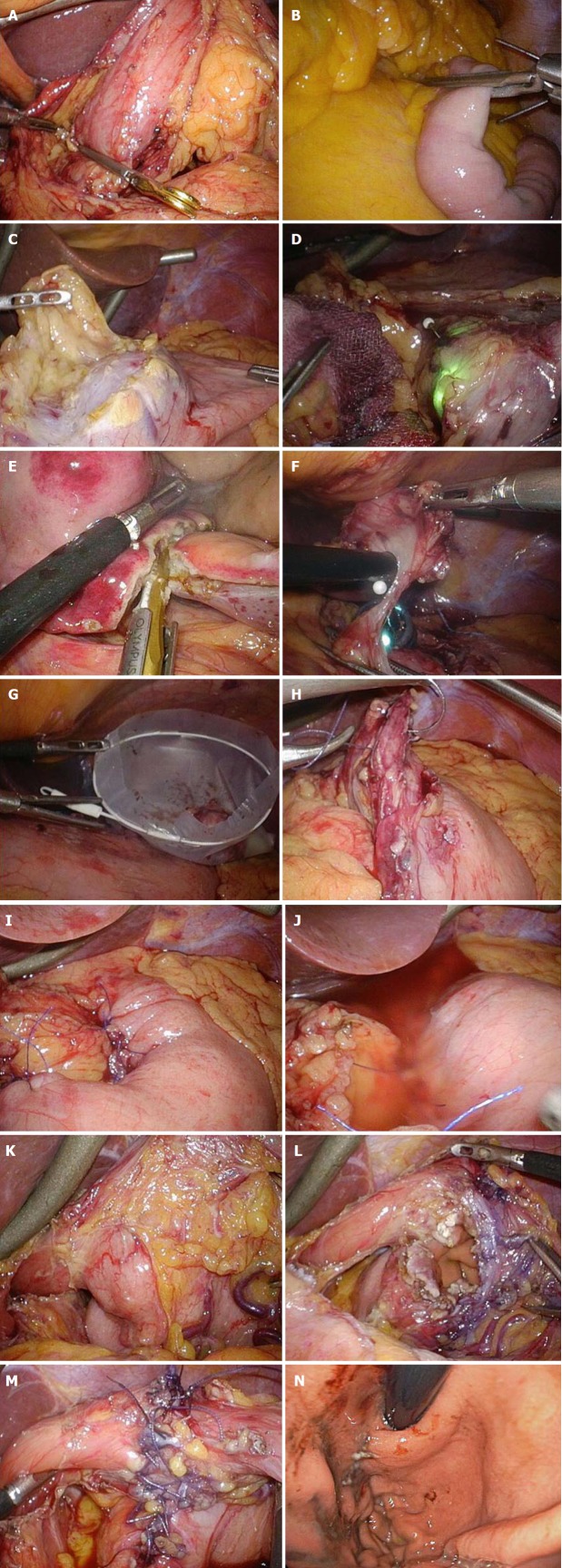
Figure 3.
Intraoperative laparoscopic view of laparoscopic and endoscopic cooperative surgery. A and B: Clamping of the (A) antrum or (B) jejunum should be performed using clamp forceps. This allows for adequate gastric expansion that provides an intraluminal working field for the endoscopic intervention; C: The surrounding fat tissue and vessels of the gastric wall are dissected, and the target wall is then mobilized to the ventral side; D: The laparoscopic surgeon should mobilize the gastric wall and prevent it from touching any surrounding organs for a safe intraluminal intervention. The pneumoperitoneal pressure and light intensity of laparoscopy are decreased to avoid disturbing the endoscopist; E: The laparoscopic surgeon can dissect the proximal gastric wall on behalf of the interventional endoscopist, if necessary; F: The surgeon and the endoscopist cooperate to complete the operation while avoiding injury to the adjacent organs; G: The resected specimen is placed in a plastic bag and removed intraluminally using endoscopy; H: The mucosal layer is closed with a running 4-0 absorbable suture thread; I: The seromuscular layer is closed with interrupted 3-0 absorbable sutures; J: A leak test is performed after suturing. K: This image depicts a case involving a tumor located in the posterior wall near the EGJ; The target gastric wall is turned as much as possible with a marginal free space established by carbon dioxide gas. The right side of the EGJ has enough working space laparoscopically; L: The defect of the gastric wall tends to become larger than many physicians expect; M: The defect in the gastric wall is closed with the laparoscopic hand-sewn technique in a layer-to-layer fashion; N: Intraluminal view after suturing. The absence of stenosis and malformation is confirmed. EGJ: Esophagogastric junction.