia.3 While still lacking a fully harmonized diagnosis,2 CMD is recognized to increase the probability of developing atherosclerotic disease, heart failure, and diabetes.4–5 Prevalence in the U.S. is estimated at 34% of the non-disabled adult population6 and is increasing with population aging. The CMD diagnosis confers a health risk equivalent to either the diagnosis of diabetes mellitus or extant coronary disease.
CMD is ultimately caused or worsened by a mismatch between energy consumption that is excessive in intake of kilocalories and saturated fats, and insufficient daily energy expenditure.7 These risks are typically expressed through lifestyle factors reflecting poor compliance with optimal nutrition and an active lifestyle. The primary metabolic abnormality of CMD is insulin resistance, while the unified cause ensues excessive body mass, whose clinical feature is excessive visceral and ectopic fat. Inflammatory stress and endocrinopathies are not included among the AHA guideline risks, although both are recognized as either cause or consequence of the disorder. 8–9
Figure 1.
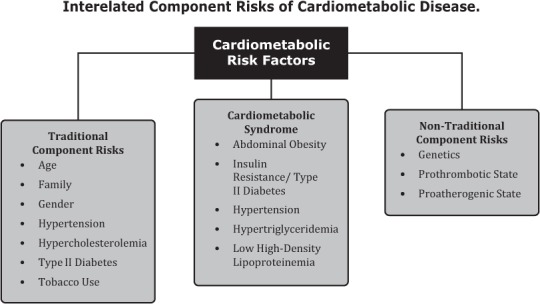
The prevalence of CMD reported in adults with SCI ranges from 31–72%, contingent on the number of possible risk factors included in the definition.10–11 Depending on the study, this prevalence at least equals, and often exceeds, the CMD prevalence for the general population, which the Panel feels informs the SCI community about the risk that it poses.
CMD Component Risks Accompanying SCI
Section Preamble
The guideline component risks for CMD include obesity, insulin resistance, dyslipidemia, and hypertension. The following section addresses the hazards imposed by these individual risk components on the SCI population.
Obesity
Panel Findings
Obesity (i.e., excessive adiposity) is a major risk component for CMD after SCI.
Obesity after SCI is associated with risks of insulin resistance, diabetes, dyslipidemia, and hypertension.
Obesity in persons with SCI is grossly underestimated when using both the surrogate marker of Body Mass Index (BMI) and criterion scores for obesity typically used for the general population.
Guidelines that identify the conditions of overweight and obesity in non-disabled persons have limited application in diagnosing obesity in persons with SCI.
Rationale
“Obesity is a chronic, relapsing, neurochemical disease produced by the interaction of environment and host.”13 Emerging data suggests adipose tissue (especially visceral adiposity) and its associated connective tissue are the primary sources of systemic proinflammatory cytokines, vasoactive hormones and non-esterified fatty acids implicated in the development of dyslipidemia, insulin resistance, hypertension, and arteriosclerosis. Initially defined by the scientific community as >22% body fat (%BF) in men or >35%BF in women, the definition of obesity was changed to BMI ≥30 kg/m2 by the WHO at the turn of the century to more easily capture large populations at risk for cardiovascular disease.14
Of the five AHA component risks, obesity after SCI has been most challenging to characterize and compare to non-SCI populations. BMI grossly underestimates obesity (overfat) in persons with SCI due to profound changes in fat-free mass (FFM), reflecting obligatory sarcopenia, osteopenia and reduced total body water associated with somatic and autonomic disruption of the spinal cord. The standard cutoff for BMI of >30 kg/m2 grossly underestimates adiposity in persons with SCI, such that the true prevalence of CMD exceeds the 31–72% prevalence of CMD in persons with SCI reported in the literature.11,15–16 Multiple studies have reported a BMI of 22–25 kg/m2 in persons with SCI translates to >30% BF,17–24 which is well above the standard cut-score for obesity of 22% BF in the non-SCI population. One study recalculated CMD prevalence with SCI-specific cutoff BMI≥22 kg/m2 and found that doing so increased the range from 27–36% to 82–85% prevalence.16
For accurate obesity comparisons between persons with SCI and those without, BMI cutoffs for obesity of 22 kg/m2 and 30 kg/m2, respectively, should be used. Another option to determine overweight and obesity risk is waist circumference. However, the use of this proxy has not been validated in SCI populations and is likely inadequate as a surrogate obesity marker due to varying levels and neurological completeness of abdominal muscle paralysis.25
Insulin Resistance
Panel Findings
The risk of insulin resistance, diabetes, or CMD in persons following SCI is at least as great as for persons without SCI.
Race, ethnicity, veteran status, and family history may increase the risk of insulin resistance, diabetes, or CMD.
Rationale
The prevalence of diabetes in people with SCI varies with the attributes of the population being studied. Prevalence studies for diabetes in people with SCI in the U. S. have primariiily focused on U.S. veterans, so findings may not be generalizable to other populations.26–28 U.S. studies report a higher prevalence of diabetes in people with SCI (16% to 33%) than those conducted in other countries (6% to 14%).29–32 Evidence indicates that the prevalence of diabetes among U.S. veterans with SCI is not different from veterans without SCI.26–27 However, moderate quality evidence from other countries indicates that persons with SCI have a higher prevalence of diabetes than able-bodied controls.29–32 Traditional risk factors for diabetes and glucose intolerance in the general population, such as increasing age, at-risk race or ethnicity (Asian, African American, Hispanic, Native American, or Pacific Islander), and family history of diabetes,33 likely apply to the SCI population as well, though evidence specific to SCI is limited and of low quality.
Dyslipidemia
Panel Findings
The prevalence of dyslipidemia among persons with SCI is high when based on established cholesterol guidelines and when compared to non-disabled individuals.
The most consistent component of dyslipidemia risk among persons with SCI, when compared to non-disabled individuals, is depressed levels of HDL-C.
Rationale
The prevalence of dyslipidemia among persons with SCI is high when based on established cholesterol guidelines as well as comparisons to non-disabled individuals. Studies on lipid profiles reflecting higher cardiovascular risk among persons with SCI, compared to non-disabled individuals, have included the spectrum of lipid subfractions, including HDL-C, LDL-C, ratios of total cholesterol to HDL-C and LDL-C, and HDL/Apo-1 and Apo-A1/ApoB.34–41 All these findings support the Panel's recommendations. The most consistent observation from studies assessing lipid profiles of persons with SCI is depressed HDL-C levels when compared to non-disabled individuals.15,38,39,42–44 However, many of these studies lack specifics regarding which lipid abnormalities are observed, and their potential association with the level and extent of the injury and other population characteristics. This disparity has led to variation in results between studies comparing cohorts of persons with SCI versus non-disabled controls. For example, in a large study comparing U.S. Veterans 65 years and older with subjects having SCI, ambulatory older Veterans, and ambulatory control subjects, no differences were observed in the prevalence of dyslipidemia (44%, 48, and 44%, respectively).27 Conversely, in a Swedish cohort, the prevalence of dyslipidemia was markedly higher in persons with SCI than non-disabled controls (11% vs. 2%, p<0.001).29 Studies have generally reported somewhat lower total cholesterol and HDL-C levels, but higher TG and a higher ratio of total cholesterol to HDL-C among SCI individuals compared with matched groups of non-SCI subjects.34–39,43 Importantly, the overall prevalence of dyslipidemia in the general US population also tends to be high, and some research has questioned whether the prevalence of dyslipidemia is appreciably higher in persons with SCI (e.g., ≈50% of Americans have some form of lipid abnormality).45 There is a lack of consistent data regarding the effects of level of injury as well as other clinical and demographic factors on the prevalence of dyslipidemia in persons with SCI.
Hypertension
Panel Findings
The prevalence of hypertension in people with SCI varies with the attributes of the population being studied, including injury level, severity, and etiology.
Rationale
The reported prevalence of hypertension in people with SCI varies widely, ranging from 14% to 61%.27,31,46–50 Age, gender, ethnicity, nationality, and other attributes of the population being studied may affect the reported prevalence, as may differences in methods to ascertain the presence of hypertension. Studies on the prevalence of hypertension in SCI in the United States27,46–49 have mostly been conducted in U.S. veterans; findings may not be generalizable to other populations.
Injury to the spinal cord influences the regulation of blood pressure. Characteristics of the SCI, including neurological level and etiology of injury, may affect the prevalence of hypertension. Prevalence of hypertension is reported to be lower in people with tetraplegia compared with paraplegia, especially those with low paraplegia (T7 and below).46–47,50 The odds of having hypertension were significantly lower in tetraplegic injuries, compared to matched controls without SCI in a study of U.S. veterans, while paraplegic injuries had similar odds of hypertension as controls. Veterans with non-traumatic SCI had higher odds of having hypertension compared with those with traumatic SCI after controlling for available SCI characteristics, age, demographics, and comorbidities.46
Supplementary CMD Risks Accompanying SCI
Section Preamble
The following section addresses the supplementary hazards associated with SCI that are population risk-relevant but not included among the AHA risk component hazards of CMD.
Physical Deconditioning
Panel Findings
Individuals with SCI become physically deconditioned after injury.
Physical deconditioning contributes to CMD and its risk determinants in persons with SCI.
Rationale
Exercise is a fundamental element in maintaining physical capacity and cardiovascular and metabolic health for persons of all ages and health states. The unified American College of Sports Medicine (ACSM) and WHO guidelines51 prescribe exercise and provide physical activity guidelines for supporting health and wellness in the general population, which to the best of their abilities are also recommended for individuals with SCI.52 These guidelines are in substantial agreement with both the ACSM Guidelines for Exercise Testing and Prescription51 and also the Physical Activity Guidelines for Adults with SCI that were established for SCI Action Canada.53 They are also similar to the Physical Fitness for Special Populations (PFSP) “Physical Fitness for Individuals with Spinal Cord Injury” recommendations of the American Physical Therapy Association.54
A sedentary lifestyle either imposed on or adopted by persons with SCI has long identified physical inactivity as a population health risk.55 Notwithstanding a single identified cause for a sedentary lifestyle, a 1993 study reported that 1 in 4 healthy, young persons with SCI fail to satisfy a level of fitness needed to perform many essential activities of daily living.56 More recently, it was reported that approximately 50% of patients with SCI report no leisure-time physical activity and 15% report leisure-time physical activity below the threshold required for meaningful health benefit (i.e., <1 hour/week).57 This report implies that of the estimated 558,000 individuals currently living with SCI in the U.S., approximately 279,000 are completely sedentary and another 84,000 participate in a leisure-time physical activity considered inadequate to positively impact health.58 While those with sensorimotor sparing of upper limb and trunk functions (i.e., paraplegia) have far greater capacities for physical activity and more extensive exercise options,59 they are not necessarily more fit than persons with tetraplegia.55,60
While physical deconditioning per se is not included among the five component risks of CMD, it is linked with and considered a major cause of obesity, insulin resistance, hypertension, and dyslipidemia. Several factors, however, point to physical deconditioning after SCI as a major contributor to a CMD diagnosis. First, the SCI population was long ago identified at the lowest end of the human fitness continuum, making physical deconditioning suspect as a cause for CMD-related risks.55,61–63 Second, a common finding after SCI is a low concentration of HDL-C,36,40–41,64 which is known in persons without disability to be both cardioprotective and strongly linked with low levels of cardiorespiratory fitness.65–67 Third, barriers to exercise participation are altogether common after SCI and may include self-imposed obstacles to exercise participation or legitimate physical barriers to exercise, lack of adapted exercise equipment, limited professional assistance, societal moirés, and financial limitations.68–72
Nutrition
Panel Findings
Those with SCI who are beyond the post-acute period, especially individuals with higher level and severity of SCI, require fewer calories after SCI to maintain a stable body mass and composition than before the injury
Rationale
Following an acute SCI, body composition is altered by a significant loss of sublesional skeletal muscle, an increase in visceral fat mass,1–4 and an injury-dependent decrease in sympathetic nervous system activity.5 As a result, persons with SCI have decreased energy expenditure relative to energy intake, and when compared to individuals without SCI.6–8 Subsequently, central (i.e., visceral) adiposity is common among persons with chronic SCI and is more prevalent than in persons without SCI. Importantly, the greatest increase in weight often occurs during the first year after injury.9–15
While physical activity has established benefits as a countermeasure to excessive caloric intake, some persons with SCI cannot substantially increase energy expenditure with physical activity alone. Some are limited by their level of injury17 and overuse injuries18–20 as well as other documented barriers to exercise.21–24 Based on the existing evidence, and appreciating that caloric expenditure from activity rarely compensates for excessive caloric intake, dietary changes appear to be a more practical target for obesity management and CMD prevention in individuals with SCI.
Inflammation
Panel Findings
CRP and other inflammatory biomarkers represent a unique subclinical risk component of CMD for the SCI population.
The role of CRP and other inflammatory biomarkers in risk identification, development, and diagnosis of CMD and CMD risk components for the SCI population requires further exploration.
Rationale
Numerous markers of inflammation have been associated with cardiovascular disease (CVD) risk in non-disabled populations.73 For example, in a study of nearly 28,000 post-menopausal women, high-sensitivity C-reactive protein (hs-CRP) was reported to be the strongest predictor of risk for cardiac events.74 However, the relationship between inflammatory markers and CVD risk in SCI is complicated by the fact that these markers may be elevated due to higher fat mass, higher prevalence of urinary tract infections, pressure ulcers, and other factors inherent to SCI. Although inflammation has been shown to be elevated in persons with chronic SCI (even in the absence of acute infection), their relationship to CVD risk specifically in persons with SCI is not as clear as that in individuals without SCI.34,75
Studies comparing levels of inflammation between persons with SCI and age-matched non-disabled subjects have enrolled relatively small sample sizes, but they demonstrate a higher systemic inflammatory state when compared to non-disabled subjects. Liang and colleagues15 studied 129 men from the National Health and Nutrition Examination Survey (NHANES) with SCI who were free of infection, matching them by age and race to a group of non-disabled subjects. SCI subjects were more likely to have elevated CRP (odds ratio 2.29), and CRP was higher in complete versus incomplete injury (median 3.7 mg/L vs. 1.2 mg/L, p=0.005). The elevation in CRP was independent of age, smoking, physical activity, waist circumference, and weight, but was associated with low HDL. Lee and colleagues76 examined the relationship between hs-CRP, insulin resistance, and metabolic syndrome among 93 individuals with chronic SCI. Metabolic syndrome and insulin resistance were present in nearly one-quarter of the SCI sample (22.6%). Subjects with fasting insulin resistance had significantly higher mean hsCRP (4.29±3.25 mg/L) than those who were not insulin resistant (2.24±2.02) (p<0.05). Moreover, hsCRP was significantly elevated in individuals who presented with high CVD risk including severe dyslipidemia (≥4 abnormal lipid values) and elevated Framingham Risk scores (≥6).
Although CRP is the most studied and widely recognized inflammatory marker, other proinflammatory cytokines have been evaluated in SCI. These biomarkers have important roles in the early stages of inflammation and the immunoregulatory process. Wang et al.77 compared 62 men with traumatic, complete SCI and no active infection with 29 age-matched, ambulatory control subjects. Irrespective of injury level and duration, subjects with SCI had consistently higher levels of serum CRP (4.0±2.7 vs. 1.4±1.1 mg/L) and interleukin-6 (IL-6). Also, these higher levels of inflammation were independent of dyslipidemia and insulin resistance. Frost et al.78 compared serum levels of CRP and cytokine levels between 37 subjects with chronic SCI and 10 healthy non-disabled control subjects. SCI subjects had higher levels of serum CRP but not IL-6 or tumor necrosis factor alpha (TNF-α). No associations were observed due to age or duration of injury. Davies et al.79 compared 56 SCI subjects with 35 age-matched, non-disabled controls and reported that SCI subjects exhibited serum concentrations of IL-6, TNF-α, and IL-1RA that were greater than non-disabled subjects. Elevated cytokine concentrations were not associated with high white blood cell counts, level of injury, or American Spinal Injury Association impairment classification.
CRP has been shown to be elevated in acute and chronic SCI subjects with and without urinary tract infections, suggesting that it may be more attributable to an underlying disease state rather than the SCI itself. While studies have consistently shown higher than normal CRP levels in persons with SCI, few data are available regarding the relationship between CRP and CVD risk, specifically in SCI.79 Among individuals with SCI who are insulin resistant and display components of the CMD, hsCRP is elevated, suggesting a clinically important association with CVD risk in this population. Lee et al.79 reported that CRP was significantly associated with the presence of other well-known CVD risk factors, including metabolic syndrome, insulin resistance, and elevated Framingham risk. Similarly, Gibson et al.80 reported that persons with SCI had CRP levels consistent with high CVD risk and that those with high CRP had larger waist circumference, BMI, percent fat mass, and HOMA-IR values than those with lower CRP. Epidemiological studies are lacking regarding the association between inflammation in SCI and outcomes; thus, the role of CRP and other inflammatory markers in the development of atherosclerosis and predicting future CVD events in the SCI population requires further exploration.
Methods for CMD Diagnosis, and CMD Risk Identification and Surveillance Intervals after SCI
Section Preamble
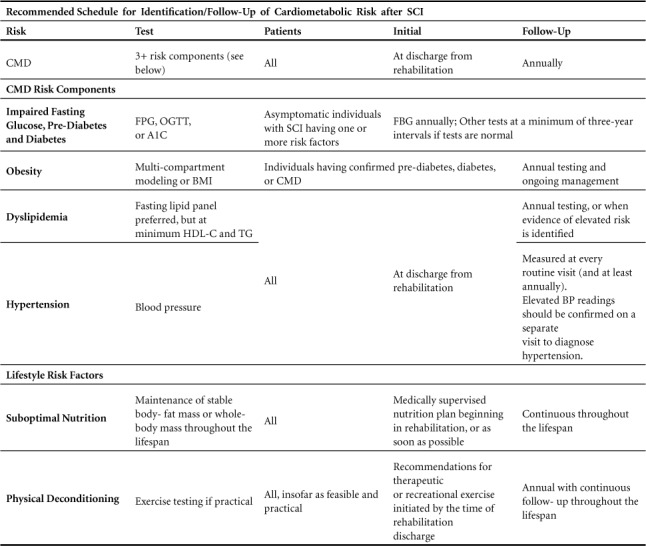
The following section provides recommendations for measurement and the criterion scores for CMD and CMD risk determination in persons with SCI. A recommended schedule for surveillance and follow-up on CMD is shown in Table 3.
Table 3.
CMD
Recommendations
-
The AHA definition should be used, and constituent hazards of obesity, insulin resistance, dyslipidemia (low HDL-C and elevated TG), and hypertension should be included as CMD risk components for persons with SCI.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Evaluate all adults with SCI for CMD at the time of discharge from rehabilitation. For those who are already discharged from rehabilitation, evaluate at the earliest opportunity.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
The recommended standard is a “sum of risks” guideline that defines CMD as three or more of the five individual risk determinants.2 Other standards are published but are not necessarily harmonized. The recommendation provides a baseline for future comparison of CMD and its risk component risks.
Obesity
Recommendations
- Assess obesity beginning at discharge from rehabilitation:
- Where possible, measure body composition using 3- or 4-compartment models to report obesity in adults with SCI, until validated, clinically appropriate equations become available. Classify adult men with >22%BF and adult women with >35%BF as obese, and at high risk for CMD.
-
A BMI ≥22 kg/m2 is the cutoff point when used as a surrogate marker for obesity in persons with SCI. Adult men and women with BMI ≥22 kg/m2 are at high risk for CMD.(Scientific evidence: III; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Repeat the testing at least every three years following initial assessment when tests are normal in asymptomatic adults with SCI.
(Scientific evidence- V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
BMI grossly underestimates obesity (overfat) in persons with SCI due to profound changes in fat-free mass (FFM), reflecting obligatory sarcopenia, osteopenia, and reduced total body water associated with somatic and autonomic disruption of the cord. Multiple studies have reported BMI of 22–25 kg/m2 in persons with SCI translates to >30%BF,81–91 well above the standard cut-score for obesity of 22%BF in the non-SCI population.
For accurate obesity comparisons between persons with SCI and those without, BMI cutoffs for obesity of 22 kg/m2 and 30 kg/m2, respectively, should be used. Unfortunately, such comparisons have not been reported. Rather, most studies have used a BMI cutoff of 25 kg/m2 to reflect “overweight or obese” in both SCI and non-SCI populations. Of eight studies that reported the prevalence of being overweight or obese in persons with SCI, i.e., BMI>25 kg/m2, a 53–60% prevalence rate was noted.15,49,92–97 Conversely, obesity rates in the general population (BMI>30 kg/m2) range between 20–27%.49,94–95,97 In the three studies that compared BMI>25 kg/m2 in persons with SCI and non-SCI controls, results were mixed, with one showing a lower prevalence in SCI,93 and the other two showing no significant difference in prevalence between SCI and controls.96,98
Impaired Fasting Glucose, Pre-Diabetes, and Diabetes
Recommendations
-
Screen adults with SCI for diabetes and prediabetes, with repeat testing at least every three years if tests are normal.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Adopt ADA guidelines to diagnose diabetes and pre-diabetes based on either FPG, the 2-hour plasma glucose (2-h PG) value after a 75-g OGTT, or A1C criteria.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
Testing for diabetes and prediabetes in asymptomatic individuals in the general population has been recommended for those with one or more risk factors and beginning at age 45 for those without additional risk factors, with repeat testing at three-year intervals at least if tests are normal.99 Lower physical activity, and changes in body composition with reduced lean muscle mass and increased percentage of body fat, may contribute to the additional risk of glucose intolerance and insulin resistance in individuals with SCI.100–101 Directly measuring insulin resistance is difficult and unstandardized, making it impractical for the clinical setting, but FPG is an acceptable indirect test. Alternatively, an OGTT or HbA1c can be used. While specific evidence for an optimal screening interval or age to start screening individuals with SCI is currently lacking, it is reasonable to consider screening in adults with SCI and to repeat testing at one- to three-year intervals if tests are normal.
Standards of Medical Care in Diabetes published by the ADA outline methods and criteria for identifying Type 2 pre-diabetes and diabetes (Table 4).99 Criteria for the diagnosis of diabetes include either FPG >126 mg/dL (7.0 mmol/L) after no caloric intake for at least 8 h, or 2-h PG >200 mg/dL (11.1 mmol/L) during an OGTT with the test performed using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved in water, or A1C >6.5% (48 mmol/mol). In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose >200 mg/dL (11.1 mmol/L) is also considered diagnostic of diabetes in the general population; however, in SCI this could be confusing since such symptoms, including polyuria, polydipsia, weight loss, and fatigue, often have other etiologies.
Table 4.
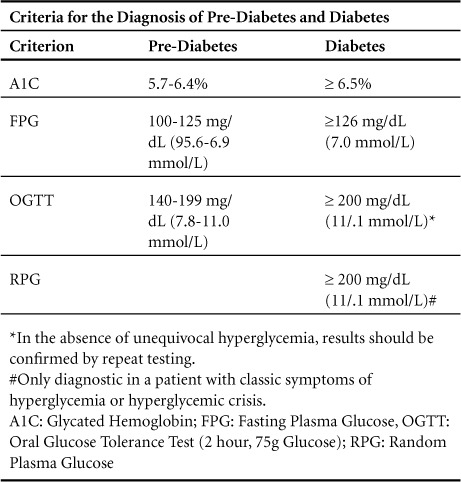
Criteria for identifying prediabetes include either FPG 100 mg/dL (5.6 mmol/L) to 125 mg/dL (6.9 mmol/L) (IFG), 2-h PG in the 75-g OGTT 140 mg/dL (7.8 mmol/L) to 199 mg/dL (11.0 mmol/L) (IGT), or A1C 5.7 to 6.4% (39 to 47 mmol/mol). For all three tests, risk is continuous, extending below the lower limit of the range and becoming disproportionately greater at the higher end of the range (Table 4).
Hypertension
Recommendations
-
Adopt AHA guidelines as the primary methods of assessment for BP measurement in persons with SCI. Measure blood pressure at every routine visit and at least annually. Confirm elevated BP readings on a separate patient visit to diagnose hypertension.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Consider unique challenges in making a diagnosis of hypertension in individuals with SCI, including postural influences and blood pressure variability due to autonomic instability.
(Scientific evidence: III; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
The AHA Scientific Statement on Recommendations for Blood Pressure Measurement in Humans102 is the most current AHA authority on BP measurement procedures, selection of devices, and device calibration. The BP goals are consistent with AHA/NHLBI Guidelines on the diagnosis of CMD.1,2
Posture may affect blood pressure in people with SCI, especially those with tetraplegia. A study of veterans with SCI reported differential orthostatic effects on systolic hypertension based on the level of injury. Prevalence of systolic blood pressure (SBP) ≥140 mmHg was lower in the supine compared to the seated position in subjects with low paraplegia, whereas the incidence of a supine SBP ≥140 mmHg was increased by 53% compared to seated in subjects with tetraplegia.48 The presence of supine hypertension may be missed in individuals with tetraplegia if only seated blood pressure is measured. Supine hypertension may be associated with lack of a nocturnal dip in blood pressure, which has been associated with cardiovascular risk in the general population.
Significant variability in blood pressure is common in people with SCI due to autonomic instability,47,103 so single blood pressure readings may be especially inaccurate to determine the presence and degree of hypertension in this population. Coexisting conditions such as autonomic dysreflexia and orthostatic hypotension may contribute to diagnostic confusion, particularly in individuals with tetraplegia. Episodic blood pressure elevation should prompt the consideration of autonomic dysreflexia in individuals with SCI at or above the T6 neurological level.104 Repeating blood pressure measurements over time and measuring blood pressure in both the supine and seated positions, with documentation of the position in which blood pressure was recorded, may improve the accuracy of diagnosing hypertension after SCI.
Dyslipidemia
Recommendations
-
Surveil asymptomatic adults with SCI for fasting LDL (estimated using the Friedewald equation105 when fasting TG levels are <200mg/dL, or, by direct measurement when higher), TC, TG, and HDL-C at least every three years when tests are first normal.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Perform annual screening of persons with SCI in the presence of multiple risk factors, or when evidence of dyslipidemia is confirmed or treatment initiated
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
A fasting lipid profile provides the most comprehensive method for detection of dyslipidemia risk. Screening guidelines for dyslipidemia in the non-disabled population vary by age, with treatment goals personalized according to risk levels. (AACE 2017 Tables 6 and 11).106 However, the decision to screen should always be based on clinical judgment. Specific indications – notably patient age, age at SCI, clinical evidence of existing disease, family history, and the presence of other co-morbid CMD risks – should alert physicians to conduct screenings. As all-cause vascular disease is reported to be accelerated after SCI, the risk for earlier CMD components risk and CMD diagnosis should be taken into consideration.7,107
The linkage of major risks for obesity and low HDL-C,108 and reports that BMI is among the strongest risk predictors for diabetes109–110, compel the attention of both obesity and insulin-resistance once presenting in persons with SCI. Moderate TG elevations (≥150 mg/dL) may identify individuals at risk for the insulin resistance and levels ≥200 mg/dL may detect individuals at substantially increased ASCVD risk, making their co-morbidity a concern once identified. Current guidelines do not consider an isolated finding of low HDL sufficient to initiate drug therapy, but at a minimum this foretells the need for diligent lifestyle intervention. 111
Moreover, recent guidelines from the AACE 106 emphasize the strong association between low HDL-C and hypertriglyceridemia, T2DM, overweight or obesity, physical inactivity, cigarette smoking, very high carbohydrate intake, and genetic factors. Low HDL-C can thus act synergistically with other lipid risk factors to increase clinical risk, making low HDL a sentinel of risk, even in the presence of low TC and very low (< 70 mg/dL) LDL-C.112
Management of CMD Risk Components after SCI
Section Preamble
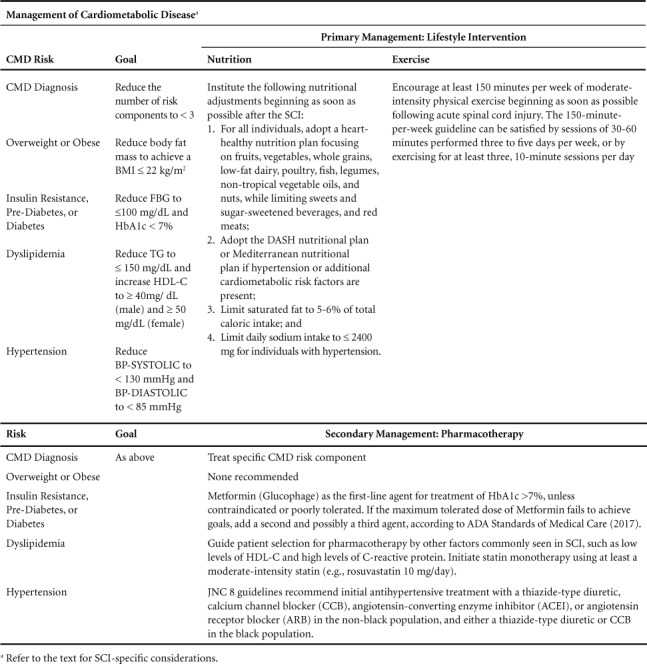
The following section will present findings and recommendations for management of CMD and CMD risk determinants through lifestyle intervention (i.e., nutrition and physical activity), pharmacotherapy, and surgery. Table 5 contains a summary of Panel recommendations.
Table 5.
LIFESTYLE INTERVENTION
Nutrition
Recommendations
-
When establishing caloric targets, all persons with SCI should undergo a caloric assessment using indirect calorimetry to estimate energy expenditure and assess energy needs.
(Scientific evidence: III; Grade of recommendation: C; Level of Panel Recommendation: Strong)
- Institute the following nutritional measures after the post-acute period:
- All individuals should adopt a heart-healthy nutrition plan focusing on fruits, vegetables, whole grains, low-fat dairy, poultry, fish, legumes, non-tropical vegetable oils, and nuts while limiting sweets, sugar-sweetened beverages, and red meats.
- Adopt the DASH nutritional plan or Mediterranean nutritional if hypertension or additional cardiometabolic risk factors are present.
- Limit saturated fat to 5–6% of total caloric intake.
-
Limit daily sodium intake to ≤ 2400 mg for individuals with hypertension.(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
Following an acute SCI, body composition is altered by a significant loss of skeletal muscle, an increase in fat mass,113–116 and in some cases a decrease in sympathetic nervous system activity.117 As a result, persons with SCI have a decreased whole-body energy expenditure compared to individuals without SCI,118–120 and a mismatch between excessive intake and expenditure. Subsequently, central adiposity is common among persons with chronic SCI and is more prevalent than in persons without SCI. Importantly, the greatest increase in weight often occurs during the first year post-injury when caloric intake is excessive relative to expenditure.17,121–126
While physical activity has established benefits as a countermeasure to excessive caloric intake some persons with SCI cannot effectively balance energy intake and expenditure with physical activity alone. Some are limited by their level of injury56 and overuse injuries127–129 as well as other documented barriers to exercise.70–71,130–131 Based on the existing evidence, and appreciating that caloric expenditure from physical activity rarely compensates for excessive caloric intake, nutritional modification may represent a more practical and effective target for obesity management and CMD prevention in individuals with SCI. The panel does not recommend a single nutritional plan but notes success in weight loss using the Mediterranean diet in the Diabetes Prevention Program,132–133 and the DASH Diet, which may be more effective for hypertension management.134 The Healthy Mediterranean-Style Pattern is also adapted from the Healthy U.S.-Style Pattern, modifying amounts recommended from some food groups to reflect eating patterns associated with positive health outcomes in studies of Mediterranean-style diets.
Prospective evaluation of weight loss programs in the SCI population has been limited. Weight loss programs designed for the non-disabled population may not be appropriate for the specific health135–139 and nutritional needs140–144 of the SCI population. A pilot study of a weight loss program consisting of education on nutrition, exercise, and behavioral modification in individuals with chronic SCI who were overweight or obese resulted in weight loss and improvements in dietary intake.145 This study utilized the Time-calorie displacement diet, which emphasizes large intakes of high bulk, low energy-density foods such as fruits and vegetables, high-fiber grains, and cereals. It also emphasized a moderate intake of high energy-density foods such as meats, cheeses, sugars, and fats.146
Physical Activity
Panel Findings
Individuals with SCI become physically deconditioned after injury.
Physical deconditioning is associated with a frank diagnosis of CMD or clinical progression of its risk determinants.
Recommendation
-
All individuals with SCI should participate in at least 150 minutes per week of a physical exercise, according to their ability, beginning as soon as possible following acute spinal cord injury. The 150-minutes-per-week guideline can be satisfied by sessions of 30–60 minutes performed three to five days per week, or by exercising for at least three, 10-minute sessions per day. When individuals with SCI are not able to meet these guidelines, they should engage in regular physical activity, according to their abilities, and should avoid inactivity. They should consult their health-care provider about the amounts and types of physical activity that are appropriate for their abilities.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
Persons with SCI occupy the lowest end of the human fitness continuum.55,62 Reduction of fitness after SCI is attributable to various factors including inactivity imposed by diminished active muscle contraction, the need for special equipment and assistance performing exercise, physical and financial barriers, pain, and injury.72,147
Engagement in routine physical exercise and activity is known to improve fitness,148–152 reduce the risk of developing CMD component and non-component conditions, and diminish pathogenicity of CMD component risks severity after diagnosis.153–154 Several prospective and cross-sectional studies in persons with SCI have identified a benefit for physical conditioning in managing selected CMD component risks. These studies mirror studies in the general population that have more extensively identified these benefits and identified exercise as an effective lifestyle plan in both healthy individuals and those with chronic diseases.155
Authoritative guidelines for exercise after SCI have already been established.156–157 The panel recommendations mirror these guidelines, including the U.S. Department of Health and Human Services Physical Activity Guidelines for Individuals with Disabilities.
PHARMACOTHERAPY AND SURGERY FOR CARDIOMETABOLIC RISK
Preamble
The following section provides recommendations for drug therapy addressing specific CMD risk components and surgical countermeasures to CMD in persons with SCI.
Pharmacotherapy for Obesity
Panel Findings
Insufficient evidence to support the use of prescription and non-prescription anti-obesity agents for either short-term or long-term use by persons with SCI.
A need for broadened surveillance and treatment of obesity starting soon after injury, and, for all individuals with SCI, emphasizing patient-centered therapeutic lifestyle change incorporating exercise and nutritional modification where these recommendations have not been implemented.
Recommendations
-
Do not use prescription medications, nutraceuticals, and herbals for the management of obesity in persons with SCI.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Warn healthcare professionals and stakeholders with SCI about the unsupervised use of over-the-counter and herbal anorexigenics, diuretics, and nutrient uptake inhibitors for body fat or mass reduction.
(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
Pharmacological agents, nutraceuticals, and herbal medicines are currently used as alternatives to, or in combination with, behavioral modification, nutritional adjustments, exercise, and surgery to treat obesity. All FDA-approved medications are recommended as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in obese adults, or, overweight patients having at least one weight-related comorbid condition, such as hypertension, type-2 diabetes, or dyslipidemia.158 The following are FDA-approved drugs for treating obesity and overweight:
Orlistat is a potent gastrointestinal lipase inhibitor that reduces dietary fat absorption by approximately 30%. It has not undergone testing for safety, tolerance, or effectiveness in persons with SCI. While the efficacy of orlistat for long-term weight loss has been reported in several RCTs,159–160 a meta-analysis incorporating five studies of 11,000 participants found common gastrointestinal side effects including diarrhea, fecal incontinence, oily spotting, flatulence, bloating, and dyspepsia.161–162 Stringent dietary management focusing on the restriction of fat intake must be undertaken to lessen, but not necessarily eliminate, these risks. The Panel feels that use of the drug in persons with a neurogenic bowel, autonomic dysreflexia, and insensate skin may be significantly disrupting, socially distressing, and potentially hazardous.
Phentermine/topiramate is a multitherapy pharmaceutical containing a low-dose of the centrally acting appetite suppressant phentermine and the antiepileptic agent topiramate. This combination has been shown to be effective for the long-term treatment of obesity,163–164 although topiramate is unlicensed as monotherapy for obesity. The efficacy, tolerance, and safety of this combination drug have not undergone testing in persons with SCI. Phentermine is a sympathomimetic agent that is FDA-approved for up to three months administration but not longer-term use. Sympathomimetic properties pose risks for insomnia, xerostomia, dizziness, palpitation, hand tremor, and elevation of blood pressure and pulse rate.165–166 Topiramate is an anti-seizure agent that may have additive effects for other analeptics, such as those used for neuropathic pain. Tricyclic antidepressants and serotonin reuptake inhibitors potentiate effects of phentermine and have major adverse interactions with phentermine/topiramate. The Panel feels that use of this agent in persons with SCI who have altered function of the autonomic nervous system and who may be taking other medications that interact with phentermine/topiramate is potentially hazardous.
Bupropion/naltrexone is a multitherapy drug containing naltrexone, a synthetic opioid antagonist, and bupropion, an aminoketone antidepressant. The combination has not undergone testing for safety, tolerance, or effectiveness in persons with SCI. In two published clinical trials167–168 the most commonly reported adverse drug events for bupropion/naltrexone sustained release were related to the gastrointestinal system. Nausea was reported in 27%–34% of participants, with an increased risk associated with a higher dosage of the naltrexone component. A headache was reported more often in treatment groups (14% to 24% of participants) than in placebo groups. In both clinical trials, the dose-dependent adverse events of constipation (15%–24%), dizziness (7%–14%), and xerostomia (8%) were higher with the study drug than placebo. There is a potential for interactions with many drug agents, including benzodiazepines, analeptics, and antidepressants. The Panel feels that use of this agent in persons with SCI who have neurogenic bowel, autonomic dysreflexia and who may be taking other medications that may interact with bupropion/naltrexone is potentially hazardous.
Lorcaserin is a 5-hydroxytryptamine (5-HT2C) selective agonist that primarily acts on the hypothalamus to suppress appetite.16 Stimulation of the 5-HT2C receptor may lead to hallucinations, euphoria, or altered mood. Caution is recommended for the use of lorcaserin by individuals with mild-moderate renal dysfunction. As a serotonin agonist, potential interactions may occur with medications that affect serotonergic pathways. The risk of serotonin syndrome and neuroleptic malignant syndrome-like reactions can occur if lorcaserin is used in combination with other serotonergic agents, although these effects have not been studied on persons with an SCI. Interactions can be expected with serotonin-norepinephrine reuptake inhibitors, selective serotonin reuptake inhibitors, tricyclic antidepressants, aminoketone antidepressants, triptans for migraine headaches, tryptophan, dextromethorphan, lithium, tramadol, and drugs used for bipolar disorders.170 The Panel feels that use of this agent in persons with SCI who have a neurogenic bladder, renal dysfunction, autonomic dysreflexia and who may be on other medications that may interact with lorcaserin is potentially hazardous.
In summary, none of the drugs prescribed for treating obesity have undergone extensive clinical testing for safety, tolerance, and effectiveness in the SCI population. All have adverse effects that may substantially affect the overall health, daily function, safety, and comfort of people with SCI. The described agents have extensive drug-drug interactions with agents contained within the pharmacopeia that are typically used to treat SCI. Lifestyle intervention using diet and exercise is an alternative that is deemed by the Panel to be as effective as, and safer than, drug therapies. For these reasons, the Panel feels the medical and social risks of drug use in persons significantly outweigh reported benefits on mass body reduction or cardiovascular disease risk abatement.
Pharmacotherapy for Dysglycemia, Type-2 Pre-Diabetes, and Type-2 Diabetes
Panel Findings
A need for broadened surveillance and treatment of dysglycemia after SCI, while first emphasizing patient-centered therapeutic lifestyle change incorporating behavior, exercise, and nutrition modification where these recommendations have not been implemented.
Recommendations
-
Use a threshold of risk for HbA1c level greater than 7% as a criterion to initiate lifestyle intervention.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
- Anti-hyperglycemic agent or agents should conform to the most recent treatment guidelines when lifestyle intervention does not satisfy glycemic targets.
- Metformin should be the primary agent for treatment of HbA1c >7% unless contraindicated or poorly tolerated. If the maximum tolerated dosage of metformin fails to achieve treatment goals, the addition of a second and possibly a third agent should conform to the most recent treatment guidelines.
- Exercise caution when using multi-therapy approaches, which are more likely to precipitate hypoglycemia. Consider patient-specific characteristics where drug selection that may invoke hypoglycemia, resting and postural hypotension, lymphedema, heart failure, and urinary tract infections.
-
Consider referral to an endocrinologist.(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
Lowering of non-gestational HbA1C with a target of <7% in adults slows microvascular progression of diabetes, and, if implemented soon after the diabetes diagnosis and sustained for the long-term, results in a modest reduction of macrovascular disease. The more conservative A1C goal of <6.5% is preferred for individuals without significant hypoglycemia or other treatment adverse effects.171 These patients may include those with short duration of diabetes, suitable treatment results accompanying lifestyle or metformin monotherapy, long life expectancy, or absence of significant CVD.
The panel recommendations agree substantially with the Pharmacologic Therapy for Type 2 Diabetes: Synopsis of the American Diabetes Association Standards of Medical Care in Diabetes (2017),172 which recommend the following:
Metformin, if not contraindicated and if tolerated, is the preferred initial pharmacologic agent for the treatment of type 2 diabetes.
Long-term use of metformin may be associated with biochemical vitamin B12 deficiency, and periodic measurement of vitamin B12 levels should be considered in metformin-treated patients, especially in those with anemia or peripheral neuropathy.
Consider initiating insulin therapy (with or without additional agents) in patients with newly diagnosed type 2 diabetes who are symptomatic and/or have A1C ≥10% (86 mmol/mol) and/or blood glucose levels ≥300 mg/dL (16.7 mmol/L).
If noninsulin monotherapy at maximum tolerated dose does not achieve or maintain the A1C target after three months, add a second oral agent, a glucagon-like peptide-1 receptor agonist, or basal insulin.
A patient-centered approach should be used to guide the choice of pharmacologic agents. Considerations include efficacy, hypoglycemia risk, impact on weight, potential side effects, cost, and patient preferences.
For patients with type 2 diabetes who are not achieving glycemic goals, insulin therapy should not be delayed.
In patients with long-standing, sub-optimally controlled type 2 diabetes and an established atherosclerotic cardiovascular disease, empagliflozin or liraglutide should be considered as they have been shown to reduce cardiovascular and all-cause mortality when added to standard care. Ongoing studies are investigating the cardiovascular benefits of other agents in these drug classes.
General warnings for GI complications and volume depletion accompany metformin monotherapy, which may be more impactful on persons with SCI and include risks of resting and orthostatic hypotension. A greater risk of hypoglycemia should be anticipated with multitherapy approaches, especially when incorporating sulfonylureas and basal insulin as second-line agents. Risks for genitourinary infection, volume depletion, and resting and orthostatic hypotension may be more pronounced in persons with SCI than the general population and should be judiciously monitored.
Pharmacotherapy for Dyslipidemia
Panel Findings
A need for broadened surveillance and treatment of dyslipidemia in SCI, while first emphasizing therapeutic lifestyle change, including exercise and nutritional modification where these recommendations have not already been implemented.
A threshold of cardiovascular risk or LDL-C for the initiation of statin therapy has not been established in SCI.
Assessment of postprandial lipemia/remnant cholesterol and inflammation (C-reactive protein) may contribute to the detection of SCI patients with risk related to dyslipidemia.
Recommendations
-
Employ caution when using integrated cardiovascular risk equations for the selection of SCI patients for treatment with lipid-lowering therapies, due to the lack of calibration in SCI and the potential under-recognition of cardiovascular risk.
(Scientific evidence: III; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Guide patient selection for pharmacotherapy by other factors commonly seen in SCI, such as low levels of HDL-C and high levels of C-reactive protein. Initiate statin monotherapy using at least a moderate-intensity statin (e.g., rosuvastatin 10–20 mg/day).
(Scientific evidence: III; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
Selection of patients for treatment of dyslipidemia is often based on the use of cardiovascular risk equations developed for use by non-disabled populations, and therefore with uncertain generalizability and calibration to populations with SCI.107,173 In particular, most risk equations, except the Reynolds Risk Score, do not account for the inflammation/lipid interaction and do not incorporate the risk associated with remnant particles or postprandial lipemia.174–175 Given these limitations, typical thresholds for the initiation of pharmacologic treatment of dyslipidemia, developed in non-disabled populations, may not apply to SCI. This finding is significant, as only approximately 25% of patients with SCI meet conventional criteria for the initiation of lipid-lowering therapy.176–177
Data are sparse on the rates of treatment and control of dyslipidemia in SCI, with available evidence suggesting that a therapeutic gap is present,176,178 consistent with data from the National Health and Nutrition Examination Survey in non-disabled persons. Lifestyle intervention for dyslipidemia most effectively incorporates exercise training, which has been shown to reduce LDL-C by up to 25% and increase HDL-C by 10%.179 Otherwise, the use of traditional therapeutic agents potentially effective in SCI-associated dyslipidemia include statins, fibric acid derivatives, and niacin. Statin drugs are effective for dyslipidemia and are demonstrated to reduce the risk of cardiovascular outcomes. Most randomized controlled trials conducted in non-disabled individuals selected subjects by LDL-C. However, recent data from the Heart Outcomes Prevention Evaluation-3 study (HOPE-3) show significantly lower rates of nonfatal cardiovascular events irrespective of LDL-C.180 In this study, patients without known cardiovascular disease were selected for treatment with rosuvastatin 10 mg daily based on the presence of a cardiovascular risk factor to include low HDL-C, or elevated waist-to-hip ratio (common factors seen in SCI). Similarly, selection of patients for treatment using rosuvastatin 20 mg/d based on the presence of elevated levels of subclinical inflammation (C-reactive protein ≥2mg/L) when LDL-C is not elevated (<130 mg/dL) is reasonable based on the results of the JUPITER trial.181 Limited outcomes data in patients with SCI suggest that statins may reduce all-cause mortality.182 Once initiated, statin therapy should be monitored in accordance with the product information per the Food and Drug Administration. A notable exception may be for heightened surveillance for myopathy using creatine kinase monitoring due to the limitations to assessing pain and weakness in the SCI population. There are no outcomes data in the treatment of dyslipidemia in SCI using non-statin therapies, such as niacin or fibric acid derivatives. Niacin tolerably improves the dyslipidemic risk profile in SCI.183 Fibrates (gemfibrozil, bezafibrate) also improve the dyslipidemia risk profile and reduce cardiovascular outcomes in nondisabled dyslipidemic patients.
Pharmacotherapy for Hypertension
Panel Findings
The Panel finds insufficient evidence to support a different threshold than the general population for treating high blood pressure in individuals with spinal cord injury.
Recommendations
-
Use evidence-based guidelines for treating hypertension in the general population to treat individuals with SCI. For most adults, consider a threshold for initiating pharmacological treatment and treatment target of 140/90 mm Hg as reasonable, although consider different targets in certain individuals and sub-populations.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Consider SCI-related factors when selecting an antihypertensive agent, such as the effect of thiazide diuretics on bladder management.
(Scientific evidence: IV; Grade of recommendation: C; Level of Panel Recommendation: Strong)
Rationale
Abundant evidence from randomized, controlled trials in the general population has shown the benefit of antihypertensive drug treatment in improving important health outcomes in people with hypertension. Baseline blood pressure is often lower in people with tetraplegia and high paraplegia than in the general population, but evidence to support a different threshold for treating high blood pressure in individuals with spinal cord injury is lacking. The Panel recommends also applying evidence-based guidelines for treating hypertension in the general population to those with SCI. Current guidelines for initiating pharmacological treatment for hypertension by most major organizations recommend 140/90 mm Hg as the threshold for pharmacological treatment and target goal for most adults with hypertension. However, there are differences and areas of controversy regarding treatment thresholds and targets for certain sub-populations between the different guidelines. For example, in age cutoff for a higher systolic BP target and treatment threshold, a lower BP threshold is recommended by some organizations for certain populations, including those with diabetes or chronic kidney disease.184–187
The Eighth Joint National Committee (JNC 8) evidence-based guideline for the management of high blood pressure in adults recommends initiating pharmacological treatment to lower blood pressure at systolic blood pressure (SBP) of 140 mm Hg or higher or diastolic blood pressure (DBP) of 90 mm Hg or higher in adults under 60 years, and in all adults with diabetes or chronic kidney disease regardless of age, and at SBP of 150 mm Hg or higher or DPB of 90 mm Hg or higher in adults age 60 or higher without diabetes or chronic kidney disease.184 Guidelines from the American College of Physicians and the American Academy of Family Physicians (ACP/AAFP) recommend the same threshold for initiating treatment and target goal as JNC 8 for adults aged 60 or older.185 The American Society of Hypertension and the International Society of Hypertension (ASH/ISH) guidelines for the management of hypertension have similar treatment threshold and target goals as the JNC 8 guidelines, except for a higher age cut-off (80 years or older versus 60 years) for using a 150 mm Hg SBP target instead of 140 mm Hg in adults without diabetes or chronic kidney disease.186 A science advisory from the AHA, the American College of Cardiology (ACC), and the Centers for Disease Control and Prevention (CDC) specifies that for most adults the BP goal is less than 140/90; however, lower targets may be appropriate for some populations.187
Consistent with the above guidelines, the Panel recommends initiating pharmacological treatment to lower blood pressure at SBP of 140 mm Hg or higher or DBP of 90 mm Hg or higher in most adults with SCI. While the Panel recognizes differences in treatment goals and targets for certain sub-populations between various guidelines, it does not endorse a specific guideline over the others given the current lack of high-quality evidence to make that determination. For individual patients, clinicians should use a combination of factors to set BP goals, including scientific evidence, clinical judgment, and patient tolerance. In some patients, including those with albuminuria, chronic kidney disease, or additional cardiovascular risk factors, clinicians could consider a lower BP target (for example 130/80 mm Hg) if lower targets can be achieved without undue treatment burden, while recognizing that the benefit of pursuing these targets levels using antihypertensive drugs is currently not established through RCTs.
Evidence-based guidelines for choosing antihypertensive medications in the general population are based on randomized controlled trials studying comparative benefit and harm of different agents on specific health outcomes. JNC 8 guidelines recommend initial antihypertensive treatment with a thiazide-type diuretic, calcium channel blocker (CCB), angiotensin-converting enzyme inhibitor (ACEI), or angiotensin receptor blocker (ARB) in the non-black population, and either a thiazide-type diuretic or CCB in the black population.184 In adults with chronic kidney disease, initial or add-on antihypertensive treatment should include an ACEI or ARB to improve kidney outcomes. Additional co-existing conditions may influence drug selection. For example, in those with a history of myocardial infarction, a beta-blocker and ARB/ or ACEI are indicated regardless of blood pressure.186
Studies to systematically test antihypertensive agents in people with SCI are lacking. In the absence of such evidence, it is reasonable to apply guidelines for choosing antihypertensive agents in the general population to people with SCI. However, SCI-related factors may affect the choice of an antihypertensive agent in some circumstances. For example, a thiazide-type diuretic may not be the antihypertensive agent of choice in individuals who perform intermittent bladder catheterizations, because of its effect on increased urine volumes between catheterizations. Hyponatremia, hypokalemia, or decline in renal function sometimes occur during the first nine months of thiazide use, and older patients may be especially vulnerable to renal-electrolyte disturbances, gout, hyperglycemia, and hypotension.
The main objective of hypertension treatment is to attain and maintain goal blood pressure. JNC 8 guidelines recommend increasing the dose of the initial drug or adding a second drug if goal blood pressure is not reached within a month of initiating treatment.184 An ACEI and an ARB should not be used together in the same patient. If goal BP cannot be achieved with two drugs, a third drug should be added and titrated. A study by Barry et al. found that veterans with traumatic SCI were less likely to be prescribed more than one antihypertensive medication when compared with matched controls.46 The authors postulated that these findings could relate to concern over the propensity of these patients to develop hypotension. While some patients with SCI who have co-existing orthostatic hypotension and supine hypertension require careful titration and trial of medications, clinicians should continue to assess blood pressure and adjust the treatment regimen until goal blood pressure is reached.
In those with treatment-resistant hypertension, compliance and adherence to treatment regimen should be confirmed. Clinician empathy increases patient trust, motivation, and adherence to therapy. Drug interactions (e.g., nonsteroidal anti-inflammatory drugs, illicit drugs, sympathomimetic agents, over-the-counter drugs and herbal supplements) may hamper blood pressure control and should be considered. Secondary causes of hypertension should be investigated. Referral to a hypertension specialist may be appropriate for those whose blood pressure cannot be controlled with the above strategies.186
Self-monitoring of BP should be encouraged for most patients with hypertension. System-level strategies should be considered to improve hypertension treatment, including: identifying all patients eligible for management, monitoring at the practice level, increasing patient and provider awareness, systematic follow-up of patients for the initiation and maintenance/intensification of therapy, clarifying roles of healthcare providers to implement a team approach and reducing barriers for patients to receive and adhere to medications.187
Bariatric Surgery for CMD Risk
Panel Findings
The evidence fails to support bariatric surgery for obesity management after SCI, except in cases of last resort.
Recommendations
- Consider bariatric surgery as a last resort for persons with morbid obesity and spinal cord injury, due to the significant peri- and postoperative risks.
-
An SCI specialist should provide preoperative, perioperative and post-operative consultative services to the surgical and anesthesia teams to alert them to unique risks associated with SCI.(Scientific evidence: V; Grade of recommendation: C; Level of Panel Recommendation: Strong)
-
Rationale
There have been no Level I, II or III studies investigating bariatric surgery to manage obesity in persons with SCI. Of the few case reports in the literature, none address the unique perioperative or post-operative risks of the procedure in this special population.188–190 Current guidelines for determining bariatric surgery candidates and their perioperative/post-operative care in Europe and the United States utilize BMI and screening practices suitable to the non-SCI population,191–192 but do not address the complex care needs/risks associated with SCI, including but not limited to paralysis, mobility and activities of daily living deficits, neurogenic bradycardia, neurogenic hypotension, adapted myocardial atrophy, circulatory hypokinesis, risk for autonomic dysreflexia, neurogenic restrictive and obstructive lung disease, neurogenic bladder, neurogenic bowel, neurogenic skin, sarcopenia, osteopenia/osteoporosis, and spasticity. While the odds ratio for venous thromboembolism in SCI after bariatric surgery has recently been determined as 5.71 (95% CI 1.36–24.02) based on 83 individuals with paraplegia in a total sample of 91,963193 other potential complications associated with such surgeries, including abdominal pain/cramping, dumping syndrome, beriberi, postoperative adhesions and loose stools have not been characterized or reported.
Directions for Future Research
In general, additional and larger population-based trials assessing risk and interventions that are discriminated by key levels of injury are needed.
Multicenter and central database studies should focus on hard endpoints, such as event rates of diabetes, myocardial infarction, stroke, and death, as well as component risks of CMD.
More targeted post-mortem determinations and retrospective chart reviews should be used to assess CMD as a cause of death after SCI.
Given their unique physiology, guideline-supported interventions derived from the general population should be assessed for safety and efficacy in persons with SCI.
Studies that rank-order CMD component risks for the SCI population should be undertaken so that hazards may be aggressively addressed. Emphasis should be directed toward early post-injury obesity and diabetes prevention.
The role of autonomic dysfunction and autonomic dysreflexia in disease progression and risk determination requires additional study.
The population hazards for non-traditional, population-specific risk factors should be better determined, including inflammatory biomarkers, physical deconditioning, the human microbiome, and others.
Subpopulation risk assessments based on race, gender, pre-injury risks, and unique subpopulations – including veterans – are needed to discriminate risk, identification, and management.
Population-specific risk prediction equations that model after Framingham should be studied, and modified if possible, for the SCI population to forecast future risks for all-cause events and death.
Big data descriptions of CMD prevalence (i.e., using electronic health records, Veteran's Health Administration, private or public insurance data, etc.) should be pursued.
Randomized trials of screened/unscreened populations and controlled interventions are needed within the SCI population.
Determine the cost-effectiveness of aggressive surveillance and early intervention for CMD risk and diagnosis among people with SCI.
Education initiatives should target primary care providers and consumers with greater knowledge of CMD identification, treatment initiation, and management in this population.
Population-specific prediction equations for energy expenditure need to be developed and validated.
Identification of population-specific pharmacotherapy and related treatment benefits, risks, and all-cause burdens are required to better understand and implement best practice.
Imaging and phenotypic assessments should be targeted to develop and optimize integrated risk markers and tools for early screening and detection of CMD.
Footnotes
Nomenclature for Rating of Evidence and Strength of Panel Agreement
Cited Literature
- 1.Alberti KG, Zimmet P, Shaw J. Metabolic syndrome--a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabetic Med. 2006;23(5):469–480. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 2.Alberti K, Eckel RH, Grundy SM et al. Harmonizing the Metabolic Syndrome: A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 3.Grundy SM, Brewer HB, Jr., Cleeman JI et al. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109(3):433–438. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 4.Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. DiabetesCare. 2005;28(7):1769–1778. doi: 10.2337/diacare.28.7.1769. [DOI] [PubMed] [Google Scholar]
- 5.Ford ES, Abbasi F, Reaven GM. Prevalence of insulin resistance and the metabolic syndrome with alternative definitions of impaired fasting glucose. Atherosclerosis. 2005;181(1):143–148. doi: 10.1016/j.atherosclerosis.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the US. Diabetes Care. 2005;28(11):2745–2749. doi: 10.2337/diacare.28.11.2745. [DOI] [PubMed] [Google Scholar]
- 7.Groah SL, Nash MS, Ward EA et al. Cardiometabolic risk in community-dwelling persons with chronic spinal cord injury. J Cardiopulm Rehabil Prev. 2011;31(2):73–80. doi: 10.1097/HCR.0b013e3181f68aba. [DOI] [PubMed] [Google Scholar]
- 8.Jialal I, Devaraj S, Venugopal SK. C-reactive protein: risk marker or mediator in atherothrombosis? Hypertension. 2004;44(1):6–11. doi: 10.1161/01.HYP.0000130484.20501.df. [DOI] [PubMed] [Google Scholar]
- 9.Tracy RP. Inflammation, the metabolic syndrome and cardiovascular risk. Int J Clin Pract Suppl. 2003;(134):10–17. [PubMed] [Google Scholar]
- 10.Liang H, Chen D, Wang Y, Rimmer JH, Braunschweig CL. Different risk factor patterns for metabolic syndrome in men with spinal cord injury compared with able-bodied men despite similar prevalence rates. Arch Phys Med Rehabil. 2007;88(9):1198–1204. doi: 10.1016/j.apmr.2007.05.023. [DOI] [PubMed] [Google Scholar]
- 11.Libin A, Tinsley E, Nash M et al. Cardiometabolic risk clustering in spinal cord injury: results of exploratory factor analysis. Topics in Spinal Cord Injury Rehabilitation. 2013;19(3):183–194. doi: 10.1310/sci1903-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grundy SM, Cleeman JI, Merz CN et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol. 2004;44(3):720–732. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 13.Bray GA, Champagne CM. Beyond energy balance: there is more to obesity than kilocalories. J Am Diet Assoc. 2005;105(5):17–23. doi: 10.1016/j.jada.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 14.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–253. [PubMed] [Google Scholar]
- 15.Liang H, Chen D, Wang Y, Rimmer JH, Braunschweig CL. Different risk factor patterns for metabolic syndrome in men with spinal cord injury compared with able-bodied men despite similar prevalence rates. Arch Phys Med Rehabil. 2007;88(9):1198–1204. doi: 10.1016/j.apmr.2007.05.023. [DOI] [PubMed] [Google Scholar]
- 16.Wahman K, Nash MS, Westgren N, Lewis JE, Seiger A, Levi R. Cardiovascular disease risk factors in persons with paraplegia: the Stockholm spinal cord injury study. J Rehabil Med. 2010;42(3):272–278. doi: 10.2340/16501977-0510. [DOI] [PubMed] [Google Scholar]
- 17.Spungen AM, Wang J, Pierson RN, Bauman WA. Soft tissue body composition differences in monozygotic twins discordant for spinal cord injury. J Appl Physiol. 2000;88(4):1310–1315. doi: 10.1152/jappl.2000.88.4.1310. [DOI] [PubMed] [Google Scholar]
- 18.Yarar-Fisher C, Chen Y, Jackson AB, Hunter GR. Body mass index underestimates adiposity in women with spinal cord injury. Obesity. 2013;21(6):1223–1225. doi: 10.1002/oby.20199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beck LA, Lamb JL, Atkinson EJ, Wuermser L-A, Amin S. Body composition of women and men with complete motor paraplegia. J Spinal Cord Med. 2014;37(4):359–365. doi: 10.1179/2045772313Y.0000000151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buchholz AC, McGillivray CF, Pencharz PB. The use of bioelectric impedance analysis to measure fluid compartments in subjects with chronic paraplegia. Arch Phys Med Rehabil. 2003;84(6):854–861. doi: 10.1016/s0003-9993(02)04950-x. [DOI] [PubMed] [Google Scholar]
- 21.Cirnigliaro CM, LaFountaine MF, Dengel DR et al. Visceral adiposity in persons with chronic spinal cord injury determined by dual energy X-Ray absorptiometry. Obesity. 2015;23(9):1811–1817. doi: 10.1002/oby.21194. [DOI] [PubMed] [Google Scholar]
- 22.Clasey JL, Gater DR. A comparison of hydrostatic weighing and air displacement plethysmography in adults with spinal cord injury. Arch Phys Med Rehabil. 2005;86(11):2106–2113. doi: 10.1016/j.apmr.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 23.Gorgey AS, Gater DR. Regional and relative adiposity patterns in relation to carbohydrate and lipid metabolism in men with spinal cord injury. Appl Physiol Nutr Metab = Physiologie appliquee, nutrition et metabolisme. 2011;36(1):107–114. doi: 10.1139/H10-091. [DOI] [PubMed] [Google Scholar]
- 24.Gorgey AS, Mather KJ, Poarch HJ, Gater DR. Influence of motor complete spinal cord injury on visceral and subcutaneous adipose tissue measured by multi-axial magnetic resonance imaging. J Spinal Cord Med. 2011;34(1):99–109. doi: 10.1179/107902610X12911165975106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gater DR, Farkas GJ. The Physiology of Exercise in Spinal Cord Injury. Springer; 2016. Alterations in Body Composition After SCI and the Mitigating Role of Exercise; pp. 175–198. [Google Scholar]
- 26.Lavela SL, Weaver FM, Goldstein B et al. Diabetes mellitus in individuals with spinal cord injury or disorder. J Spinal Cord Med. 2006;29(4):387–395. doi: 10.1080/10790268.2006.11753887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.LaVela SL, Evans CT, Prohaska TR, Miskevics S, Ganesh SP, Weaver FM. Males aging with a spinal cord injury: prevalence of cardiovascular and metabolic conditions. Arch Phys Med Rehabil. 2012;93(1):90–95. doi: 10.1016/j.apmr.2011.07.201. [DOI] [PubMed] [Google Scholar]
- 28.Rajan S, McNeely MJ, Hammond M, Goldstein B, Weaver F. Association between obesity and diabetes mellitus in veterans with spinal cord injuries and disorders. Am J Phys Med Rehabil/Association of Academic Physiatrists. 2010;89(5):353–361. doi: 10.1097/PHM.0b013e3181d896b9. [DOI] [PubMed] [Google Scholar]
- 29.Wahman K, Nash MS, Lewis JE, Seiger A, Levi R. Increased cardiovascular disease risk in Swedish persons with paraplegia: The Stockholm spinal cord injur y study. J Rehabil Med. 2010;42(5):489–492. doi: 10.2340/16501977-0541. [DOI] [PubMed] [Google Scholar]
- 30.Cragg JJ, Noonan VK, Dvorak M, Krassioukov A, Mancini GB, Borisoff JF. Spinal cord injury and type 2 diabetes: results from a population health survey. Neurology. 2013;81(21):1864–1868. doi: 10.1212/01.wnl.0000436074.98534.6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung W-S, Lin C-L, Chang S-N, Chung H-A, Sung F-C, Kao C-H. Increased risk of deep vein thrombosis and pulmonary thromboembolism in patients with spinal cord injury: a nationwide cohort prospective study. Thromb Res. 2014;133(4):579–584. doi: 10.1016/j.thromres.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 32.Imai K, Kadowaki T, Aizawa Y, Fukutomi K. Problems in the health management of persons with spinal cord injury. J Clin Epidemiol. 1996;49(5):505–510. doi: 10.1016/0895-4356(95)00576-5. [DOI] [PubMed] [Google Scholar]
- 33.Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Castillo C, Gater DR. Effects of spinal cord injury on body composition and metabolic profile–Part I. J Spinal Cord Med. 2014;37(6):693–702. doi: 10.1179/2045772314Y.0000000245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Myers J, Lee M, Kiratli J. Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation, and management. Am J Phys Med Rehabil. 2007;86(2):142–152. doi: 10.1097/PHM.0b013e31802f0247. [DOI] [PubMed] [Google Scholar]
- 35.Bauman W, Kahn N, Grimm D, Spungen A. Risk factors for atherogenesis and cardiovascular autonomic function in persons with spinal cord injury. Spinal Cord. 1999;37(9):601–616. doi: 10.1038/sj.sc.3100911. [DOI] [PubMed] [Google Scholar]
- 36.Gilbert O, Croffoot JR, Taylor AJ, Nash M, Schomer K, Groah S. Serum lipid concentrations among persons with spinal cord injury – A systematic review and meta-analysis of the literature. Atherosclerosis. 2014;232(2):305–312. doi: 10.1016/j.atherosclerosis.2013.11.028. [DOI] [PubMed] [Google Scholar]
- 37.Wahman K, Nash MS, Lewis JE, Seiger Å, Levi R. Increased cardiovascular disease risk in Swedish persons with paraplegia: The Stockholm spinal cord injury study. J Rehabil Med. 2010;42(5):489–492. doi: 10.2340/16501977-0541. [DOI] [PubMed] [Google Scholar]
- 38.Bauman W, Adkins R, Spungen A et al. Is immobilization associated with an abnormal lipoprotein profile? Observations from a diverse cohort. Spinal Cord. 1999;37(7):485–493. doi: 10.1038/sj.sc.3100862. [DOI] [PubMed] [Google Scholar]
- 39.Washburn R, Figoni S. High density lipoprotein cholesterol in individuals with spinal cord injury: the potential role of physical activity. Spinal Cord. 1999;37(10) doi: 10.1038/sj.sc.3100917. [DOI] [PubMed] [Google Scholar]
- 40.Nash MS, Mendez AJ. A guideline-driven assessment of need for cardiovascular disease risk intervention in persons with chronic paraplegia. Arch Phys Med Rehabil. 2007;88(6):751–757. doi: 10.1016/j.apmr.2007.02.031. [DOI] [PubMed] [Google Scholar]
- 41.Zlotolow SP, Levy E, Bauman WA. The serum lipoprotein profile in veterans with paraplegia: the relationship to nutritional factors and body mass index. J Am Paraplegia Soc. 1992;15(3):158–162. doi: 10.1080/01952307.1992.11735869. [DOI] [PubMed] [Google Scholar]
- 42.Bauman W, Spungen A, Zhong Y-G, Rothstein J, Petry C, Gordon S. Depressed serum high density lipoprotein cholesterol levels in veterans with spinal cord injury. Spinal Cord. 1992;30(10):697–703. doi: 10.1038/sc.1992.136. [DOI] [PubMed] [Google Scholar]
- 43.Krum H, Howes L, Brown DJ et al. Risk factors for cardiovascular disease in chronic spinal cord injury patients. Spinal Cord. 1992;30(6):381–388. doi: 10.1038/sc.1992.87. [DOI] [PubMed] [Google Scholar]
- 44.Lieberman J, Goff J, David, Hammond F et al. Dietary intake relative to cardiovascular disease risk factors in individuals with chronic spinal cord injury: a pilot study. Top Spinal Cord Inj Rehabil. 2014;20(2):127–136. doi: 10.1310/sci2002-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tóth PP, Potter D, Ming EE. Prevalence of lipid abnormalities in the United States: the national health and nutrition examination survey 2003–2006. J Clin Lipidol. 2012;6(4):325–330. doi: 10.1016/j.jacl.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 46.Barry W, St Andre J, Evans C et al. Hypertension and antihypertensive treatment in veterans with spinal cord injury and disorders. Spinal Cord. 2013;51(2):109–115. doi: 10.1038/sc.2012.122. [DOI] [PubMed] [Google Scholar]
- 47.Zhu C, Galea M, Livote E, Signor D, Wecht JM. A retrospective chart review of heart rate and blood pressure abnormalities in veterans with spinal cord injury. J Spinal Cord Med. 2013;36(5):463–475. doi: 10.1179/2045772313Y.0000000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wecht JM, Zhu C, Weir JP, Yen C, Renzi C, Galea M. A prospective report on the prevalence of heart rate and blood pressure abnormalities in veterans with spinal cord injuries. J Spinal Cord Med. 2013;36(5):454–462. doi: 10.1179/2045772313Y.0000000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weaver FM, Collins EG, Kurichi J et al. Prevalence of obesity and high blood pressure in veterans with spinal cord injuries and disorders - A retrospective review. AmJ Phys Med Rehabil. 2007;86(1):22–29. doi: 10.1097/phm.0b013e31802b8937. [DOI] [PubMed] [Google Scholar]
- 50.Hitzig SL, Tonack M, Campbell KA et al. Secondary health complications in an aging Canadian spinal cord injury sample. Am J Phys Med Rehabil. 2008;87(7):545–555. doi: 10.1097/PHM.0b013e31817c16d6. [DOI] [PubMed] [Google Scholar]
- 51.Garber CE, Blissmer B, Deschenes MR et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sport Exer. 2011;43(7):1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 52.Thompson WR GN, Pescatello LS. ACSM's Guidelines for Exercise Testing and Prescription. 9th ed. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 53.Ginis KA, Hicks AL, Latimer AE et al. The development of evidence-informed physical activity guidelines for adults with spinal cord injury. Spinal Cord. 2011;49(11):1088–1096. doi: 10.1038/sc.2011.63. [DOI] [PubMed] [Google Scholar]
- 54.Association APT Physical Fitness for Individuals with Spinal Cord Injury. Alexandria, VA: American Physical Therapy Association; 2015. [Google Scholar]
- 55.Dearwater SR, LaPorte RE, Robertson RJ, Brenes G, Adams LL, Becker D. Activity in the spinal cord-injured patient: an epidemiologic analysis of metabolic parameters. Med Sci Sports Exerc. 1986;18(5):541–544. [PubMed] [Google Scholar]
- 56.Noreau L, Shephard RJ, Simard C, Pare G, Pomerleau P. Relationship of impairment and functional ability to habitual activity and fitness following spinal cord injury. Int J Rehabil Res. 1993;16(4):265–275. doi: 10.1097/00004356-199312000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Ginis KA, Latimer AE, Arbour-Nicitopoulos KP et al. Leisure time physical activity in a population-based sample of people with spinal cord injury part I: demographic and injury-related correlates. Arch Phys Med Rehabil. 2010;91(5):722–728. doi: 10.1016/j.apmr.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 58.Miller LE, Herbert WG. Health and economic benefits of physical activity for patients with spinal cord injury. Clinicoecon Outcomes Res. 2016;8:551–558. doi: 10.2147/CEOR.S115103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Simmons OL, Kressler J, Nash MS. Reference Fitness Values in the Untrained Spinal Cord Injury Population. Arch Phys Med Rehabil. 2014 doi: 10.1016/j.apmr.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 60.Bostom AG, Toner MM, McArdle WD, Montelione T, Brown CD, Stein RA. Lipid and lipoprotein profiles relate to peak aerobic power in spinal cord injured men. Med Sci Sports Exerc. 1991;23(4):409–414. [PubMed] [Google Scholar]
- 61.Brenes G, Dearwater S, Shapera R, LaPorte RE, Collins E. High density lipoprotein cholesterol concentrations in physically active and sedentary spinal cord injured patients. Arch Phys Med Rehabil. 1986;67(7):445–450. [PubMed] [Google Scholar]
- 62.LaPorte RE, Adams LL, Savage DD, Brenes G, Dearwater S, Cook T. The spectrum of physical activity, cardiovascular disease and health: an epidemiologic perspective. Am J Epidemiol. 1984;120(4):507–517. doi: 10.1093/oxfordjournals.aje.a113911. [DOI] [PubMed] [Google Scholar]
- 63.LaPorte RE, Brenes G, Dearwater S et al. HDL cholesterol across a spectrum of physical activity from quadriplegia to marathon running. Lancet. 1983;1(8335):1212–1213. doi: 10.1016/s0140-6736(83)92482-0. [DOI] [PubMed] [Google Scholar]
- 64.Bauman WA, Spungen AM, Zhong YG, Rothstein JL, Petry C, Gordon SK. Depressed serum high density lipoprotein cholesterol levels in veterans with spinal cord injury. Paraplegia. 1992;30(10):697–703. doi: 10.1038/sc.1992.136. [DOI] [PubMed] [Google Scholar]
- 65.Halle M, Berg A, Baumstark M, Keul J. Association of physical fitness with LDL and HDL subfractions in young healthy men. Int J Sports Med. 1999;20(7):464–469. doi: 10.1055/s-1999-8833. [DOI] [PubMed] [Google Scholar]
- 66.Franks PW, Ekelund U, Brage S, Wong M-Y, Wareham NJ. Does the association of habitual physical activity with the metabolic syndrome differ by level of cardiorespiratory fitness? Diabetes Care. 2004;27(5):1187–1193. doi: 10.2337/diacare.27.5.1187. [DOI] [PubMed] [Google Scholar]
- 67.Carnethon MR, Gulati M, Greenland P. Prevalence and cardiovascular disease correlates of low cardiorespiratory fitness in adolescents and adults. J Am Med Assoc. 2005;294(23):2981–2988. doi: 10.1001/jama.294.23.2981. [DOI] [PubMed] [Google Scholar]
- 68.Cowan RE, Nash MS, Anderson KD. Exercise participation barrier prevalence and association with exercise participation status in individuals with spinal cord injury. Spinal Cord. 2013;51(1):27–32. doi: 10.1038/sc.2012.53. [DOI] [PubMed] [Google Scholar]
- 69.Ginis KA, Latimer AE, Arbour-Nicitopoulos KP et al. Leisure time physical activity in a population-based sample of people with spinal cord injury part I: demographic and injury-related correlates. Arch Phys Med Rehabil. 2010;91(5):722–728. doi: 10.1016/j.apmr.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 70.Scelza WM, Kalpakjian CZ, Zemper ED, Tate DG. Perceived barriers to exercise in people with spinal cord injury. Am J Phys Med Rehabil. 2005;84(8):576–583. doi: 10.1097/01.phm.0000171172.96290.67. [DOI] [PubMed] [Google Scholar]
- 71.Vissers M, van den Berg-Emons R, Sluis T, Bergen M, Stam H, Bussmann H. Barriers to and facilitators of everyday physical activity in persons with a spinal cord injury after discharge from the rehabilitation centre. J Rehabil Med. 2008;40(6):461–467. doi: 10.2340/16501977-0191. [DOI] [PubMed] [Google Scholar]
- 72.Cowan RE, Nash MS, Anderson KD. Exercise participation barrier prevalence and association with exercise participation status in individuals with spinal cord injury. Spinal Cord. 2012 doi: 10.1038/sc.2012.53. [DOI] [PubMed] [Google Scholar]
- 73.Pearson TA, Mensah GA, Alexander RW et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107(3):499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 74.Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342(12):836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- 75.Cragg JJ, Stone JA, Krassioukov AV. Management of cardiovascular disease risk factors in individuals with chronic spinal cord injury: an evidence-based review. J Neurotraum. 2012;29(11):1999–2012. doi: 10.1089/neu.2012.2313. [DOI] [PubMed] [Google Scholar]
- 76.Lee M, Myers J, Hayes A et al. C-reactive protein, metabolic syndrome, and insulin resistance in individuals with spinal cord injury. J Spinal Cord Med. 2005;28(1):20–25. doi: 10.1080/10790268.2005.11753794. [DOI] [PubMed] [Google Scholar]
- 77.Wang TD, Wang YH, Huang TS, Su TC, Pan SL, Chen SY. Circulating levels of markers of inflammation and endothelial activation are increased in men with chronic spinal cord injury. J Formos Med Assoc. 2007;106(11):919–928. doi: 10.1016/S0929-6646(08)60062-5. [DOI] [PubMed] [Google Scholar]
- 78.Frost F, Roach MJ, Kushner I, Schreiber P. Inflammatory C-reactive protein and cytokine levels in asymptomatic people with chronic spinal cord injury. Arch Phys Med Rehabil. 2005;86(2):312–317. doi: 10.1016/j.apmr.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 79.Davies AL, Hayes KC, Dekaban GA. Clinical correlates of elevated serum concentrations of cytokines and autoantibodies in patients with spinal cord injury. Arch Phys Med Rehabil. 2007;88(11):1384–1393. doi: 10.1016/j.apmr.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 80.Gibson A, Buchholz A, Ginis KM. C-Reactive protein in adults with chronic spinal cord injury: increased chronic inflammation in tetraplegia vs paraplegia. Spinal Cord. 2008;46(9):616–621. doi: 10.1038/sc.2008.32. [DOI] [PubMed] [Google Scholar]
- 81.Spungen AM, Wang J, Pierson RN, Bauman WA. Soft tissue body composition differences in monozygotic twins discordant for spinal cord injury. J Appl Physiol. 2000;88(4):1310–1315. doi: 10.1152/jappl.2000.88.4.1310. [DOI] [PubMed] [Google Scholar]
- 82.Yarar-Fisher C, Chen Y, Jackson AB, Hunter GR. Body mass index underestimates adiposity in women with spinal cord injury. Obesity (Silver Spring) 2013;21(6):1223–1225. doi: 10.1002/oby.20199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Beck LA, Lamb JL, Atkinson EJ, Wuermser L-A, Amin S. Body composition of women and men with complete motor paraplegia. J Spinal Cord Med. 2014;37:359–365. doi: 10.1179/2045772313Y.0000000151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Buchholz AC, McGillivray CF, Pencharz PB. The use of bioelectric impedance analysis to measure fluid compartments in subjects with chronic paraplegia. Arch Phys Med Rehabil. 2003;84(6):854–861. doi: 10.1016/s0003-9993(02)04950-x. [DOI] [PubMed] [Google Scholar]
- 85.Cirnigliaro CM, LaFountaine MF, Dengel DR et al. Visceral adiposity in persons with chronic spinal cord injury determined by dual energy X-ray absorptiometry. Obesity (Silver Spring) 2015;23(9):1811–1817. doi: 10.1002/oby.21194. [DOI] [PubMed] [Google Scholar]
- 86.Clasey JL, Gater DR. A comparison of hydrostatic weighing and air displacement plethysmography in adults with spinal cord injuries. Arch Phys Med Rehabil. 2005;86(11):2106–2113. doi: 10.1016/j.apmr.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 87.Gorgey AS, Gater DR. Regional and relative adiposity patterns in relation to carbohydrate and lipid metabolism in men with spinal cord injury. Appl Physiol Nutr Metab. 2011;36(1):107–114. doi: 10.1139/H10-091. [DOI] [PubMed] [Google Scholar]
- 88.Gorgey AS, Mather KJ, Poarch HJ, Gater DR. Influence of motor complete spinal cord injury on visceral and subcutaneous adipose tissue measured by multi-axial magnetic resonance imaging. J Spinal Cord Med. 2011;34:99–109. doi: 10.1179/107902610X12911165975106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Maggioni M, Bertoli S, Margonato V, Merati G, Veicsteinas A, Testolin G. Body composition assessment in spinal cord injury subjects. Acta Diabetol. 2003;40:S183–S186. doi: 10.1007/s00592-003-0061-7. [DOI] [PubMed] [Google Scholar]
- 90.Maruyama Y, Mizuguchi M, Yaginuma T et al. Serum leptin, abdominal obesity and the metabolic syndrome in individuals with chronic spinal cord injury. Spinal Cord. 2008;46(7):494–499. doi: 10.1038/sj.sc.3102171. [DOI] [PubMed] [Google Scholar]
- 91.Spungen AM, Adkins RH, Stewart CA et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol. 2003;95(6):2398–2407. doi: 10.1152/japplphysiol.00729.2002. [DOI] [PubMed] [Google Scholar]
- 92.Barry W, St Andre JR, Evans CT et al. Hypertension and antihypertensive treatment in veterans with spinal cord injury and disorders. Spinal Cord. 2013;51(2):109–115. doi: 10.1038/sc.2012.122. [DOI] [PubMed] [Google Scholar]
- 93.Bauman WA, Adkins RH, Spungen AM et al. Is immobilization associated with an abnormal lipoprotein profile? Observations from a diverse cohort. Spinal Cord. 1999;37(7):485–493. doi: 10.1038/sj.sc.3100862. [DOI] [PubMed] [Google Scholar]
- 94.Chen YY, Cao Y, Allen V, Richards JS. Weight Matters: Physical and Psychosocial Well Being of Persons With Spinal Cord Injury in Relation to Body Mass Index. Arch Phys Med Rehabil. 2011;92(3):391–398. doi: 10.1016/j.apmr.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 95.Rajan S, McNeely MJ, Hammond M, Goldstein B, Weaver F. Association Between Obesity and Diabetes Mellitus in Veterans With Spinal Cord Injuries and Disorders. Am J Phys Med Rehabil. 2010;89(5):353–361. doi: 10.1097/PHM.0b013e3181d896b9. [DOI] [PubMed] [Google Scholar]
- 96.Wahman K, Nash MS, Lewis JE, Seiger A, Levi R. Increased cardiovascular disease risk in Swedish persons with paraplegia: The Stockholm Spinal Cord Injury Study. J Rehabil Med. 2010;42(5):489–492. doi: 10.2340/16501977-0541. [DOI] [PubMed] [Google Scholar]
- 97.Zhu C, Galea M, Livote E, Signor D, Wecht JM. A retrospective chart review of heart rate and blood pressure abnormalities in veterans with spinal cord injury. J Spinal Cord Med. 2013;36(5):463–475. doi: 10.1179/2045772313Y.0000000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Liang HF, Chen D, Braunschweig CL. Elevated C-reactive protein and better insulin sensitivity in men with spinal cord injury compared to able- bodied men. Diabetes. 2007;56:A246–A246. [Google Scholar]
- 99.Marathe PH, Gao HX, Close KL. American Diabetes Association Standards of Medical Care in Diabetes 2017. J Diabetes. 2017 doi: 10.1111/1753-0407.12524. [DOI] [PubMed] [Google Scholar]
- 100.Bauman WA, Spungen AM. Carbohydrate and lipid metabolism in chronic spinal cord injury. J Spinal Cord Med. 2001;24(4):266–277. doi: 10.1080/10790268.2001.11753584. [DOI] [PubMed] [Google Scholar]
- 101.Gorgey AS. Exercise awareness and barriers after spinal cord injury. World J Orthop. 2014;5(3):158–162. doi: 10.5312/wjo.v5.i3.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pickering TG, Hall JE, Appel LJ et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 103.Mathias CJ. Orthostatic hypotension and paroxysmal hypertension in humans with high spinal cord injury. Prog Brain Res. 2006;152:231–243. doi: 10.1016/S0079-6123(05)52015-6. [DOI] [PubMed] [Google Scholar]
- 104.Medicine CfSC Acute management of autonomic dysreflexia: individuals with spinal cord injury presenting to health-care facilities. Paralyzed Veterans of America; 2001. [PubMed] [Google Scholar]
- 105.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 106.Jellinger PS, Handelsman Y, Rosenblit PD et al. American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Dysplipidemia and Prevention of Cardiovasuclar Disease. Endocr Pract. 2017;23(s2):1–87. doi: 10.4158/EP171764.APPGL. [DOI] [PubMed] [Google Scholar]
- 107.Nash MS, Tractenberg RE, Mendez AJ et al. Cardiometabolic Syndrome in People with Spinal Cord Injury/Disease: Guideline-derived and Non-Guideline Risk Components in a Pooled Sample. Arch Phys Med Rehabil. 2016 doi: 10.1016/j.apmr.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 108.Arya R, Lehman D, Hunt KJ et al. Evidence for bivariate linkage of obesity and HDL-C levels in the Framingham Heart Study. BMC genetics. 2003;4(1):S52. doi: 10.1186/1471-2156-4-S1-S52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ford ES, Williamson DF, Liu S. Weight change and diabetes incidence: findings from a national cohort of U.S. adults. Am J Epidemiol. 1997;146(3):214–222. doi: 10.1093/oxfordjournals.aje.a009256. [DOI] [PubMed] [Google Scholar]
- 110.Resnick HE, Valsania P, Halter JB, Lin X. Relation of weight gain and weight loss on subsequent diabetes risk in overweight adults. J Epidemiol Community Health. 2000;54(8):596–602. doi: 10.1136/jech.54.8.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Barter PJ. Management of low HDL cholesterol. Aust Fam Physician. 1995;24(11):2066–2069. [PubMed] [Google Scholar]
- 112.Barter P, Gotto AM, LaRosa JC et al. HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. New Engl J Med. 2007;357(13):1301–1310. doi: 10.1056/NEJMoa064278. [DOI] [PubMed] [Google Scholar]
- 113.Modlesky CM, Bickel CS, Slade JM, Meyer RA, Cureton KJ, Dudley GA. Assessment of skeletal muscle mass in men with spinal cord injury using dual-energy X-ray absorptiometry and magnetic resonance imaging. J Appl Physiol. 2004;96(2):561–565. doi: 10.1152/japplphysiol.00207.2003. [DOI] [PubMed] [Google Scholar]
- 114.Jones L, Goulding A, Gerrard D. DEXA: a practical and accurate tool to demonstrate total and regional bone loss, lean tissue loss and fat mass gain in paraplegia. Spinal Cord. 1998;36(9):637–640. doi: 10.1038/sj.sc.3100664. [DOI] [PubMed] [Google Scholar]
- 115.Nuhlicek D, Spurr G, Barboriak J, Rooney C, El Ghatit A, Bongard R. Body composition of patients with spinal cord injury. Eur J Clin Nutr. 1988;42(9):765–773. [PubMed] [Google Scholar]
- 116.Castro MJ, Apple DF, Hillegass EA, Dudley GA. Influence of complete spinal cord injury on skeletal muscle cross-sectional area within the first 6 months of injury. Eur J Appl Physiol Occup Physiol. 1999;80(4):373–378. doi: 10.1007/s004210050606. [DOI] [PubMed] [Google Scholar]
- 117.Stjernberg L, Blumberg H, Wallin BG. Sympathetic activity in man after spinal cord injury. Outflow to muscle below the lesion. Brain. 1986;109(Pt 4):695–715. doi: 10.1093/brain/109.4.695. [DOI] [PubMed] [Google Scholar]
- 118.Monroe MB, Tataranni PA, Pratley R, Manore MM, Skinner JS, Ravussin E. Lower daily energy expenditure as measured by a respiratory chamber in subjects with spinal cord injury compared with control subjects. Am J Clin Nutr. 1998;68(6):1223–1227. doi: 10.1093/ajcn/68.6.1223. [DOI] [PubMed] [Google Scholar]
- 119.Bauman WA, Spungen AM, Wang J, Pierson RN., Jr The relationship between energy expenditure and lean tissue in monozygotic twins discordant for spinal cord injury. J Rehabil Res Dev. 2004;41(1):1. doi: 10.1682/jrrd.2004.01.0001. [DOI] [PubMed] [Google Scholar]
- 120.Buchholz AC, Pencharz PB. Energy expenditure in chronic spinal cord injury. Curr Opin Clin Nutr Metab Care. 2004;7(6):635–639. doi: 10.1097/00075197-200411000-00008. [DOI] [PubMed] [Google Scholar]
- 121.Maki K, Briones E, Langbein W et al. Associations between serum lipids and indicators of adiposity in men with spinal cord injury. Paraplegia. 1995;33(2):102–109. doi: 10.1038/sc.1995.24. [DOI] [PubMed] [Google Scholar]
- 122.Edwards LA, Bugaresti JM, Buchholz AC. Visceral adipose tissue and the ratio of visceral to subcutaneous adipose tissue are greater in adults with than in those without spinal cord injury, despite matching waist circumferences. Am J Clin Nutr. 2008;87(3):600–607. doi: 10.1093/ajcn/87.3.600. [DOI] [PubMed] [Google Scholar]
- 123.Jones LM, Legge M, Goulding A. Healthy body mass index values often underestimate body fat in men with spinal cord injury. Arch Phys Med Rehabil. 2003;84(7):1068–1071. doi: 10.1016/s0003-9993(03)00045-5. [DOI] [PubMed] [Google Scholar]
- 124.George C, Wells C, Dugan N. Validity of hydrodensitometry for determination of body composition in spinal injured subjects. Hum Bio. 1988:771–780. [PubMed] [Google Scholar]
- 125.Spungen AM, Adkins RH, Stewart CA et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol. 2003;95(6):2398–2407. doi: 10.1152/japplphysiol.00729.2002. [DOI] [PubMed] [Google Scholar]
- 126.Crane DA, Little JW, Burns SP. Weight gain following spinal cord injury: a pilot study. J Spinal Cord Med. 2011;34(2):227–232. doi: 10.1179/2045772311Y.0000000001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Boninger ML, Dicianno BE, Cooper RA, Towers JD, Koontz AM, Souza AL. Shoulder magnetic resonance imaging abnormalities, wheelchair propulsion, and gender. Arch Phys Med Rehabil. 2003;84(11):1615–1620. doi: 10.1053/s0003-9993(03)00282-x. [DOI] [PubMed] [Google Scholar]
- 128.Ballinger DA, Rintala DH, Hart KA. The relation of shoulder pain and range-of-motion problems to functional limitations, disability, and perceived health of men with spinal cord injury: a multifaceted longitudinal study. Arch Phys Med Rehabil. 2000;81(12):1575–1581. doi: 10.1053/apmr.2000.18216. [DOI] [PubMed] [Google Scholar]
- 129.Gellman H, Sib I, Waters RL. Late complications of the weight-bearing upper extremity in the paraplegic patient. Clin Orthop Relat R. 1988;233:132–135. [PubMed] [Google Scholar]
- 130.Cardinal BJ, Kosma M, McCubbin JA. Factors influencing the exercise behavior of adults with physical disabilities. Med Sci Sport Exer. 2004;36(5):868–875. doi: 10.1249/01.mss.0000126568.63402.22. [DOI] [PubMed] [Google Scholar]
- 131.Kehn M, Kroll T. Staying physically active after spinal cord injury: a qualitative exploration of barriers and facilitators to exercise participation. Bmc Public Health. 2009;9(1):168. doi: 10.1186/1471-2458-9-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.The Diabetes Prevention Program Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1999;22(4):623–634. doi: 10.2337/diacare.22.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Steinberg D, Bennett GG, Svetkey L. The DASH diet, 20 years later. J Am Med Assoc. 2017;317(15):1529–1530. doi: 10.1001/jama.2017.1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Banerjea R, Sambamoorthi U, Weaver F, Maney M, Pogach LM, Findley T. Risk of stroke, heart attack, and diabetes complications among veterans with spinal cord injury. Arch Phys Med Rehabil. 2008;89(8):1448–1453. doi: 10.1016/j.apmr.2007.12.047. [DOI] [PubMed] [Google Scholar]
- 136.Anson C, Shepherd C. Incidence of secondary complications in spinal cord injury. Int J Rehabil Res. 1996;19(1):55–66. doi: 10.1097/00004356-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 137.Yekutiel M, Brooks M, Ohry A, Yarom J, Carel R. The prevalence of hypertension, ischaemic heart disease and diabetes in traumatic spinal cord injured patients and amputees. Spinal Cord. 1989;27(1):58–62. doi: 10.1038/sc.1989.9. [DOI] [PubMed] [Google Scholar]
- 138.Bauman WA, Zhong YG, Schwartz E. Vitamin D deficiency in veterans with chronic spinal cord injury. Metabolism. 1995;44(12):1612–1616. doi: 10.1016/0026-0495(95)90083-7. [DOI] [PubMed] [Google Scholar]
- 139.McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil. 1999;80(11):1402–1410. doi: 10.1016/s0003-9993(99)90251-4. [DOI] [PubMed] [Google Scholar]
- 140.Nemunaitis GA, Mejia M, Nagy JA, Johnson T, Chae J, Roach MJ. A descriptive study on vitamin D levels in individuals with spinal cord injury in an acute inpatient rehabilitation setting. PM R. 2010;2(3):202–208. doi: 10.1016/j.pmrj.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 141.Barber D FD, Rogers S. The importance of nutrition in the care of persons with spinal cord injury. J Spinal Cord Med. 2003;26(2):122–123. doi: 10.1080/10790268.2003.11753670. [DOI] [PubMed] [Google Scholar]
- 142.Alexander LR, Spungen AM, Liu MH, Losada M, Bauman WA. Resting metabolic rate in subjects with paraplegia: the effect of pressure sores. Arch Phys Med Rehabil. 1995;76(9):819–822. doi: 10.1016/s0003-9993(95)80545-1. [DOI] [PubMed] [Google Scholar]
- 143.Levine AM, Nash MS, Green BA, Shea JD, Aronica MJ. An examination of dietary intakes and nutritional status of chronic healthy spinal cord injured individuals. Paraplegia. 1992;30(12):880–889. doi: 10.1038/sc.1992.165. [DOI] [PubMed] [Google Scholar]
- 144.Peiffer SC, Blust P, Leyson JF. Nutritional assessment of the spinal cord injured patient. J Am Diet Assoc. 1981;78(5):501–505. [PubMed] [Google Scholar]
- 145.Chen Y, Henson S, Jackson A, Richards J. Obesity intervention in persons with spinal cord injury. Spinal Cord. 2006;44(2):82–91. doi: 10.1038/sj.sc.3101818. [DOI] [PubMed] [Google Scholar]
- 146.Weinsier R, Bacon J, Birch R. Time-calorie displacement diet for weight control: a prospective evaluation of its adequacy for maintaining normal nutritional status. Int J Obes. 1982;7(6):539–548. [PubMed] [Google Scholar]
- 147.Cowan RE, Nash MS, Anderson-Erisman K. Perceived exercise barriers and odds of exercise participation among persons with SCI living in high-income households. Top Spinal Cord Inj Rehabil. 2012;18(2):126–127. doi: 10.1310/sci1802-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Jacobs PL, Nash MS, Rusinowski JW. Circuit training provides cardiorespiratory and strength benefits in persons with paraplegia. Med Sci Sports Exerc. 2001;33(5):711–717. doi: 10.1097/00005768-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 149.Nash MS, van de Ven I, van Elk N, Johnson BM. Effects of circuit resistance training on fitness attributes and upper-extremity pain in middle-aged men with paraplegia. Arch Phys Med Rehabil. 2007;88(1):70–75. doi: 10.1016/j.apmr.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 150.Hicks A, Ginis KM, Pelletier C, Ditor D, Foulon B, Wolfe D. The effects of exercise training on physical capacity, strength, body composition and functional performance among adults with spinal cord injury: a systematic review. Spinal Cord. 2011;49(11):1103–1127. doi: 10.1038/sc.2011.62. [DOI] [PubMed] [Google Scholar]
- 151.Nash M. Exercise reconditioning of the heart and peripheral circulation after spinal cord injury. Top Spinal Cord Inj Rehabil. 1998;3:1–15. [Google Scholar]
- 152.Cowan RE, Nash MS. Cardiovascular disease, SCI and exercise: unique risks and focused countermeasures. Disabil Rehabil. 2010;32(26):2228–2236. doi: 10.3109/09638288.2010.491579. [DOI] [PubMed] [Google Scholar]
- 153.Cowan RE, Malone LA, Nash MS. Exercise is Medicine™: Exercise Prescription After SCI to Manage Cardiovascular Disease Risk Factors. Top Spinal Cord Inj Rehabil. 2009;14(3):69–83. [Google Scholar]
- 154.Nash MS, Cowan R. E. Cardiovascular disease, SCI and exercise: unique risks and focused countermeasures. Vol 32 doi: 10.3109/09638288.2010.491579. 2010/06/08 ed2010. [DOI] [PubMed] [Google Scholar]
- 155.Pedersen BK, Saltin B. Exercise as medicine–evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25(S3):1–72. doi: 10.1111/sms.12581. [DOI] [PubMed] [Google Scholar]
- 156.Ginis KM, Hicks A, Latimer A et al. The development of evidence-informed physical activity guidelines for adults with spinal cord injury. Spinal Cord. 2011;49(11):1088–1096. doi: 10.1038/sc.2011.63. [DOI] [PubMed] [Google Scholar]
- 157.Medicine ACoS ACSM's guidelines for exercise testing and prescription. Lippincott Williams & Wilkins; 2013. [DOI] [PubMed] [Google Scholar]
- 158.Vetter ML, Faulconbridge LF, Webb VL, Wadden TA. Behavioral and pharmacologic therapies for obesity. Nat Rev Endocrinol. 2010;6(10):578–588. doi: 10.1038/nrendo.2010.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Rossner S, Sjostrom L, Noack R, Meinders E, Noseda G. Weight loss, weight maintenance, and improved cardiovascular risk factors after 2 years treatment with orlistat for obesity. Obes Res. 2000 doi: 10.1038/oby.2000.8. [DOI] [PubMed] [Google Scholar]
- 160.Torgerson JS, Hauptman J, Boldrin MN, Sjöström L. Xenical in the prevention of diabetes in obese subjects (XENDOS) study. Diabetes Care. 2004;27(1):155–161. doi: 10.2337/diacare.27.1.155. [DOI] [PubMed] [Google Scholar]
- 161.Ioannides-Demos LL, Proietto J, Tonkin AM, McNeil JJ. Safety of drug therapies used for weight loss and treatment of obesity. Drug Saf. 2006;29(4):277–302. doi: 10.2165/00002018-200629040-00001. [DOI] [PubMed] [Google Scholar]
- 162.Rucker D, Padwal R, Li SK, Curioni C, Lau DC. Long term pharmacotherapy for obesity and overweight: updated meta-analysis. BMJ. 2007 doi: 10.1136/bmj.39385.413113.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Garvey WT, Ryan DH, Look M et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. The Am J Clin Nutr. 2012;95(2):297–308. doi: 10.3945/ajcn.111.024927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Allison DB, Gadde KM, Garvey WT et al. Controlled-release phentermine/topiramate in severely obese adults: a randomized controlled trial (EQUIP) Obesity. 2012;20(2):330–342. doi: 10.1038/oby.2011.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Rothman RB, Hendricks EJ. Phentermine cardiovascular safety. Am J Emerg Med. 2009;27(8):1010–1013. doi: 10.1016/j.ajem.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 166.Kang J, Park CY, Kang J, Park YW, Park S. Randomized controlled trial to investigate the effects of a newly developed formulation of phentermine diffuse-controlled release for obesity. Diabetes Obes Metab. 2010;12(10):876–882. doi: 10.1111/j.1463-1326.2010.01242.x. [DOI] [PubMed] [Google Scholar]
- 167.Greenway FL, Fujioka K, Plodkowski RA et al. Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-I): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet. 2010;376(9741):595–605. doi: 10.1016/S0140-6736(10)60888-4. [DOI] [PubMed] [Google Scholar]
- 168.Wadden TA, Foreyt JP, Foster GD et al. Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modification: the COR-BMOD trial. Obesity. 2011;19(1):110–120. doi: 10.1038/oby.2010.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Thomsen WJ, Grottick AJ, Menzaghi F et al. Lorcaserin, a novel selective human hydroxytryptamine 2C agonist: in vitro and in vivo pharmacological characterization. J Pharmacol Exper Ther. 2008;325(2):577–587. doi: 10.1124/jpet.107.133348. [DOI] [PubMed] [Google Scholar]
- 170.Gustafson A, King C, Rey JA. Lorcaserin (Belviq): A selective serotonin 5-HT2C agonist in the treatment of obesity. Pharmacy and Therapeutics. 2013;38(9):525. [PMC free article] [PubMed] [Google Scholar]
- 171.Garber AJ, Abrahamson MJ, Barzilay JI et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm–2016 executive summary. Endocr Pract. 2016;22(1):84–113. doi: 10.4158/EP151126.CS. [DOI] [PubMed] [Google Scholar]
- 172.Chamberlain JJ, Herman WH, Leal S et al. Pharmacologic Therapy for Type 2 Diabetes: Synopsis of the 2017 American Diabetes Association Standards of Medical Care in Diabetes Pharmacologic Therapy for Type 2 Diabetes. Ann Intern Med. 2017;166(8):572–578. doi: 10.7326/M16-2937. [DOI] [PubMed] [Google Scholar]
- 173.Finnie A, Buchholz A, Ginis KM. Current coronary heart disease risk assessment tools may underestimate risk in community-dwelling persons with chronic spinal cord injury. Spinal Cord. 2008;46(9):608–615. doi: 10.1038/sc.2008.21. [DOI] [PubMed] [Google Scholar]
- 174.Ellenbroek D, Kressler J, Cowan RE, Burns PA, Mendez AJ, Nash MS. Effects of prandial challenge on triglyceridemia, glycemia, and pro-inflammatory activity in persons with chronic paraplegia. J Spinal Cord Med. 2015;38(4):468–475. doi: 10.1179/2045772314Y.0000000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Nash MS, DeGroot J, Martinez-Arizala A, Mendez AJ. Evidence for an exaggerated postprandial lipemia in chronic paraplegia. J Spinal Cord Med. 2005;28(4):320–325. doi: 10.1080/10790268.2005.11753827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Chopra AS, Miyatani M, Craven BC. Cardiovascular disease risk in individuals with chronic spinal cord injury: Prevalence of untreated risk factors and poor adherence to treatment guidelines. J Spinal Cord Med. 2016:1–8. doi: 10.1080/10790268.2016.1140390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Lieberman JA, Hammond FM, Barringer TA et al. Comparison of coronary artery calcification scores and National Cholesterol Education program guidelines for coronary heart disease risk assessment and treatment paradigms in individuals with chronic traumatic spinal cord injury. J Spinal Cord Med. 2011;34(2):233. doi: 10.1179/107902611X13019162562548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Lieberman JA, Hammond FM, Barringer TA et al. Adherence with the National Cholesterol Education Program guidelines in men with chronic spinal cord injury. J Spinal Cord Med. 2011;34(1):28–34. doi: 10.1179/107902610x12883422813589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Nash MS, Jacobs PL, Mendez AJ, Goldberg RB. Circuit resistance training improves the atherogenic lipid profile in persons with chronic paraplegia. J Spinal Cord Med. 2001 doi: 10.1080/10790268.2001.11753548. [DOI] [PubMed] [Google Scholar]
- 180.Yusuf S, Bosch J, Dagenais G et al. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. New Engl J Med. 2016;374(21):2021–2031. doi: 10.1056/NEJMoa1600176. [DOI] [PubMed] [Google Scholar]
- 181.Ridker PM, Danielson E, Fonseca F et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. New Engl J Med. 2008;359(21):2195. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 182.Stillman M, Aston C, Rabadi M. Mortality benefit of statin use in traumatic spinal cord injury: a retrospective analysis. Spinal Cord. 2016;54(4):298–302. doi: 10.1038/sc.2015.180. [DOI] [PubMed] [Google Scholar]
- 183.Nash MS, Lewis JE, Dyson-Hudson TA et al. Safety, tolerance, and efficacy of extended-release niacin monotherapy for treating dyslipidemia risks in persons with chronic tetraplegia: a randomized multicenter controlled trial. Arch Phys Med Rehabil. 2011;92(3):399–410. doi: 10.1016/j.apmr.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 184.James PA, Oparil S, Carter BL et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) J Am Med Assoc. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 185.Qaseem A, Wilt TJ, Rich R, Humphrey LL, Frost J, Forciea MA. Pharmacologic Treatment of Hypertension in Adults Aged 60 Years or Older to Higher Versus Lower Blood Pressure Targets: A Clinical Practice Guideline From the American College of Physicians and the American Academy of Family Physicians, Pharmacologic Treatment of Hypertension in Adults. Ann Intern Med. 2017;166(6):430–437. doi: 10.7326/M16-1785. [DOI] [PubMed] [Google Scholar]
- 186.Weber MA, Schiffrin EL, White WB et al. Clinical practice guidelines for the management of hypertension in the community. J Clin Hypertens. 2014;16(1):14–26. doi: 10.1111/jch.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Go AS, Bauman MA, King SMC et al. An effective approach to high blood pressure control. Hypertension. 2014;63(4):878–885. doi: 10.1161/HYP.0000000000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Alaedeen DI, Jasper J. Gastric bypass surgery in a paraplegic morbidly obese patient. Obes Surg. 2006;16(8):1107–1108. doi: 10.1381/096089206778026389. [DOI] [PubMed] [Google Scholar]
- 189.Williams GJ, Georgiou PA, Cocker DM, Bonanomi G, Smellie J, Efthimiou E. The safety and efficacy of bariatric surgery for obese wheelchair-bound patients. Ann R Coll Surg Engl. 2014;96(5):373–376. doi: 10.1308/003588414X13946184901083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Wong S, Barnes T, Coggrave M et al. Morbid obesity after spinal cord injury: an ailment not to be treated? Eur J Clin Nutr. 2013;67(9):998–999. doi: 10.1038/ejcn.2013.129. [DOI] [PubMed] [Google Scholar]
- 191.Fried M, Yumuk V, Oppert JM et al. Interdisciplinary European Guidelines on Metabolic and Bariatric Surgery. Obes Surg. 2014;24(1):42–55. doi: 10.1007/s11695-013-1079-8. [DOI] [PubMed] [Google Scholar]
- 192.Mechanick JI, Youdim A, Jones DB et al. Clinical Practice Guidelines for the Perioperative Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery Patient-2013 Update: Cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity. 2013;21:S1–S27. doi: 10.1002/oby.20461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Aminian A, Andalib A, Khorgami Z et al. Who should get extended thromboprophylaxis after bariatric surgery? A risk assessment tool to guide indications for post-discharge pharmacoprophylaxis. Ann Surg. 2017;265(1):143–150. doi: 10.1097/SLA.0000000000001686. [DOI] [PubMed] [Google Scholar]


