Abstract
Background
Alcoholic cirrhosis is an indication for 40% of liver transplantations (LT) in Europe. In most centers, 6 months of abstinence is required before listing. However, alcohol recidivism is quite high after LT, and approximately 20–25% of recipients with ALD resume harmful drinking, resulting in liver insufficiency, which casts doubt on the 6-months rule as a reliable marker of abstinence maintenance after LT.
Material/Methods
We analyzed data on patients who underwent orthotopic LT in Marie Curie Hospital, Szczecin, Poland, from 2000 to 2015 due to alcoholic or cryptogenic cirrhosis. Every ALD patient met the 6-month abstinence requirement. Alcohol recidivism has been studied based on a history of alcohol abuse taken from the patients or from their relatives, and in case of denial, on laboratory tests for alcohol abuse. Five patterns of recidivism were distinguished: death, constant heavy drinking, heavy drinking with abstinence attempts, occasional laps, and a single episode of alcohol intake. The analysis of survival was performed according to the Kaplan-Meier method. Patient survival rates in ALD recipients vs. non-ALD recipients were compared using the log-rank test.
Results
Alcohol recidivism was finally evaluated in 109 patients: 81 males and 28 females, with a median age of 53.3 years (range 30–66). Harmful drinking was discovered in 16 patients (14.7%), including seven deaths due to alcoholic hepatitis. Sporadic or episodic drinking was found in 29 patients (27%). In heavy drinkers, the abstinence period after transplantation was significantly shorter and patients were younger than the average (median age 43.8 years). Women break abstinence faster than men and are at greater risk of liver insufficiency. Five, 10 and 15-year survival in the ALD group was superior in comparison with non-ALD group, but differences did not reach statistical significance (p=0.066, p=0.063, p=0.075, respectively).
Conclusions
The prognostic value of a 6-month abstinence period before transplantation is rather low as it does not predict sobriety after transplantation. However, only a minority of such patients drink harmfully. Survival in ALD recipients tends to be better in comparison with survival in the other etiologies. Younger women dependent on alcohol shortly before LT are at greatest risk of recidivism.
MeSH Keywords: Liver Cirrhosis, Alcoholic; Liver Diseases, Alcoholic; Liver Transplantation
Background
Alcoholic liver disease (ALD) is a frequent indication for liver transplantation in Europe, accounting for approximately 40% of all liver transplants [1]. This indication, viewed as a self-inflicted disease, is a subject of many controversies and debates in light of limited organ resources, and never gained full acceptance. On one hand, in patients who abstain from alcohol after liver transplantation, 1- and 5-year survival does not differ from survival in other indications, and reaches 82–92% and 72–83%, respectively [2,3]. On the other hand, alcoholism is a life-long disease not cured by transplantation; therefore, the relapse rate after LT can be as high as 50% according to some reports, significantly impairing long-term outcomes and stimulating intense public debate on organ allocation to patients with self-induced injury [4,5]. Various criteria are being applied to improve patient selection before LT in order to minimize individual risk of relapse to heavy drinking. The most widely used are a pre-transplant abstinence period of 3–6 months, participation in special rehabilitation programs for alcohol-addicted persons, and regular consultations with a psychiatrist. The 6-month rule was adopted based on a report by Bird et al., showing the clearly better LT outcomes in LT patients who abstained for this period [6]. Soon after publication of that report, however, many contradictory results have been published questioning the reliability of the 6-month rule in selection of optimal patients for LT [7,8].
The most controversial indication for LT is alcoholic hepatitis in patients currently drinking alcohol or with a recent history of addiction. Mortality rates in this clinical syndrome are very high and exceed 50% in patients non-responsive to treatment with steroids and/or pentoxifylline. Because the need for LT arises from life-threatening conditions, a pre-transplant abstinence period of 6 months usually cannot be achieved, and alcoholic hepatitis is considered as a contraindication for LT in many centers. Nevertheless, in these circumstances, LT is the only life-saving option, with survival comparable to that of patients responding to conservative treatment and similar to survival rates of patients undergoing LT for alcoholic cirrhosis [9]. Alcohol recidivism is usually higher in patients with alcoholic hepatitis than in patients with non-active alcoholic cirrhosis, but, according to some authors, relapse to harmful drinking is nevertheless rather low and some institutions suggest considering LT in selected patients with alcoholic hepatitis; for example, those with a first episode of liver decompensation [10]. Another argument favoring LT in patients with severe alcoholic hepatitis without pre-transplant abstinence period is the generally low predictive value of a 6-month abstinence for alcohol recidivism.
The aim of the present study was to evaluate the efficacy of the 6-month abstinence period rule in patients transplanted for ALD in a single center.
Material and Methods
All patients who underwent liver transplantation (LT) for alcoholic liver disease and cryptogenic cirrhosis between 2000 and 2015 in Marie Curie Hospital of Szczecin, Poland, were enrolled into this study. The latter group was included due to unclear etiology of liver disease and the assumption that some cases of cirrhosis were in fact caused by excessive alcohol consumption in the past. A documented alcohol abstinence period of at least 6 months is required for listing for LT in our center, and every enrolled patient fulfilled this condition. To verify this, a blood sample was sporadically taken for alcohol measurement and patients had to document regular consultations with a psychiatrist or participation in special meetings for alcoholics in case of diagnosis of alcohol addiction. Additionally, worse lab test results, typical for people drinking alcohol, was taken into account. In case of alcohol relapse while on a waiting list, a patient was temporarily or permanently suspended from the procedure.
Post-transplant patients were carefully evaluated for alcohol intake in the follow-up period. They attended an outpatient clinic every week for the first month post-LT, every 2 weeks until 3 months, and every 4 weeks thereafter for the first year post-LT. In the following years, visits were scheduled at 3-month intervals. At every visit, a history of alcohol consumption was taken, laboratory tests were performed, and blood alcohol level was measured when necessary. Furthermore, in a few cases, a liver biopsy was performed to confirm suspicion of alcohol consumption.
Patterns of alcohol recidivism were classified into 5 categories:
– death due to liver decompensation in the course of alcoholic hepatitis;
– heavy and increasing drinking without abstinence attempts;
– heavy drinking with abstinence attempts and hospitalizations in psychiatric institutions;
– infrequent butt repeated episodes of alcohol consumption (slips);
– single episode of alcohol intake.
Relapse monitoring was based on 3 strategies: (1) patients’ statement on alcohol consumption; (2) reports from family members; (3) and/or laboratory tests diagnostic for ALD according to EASL guidelines, such as significant increase in gamma glutamyl transferase (GGT) activity, aspartate aminotransferase (AST) to alanine aminotransferase (ALT) ratio >2, mean corpuscular volume (MCV) >100 fl, increase in immune globulin A level above the upper limit of normal, and elevated triglycerides [11]. Alcohol quantification was sometimes performed.
Kaplan-Meier cumulative mortality in ALD recipients vs. non-ALD recipients was calculated and the statistical significance of survival data was analyzed and compared using the log-rank test. Unadjusted Cox proportional hazards models were used to assess the effect of liver disease etiology on the risk of death and to calculate the hazard ratios (HR). P values of 0.05 were considered significant.
Results
From 2000 to 2015, a total of 577 patients underwent LT: alcoholic cirrhosis was diagnosed in 103 patients, and in 39 cases no etiology of liver disease was recognized (cryptogenic cirrhosis). All but 3 patients with the diagnosis of alcoholic liver disease were consulted by a psychiatrist before listing. Three patients were transferred to the surgery department from different intensive care units and their general condition precluded proper abstinence assessment. Data on the length of abstinence were collected from the family, but such data might be highly inaccurate. In those cases, there was a high suspicion of alcohol dependence as well as alcoholic hepatitis in addition to liver cirrhosis. Alcohol abuse or distant alcohol dependence (diagnosis made not later than 1 year before listing) was diagnosed in 72 cases, and recent alcohol dependence was diagnosed in 28 cases; in the latter situation and in every case when indicated, patients had to attend special rehabilitation programs and to visit a psychiatrist regularly despite frequent non-acceptance of the diagnosis. Six months of abstinence was strictly required before listing. Table 1 shows the baseline etiology of liver disease.
Table 1.
The baseline etiology of liver disease.
| No. of transplantations performed in the Marie Curie Hospital in years 2000–2015 | No. of patients with alcoholic cirrhosis | No. of patients with presumable alcoholic hepatitis on top of alcoholic cirrhosis | No. of patients with cryptogenic cirrhosis |
|---|---|---|---|
| 577 | 100 | 3 | 39* |
Probable alcoholic etiology in 13 patients.
Among the 39 subjects diagnosed with cryptogenic cirrhosis, regular alcohol drinking after transplantation was recognized in 13 patients. This behavior strongly suggested an etiology of liver disease, which was obscure before transplantation due to inactive form of cirrhosis and inaccurate medical history. Alcoholic etiology of liver disease in transplant candidates was therefore considered in 116 cases. Seven patients died in the early post-transplant period (within first 30 days post-LT) and were excluded from the study. Finally, alcohol recidivism was evaluated in a group of 109 patients (81 males and 28 females), with a median age of 53.3 years (range 30–66). Table 2 shows alcohol recidivism patterns in the study group.
Table 2.
Patterns of alcohol recidivism.
| Pattern of recidivism | Patients, n (%) | Sex (male/female, n) | Average time from LT to breaking abstinence (in months), the whole group | Average time from LT to breaking abstinence (in months), males | Average time from LT to breaking abstinence (in months), females |
|---|---|---|---|---|---|
| Death due to alcoholic hepatitis | 8 (7.4) | 3/5 | 6 | 12 | 4 |
| Harmful and increasing drinking without any attempts of abstinence | 3 (2.7) | 3/0 | 20 | 20 | NA |
| Harmful drinking with periodical abstinence | 5 (4.6) | 3/2 | 9.6 | 13 | 4.5 |
| Slips | 22 (20.6) | 14/8 | 31.3 | 30.8 | 32.6 |
| Single episode of alcohol consumption | 7 (6.4) | 7/0 | 30.4 | 30.4 | NA |
| No alcohol consumption | 47 (43.1) | 40/7 | |||
| Lost from follow-up | 17 (15.6) | 11/6 | |||
| Together | 109 | 81/28 |
Harmful drinking, including 8 deaths due to alcoholic hepatitis, was observed in 16 (14.7%) patients, with a slight predominance of males. In all these patients, abnormal liver enzymes were noted, with the evidence of liver insufficiency (elevated bilirubin, low albumin level, and long prothrombin time). In 3 patients not accepting diagnosis and denying alcohol drinking, alcoholic liver damage was confirmed with a liver biopsy. The majority of relapsers (27%) drank occasionally or reported a single episode of alcohol intake. In these cases, increases in liver enzymes activity were noticed with return to normal values between peaks. No laboratory evidence of liver insufficiency was detected. The average time to relapse was 12 months (range 2–78 months). In case of harmful drinking, the abstinence period after transplantation was significantly shorter – 6 months in the group of patients who died, and 9.6 months in the harmfully drinking patients who were still alive – and patients were younger than the average (median age 43.8 years). It is worth noting, however, that women relapse from abstinence faster than men and are at greater risk of liver insufficiency while drinking alcohol. All cases of harmful drinking were noted in the group patients with recent alcohol dependence, including 2 out of 3 patients transferred for LT from an ICU.
Patients lost to follow-up (17 cases) were identified as alive with the use of the personal identity number. Most had probably they moved to another transplant center or had migrated. History of alcohol recidivism is not known in this group.
The estimated survival rate did not differ between ALD recipients and patients transplanted due to other etiologies in any time point, but it tended to be improved in the alcoholic group (Figure 1).
Figure 1.
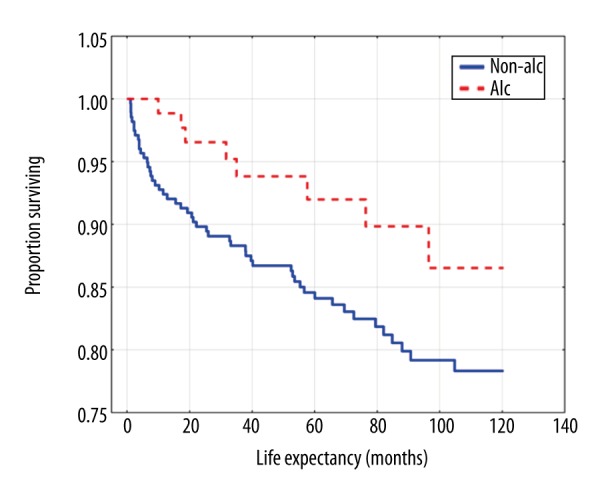
Kaplan-Meier estimates of survival according to the reason of transplantation (ALD vs. non-ALD recipients).
Discussion
End-stage liver disease of alcoholic etiology is the second most frequent indication for liver transplantation in Europe, with a good prognosis and survival, provided that there is no relapse of alcohol abuse. Therefore, the main task in the management of patients with ALD is to maintain abstinence after transplantation. Motivation for not drinking before transplantation is far stronger as abstinence is a strict criterion in most transplant centers to put a patient on a waiting list. The length of pre-transplant abstinence was, and still is, a matter of debate, but according to the recommendations of the United Network of Organ Sharing, a minimum 6-month period of abstinence from alcohol before LT has been accepted as a rule by the majority of transplant societies and national transplant organizations [12]. This length of abstinence is required to minimize the chance of alcohol recidivism after transplantation, as well as to stabilize the general condition of the patient and to rule-out alcoholic hepatitis as a reason of liver decompensation. It is extremely important due to the organ shortage and low social acceptance of graft allocation to people who continue drinking. However, selection of suitable candidates for transplantation according to the duration of the pre-transplant abstinence period as the most specific and important prognostic factor of post-transplant abstinence has been a subject of much criticism. Despite strict adherence to the 6-month abstinence period rule, relapse to post-transplantation drinking is remarkably high because the majority of liver recipients start to consume small or moderate amounts of alcohol, and approximately 20–25% resume heavy alcohol abuse, with subsequent liver damage [13]. Some authors suggest that the abstinence period should be longer than 6 months to guarantee better sobriety maintenance. Dom et al. showed that every month of abstinence before transplantation increased the probability of abstinence by 5% after the procedure [14]. Another argument against the 6-month rule is the necessity for more complex selection of transplant candidates with ALD, which is based on the abstinence period and on other prognostic factors such as general compliance, psychiatric diagnosis (alcohol dependence vs. harmful alcohol abuse), presence of concomitant psychiatric disorders with special attention to depression, access to rehabilitation programs for alcoholics, family support and social security, duration of pre-transplant alcohol drinking and daily amounts of alcohol, and a family history of alcoholism. Not denying the importance of better selection criteria for ALD patients, it seems unrealistic to apply all of them in a situation of life-threatening disease decompensation. Moreover, according to some authors, recidivism to harmful drinking connected with liver damage and graft loss is not very high and usually does not exceed 20%, which is similar to liver failure in some other recurrent diseases [15].
In our study, drinking alcohol was noted in 41.7% of patients transplanted due to confirmed or suspected ALD. Assuming that the patients who were lost to follow-up also drink, this percentage rises to 57.3. It is therefore evident that the prognostic value of a 6-month abstinence period before transplantation is rather low because it does not predict sobriety after transplantation. Prognosis of abstinence is much better when it is connected with the diagnosis of alcohol abuse but not alcohol dependence and the older age of recipients. It seems that the greatest risk of recidivism is in younger women dependent on alcohol before LT. They relapse to substance abuse much faster than men and tend to drink more harmfully. Selection for liver transplantation in women addicted to alcohol should be done with caution and some other prognostic factors (compliance, social support, exclusion of depression, regular surveillance by the psychiatrist) should be taken into account, in addition to a 6-month abstinence period
Conclusions
The prognostic value of a 6-month abstinence period before transplantation is rather low as it does not predict sobriety after transplantation. However, only a minority of such patients drink harmfully. Younger women dependent on alcohol shortly before LT are at greatest risk of recidivism.
Footnotes
Source of support: Departmental sources
References
- 1.Burra P, Senzolo M, Adam R, et al. Liver transplantation for alcoholic liver disease in Europe: A study from the ELTR (European Liver Transplant Registry) Am J Transplant. 2010;10:138–48. doi: 10.1111/j.1600-6143.2009.02869.x. [DOI] [PubMed] [Google Scholar]
- 2.De Gottardi A, Spahr L, Gelez P, et al. A simple score for predicting alcohol relapse after liver transplantation: results form 387 patients over 15 years. Arch Intern Med. 2007;167:1183–88. doi: 10.1001/archinte.167.11.1183. [DOI] [PubMed] [Google Scholar]
- 3.Pfitzmann R, Schwenzer J, Rayes N, et al. Long-term survival and predictors of relapse after orthotopic liver transplantation for alcoholic liver disease. Liver Transpl. 2007;13:197–205. doi: 10.1002/lt.20934. [DOI] [PubMed] [Google Scholar]
- 4.Lim JK, Keeffe EB. Liver transplantation for alcoholic liver disease: Current concepts and length of sobriety. Liver Transpl. 2004;10(Suppl 2):S31–38. doi: 10.1002/lt.20267. [DOI] [PubMed] [Google Scholar]
- 5.Dew MA, DiMartini AF, Steel J, et al. Meta-analysis of risk for relapse to substance use after transplantation of the liver or other solid organs. Liver Transpl. 2008;14:159–72. doi: 10.1002/lt.21278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bird GL, O’Grady JG, Harvey FA, et al. Liver transplantation in patients with alcoholic cirrhosis: selection criteria and rates of survival and relapse. BMJ. 1990;301:15–17. doi: 10.1136/bmj.301.6742.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mackie J, Groves K, Hoyle A, et al. Orthotopic liver transplantation for alcoholic liver disease: A retrospective analysis of survival, recidivism and risk factors predisposing to recidivism. Liver Transpl. 2001;7:418–27. doi: 10.1053/jlts.2001.23789. [DOI] [PubMed] [Google Scholar]
- 8.Egawa H, Nishimura K, Teramukai S, et al. Risk factors for alcohol relapse after liver transplantation for alcoholic cirrhosis in Japan. Liver Transpl. 2014;20:298–310. doi: 10.1002/lt.23797. [DOI] [PubMed] [Google Scholar]
- 9.Singal AK, Bashar H, Anand BS, et al. Outcomes after liver transplantation for alcoholic hepatitis are similar to alcoholic cirrhosis: Exploratory analysis form the UNOS database. Hepatology. 2012;55:1398–405. doi: 10.1002/hep.25544. [DOI] [PubMed] [Google Scholar]
- 10.Mathurin P, Moreno C, Samuel D, et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med. 2011;365:1790–800. doi: 10.1056/NEJMoa1105703. [DOI] [PubMed] [Google Scholar]
- 11.European Association for the Study of the Liver. EASL clinical practical guidelines: Management of alcoholic liver disease. J Hepatol. 2012;57:399–420. doi: 10.1016/j.jhep.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 12.Dimartini A, Trzepacz P. Alcoholism and organ transplantation. In: Dimartini A, Trzepacz P, editors. The transplant patient: Biological, psychiatric and ethical issues in organ transplantation. 1st ed. Cambridge, UK: Cambridge University Press; 2000. pp. 214–38. [Google Scholar]
- 13.Lucey MR. Liver transplantation in patients with alcoholic liver disease. Liver Transpl. 2011;17:751–59. doi: 10.1002/lt.22330. [DOI] [PubMed] [Google Scholar]
- 14.Dom G, Wojnar M, Crunelle CL, et al. Assessing and treating alcohol relapse risk in liver transplantation candidates. Alcohol Alcohol. 2015;50:164–72. doi: 10.1093/alcalc/agu096. [DOI] [PubMed] [Google Scholar]
- 15.Kawaguchi Y, Sugawara Y, Akamatsu N, et al. Perceprtions of post-transplant recidivism in liver transplantation for alcoholic liver disease. World J Hepatol. 2014;6:812–17. doi: 10.4254/wjh.v6.i11.812. [DOI] [PMC free article] [PubMed] [Google Scholar]


