Key Points
Question
Are changes in cardiovascular health associated with incident cardiovascular events?
Findings
In this prospective cohort study that included 9256 participants without cardiovascular disease (CVD), changes over 10 years in category of cardiovascular health, based on a composite metric, did not show a consistent association with incident CVD. For example, while increase from a moderate to a high category of cardiovascular health was associated with a significant hazard ratio of 0.39, decrease from a high to a low category of cardiovascular health was also associated with a significant hazard ratio of 0.49.
Meaning
This study did not find a consistent relationship between direction of change in category of a composite metric of cardiovascular health and risk of CVD.
Abstract
Importance
There is consistent evidence of the association between ideal cardiovascular health and lower incident cardiovascular disease (CVD); however, most studies used a single measure of cardiovascular health.
Objective
To examine how cardiovascular health changes over time and whether these changes are associated with incident CVD.
Design, Setting, and Participants
Prospective cohort study in a UK general community (Whitehall II), with examinations of cardiovascular health from 1985/1988 (baseline) and every 5 years thereafter until 2015/2016 and follow-up for incident CVD until March 2017.
Exposures
Using the 7 metrics of the American Heart Association (nonsmoking; and ideal levels of body mass index, physical activity, diet, blood pressure, fasting blood glucose, and total cholesterol), participants with 0 to 2, 3 to 4, and 5 to 7 ideal metrics were categorized as having low, moderate, and high cardiovascular health. Change in cardiovascular health over 10 years between 1985/1988 and 1997/1999 was considered.
Main Outcome and Measure
Incident CVD (coronary heart disease and stroke).
Results
The study population included 9256 participants without prior CVD (mean [SD] age at baseline, 44.8 [6.0] years; 2941 [32%] women), of whom 6326 had data about cardiovascular health change. Over a median follow-up of 18.9 years after 1997/1999, 1114 incident CVD events occurred. In multivariable analysis and compared with individuals with persistently low cardiovascular health (consistently low group, 13.5% of participants; CVD incident rate per 1000 person-years, 9.6 [95% CI, 8.4-10.9]), there was no significant association with CVD risk in the low to moderate group (6.8% of participants; absolute rate difference per 1000 person-years, −1.9 [95% CI, −3.9 to 0.1]; HR, 0.84 [95% CI, 0.66-1.08]), the low to high group, (0.3% of participants; absolute rate difference per 1000 person-years, −7.7 [95% CI, −11.5 to −3.9]; HR, 0.19 [95% CI, 0.03-1.35]), and the moderate to low group (18.0% of participants; absolute rate difference per 1000 person-years, −1.3 [95% CI, −3.0 to 0.3]; HR, 0.96 [95% CI, 0.80-1.15]). A lower CVD risk was observed in the consistently moderate group (38.9% of participants; absolute rate difference per 1000 person-years, −4.2 [95% CI, −5.5 to −2.8]; HR, 0.62 [95% CI, 0.53-0.74]), the moderate to high group (5.8% of participants; absolute rate difference per 1000 person-years, −6.4 [95% CI, −8.0 to −4.7]; HR, 0.39 [95% CI, 0.27-0.56]), the high to low group (1.9% of participants; absolute rate difference per 1000 person-years, −5.3 [95% CI, −7.8 to −2.8]; HR, 0.49 [95% CI, 0.29-0.83]), the high to moderate group (9.3% of participants; absolute rate difference per 1000 person-years, −4.5 [95% CI, −6.2 to −2.9]; HR, 0.66 [95% CI, 0.51-0.85]), and the consistently high group (5.5% of participants; absolute rate difference per 1000 person-years, −5.6 [95% CI, −7.4 to −3.9]; HR, 0.57 [95% CI, 0.40-0.80]).
Conclusions and Relevance
Among a group of participants without CVD who received follow-up over a median 18.9 years, there was no consistent relationship between direction of change in category of a composite metric of cardiovascular health and risk of CVD.
This cohort study uses UK Whitehall II study data to characterize changes in cardiovascular risk factors over 10 years and associations between change in risk and incident cardiovascular events among people without baseline cardiovascular disease.
Introduction
Primordial prevention, ie, preventing the development of risk factors before they emerge, is increasingly emphasized as a complementary prevention strategy for cardiovascular disease (CVD).1 To this end, the American Heart Association (AHA) developed a simple 7-item tool consisting of 4 behavioral metrics (nonsmoking, and ideal levels of body weight, physical activity, and diet) and 3 biological metrics (ideal levels of untreated blood pressure, fasting blood glucose, and total cholesterol) for promoting ideal cardiovascular health.
Recent studies and meta-analyses2,3 have consistently reported substantial benefit of high cardiovascular health and having higher ideal metrics for incident CVD events and mortality. Despite their prospective nature, most but not all4 previous studies used a single assessment of cardiovascular health. Whether cardiovascular health changes over time and how these changes are related to incident CVD and mortality is largely unknown.5
Using serial examinations of the Whitehall II study,6 the aims of the present study were the following: (1) to quantify the association of time-varying cardiovascular health during follow-up with incident CVD events, all-cause mortality, and cause-specific mortality; (2) to describe change in cardiovascular health over 10 years; and (3) to quantify the association of change in cardiovascular health with subsequent incident CVD and mortality.
Methods
Participants
The Whitehall II study is an ongoing prospective cohort study originally employed by the British civil service in London-based offices.6 A total of 10 308 participants (6895 men and 3413 women; aged 35-55 years) were recruited between 1985 and 1988, during which time they underwent a clinical examination and provided responses on a self-administered questionnaire. Subsequent uniform, structured clinical examinations, consisting of measures of anthropometry, cardiovascular and metabolic risk factors, and self-administrated questionnaires were completed approximately every 5 years (1991/1993, 1997/1999, 2002/2004, 2007/2009, 2012/2013, and 2015/2016). Participant consent and research ethics approvals (University College London [UCL] ethics committee) were renewed at each contact; the latest approval was by the Joint UCL/UCLH Committee on the Ethics of Human Research.
Cardiovascular Health Metrics and Status
The AHA criteria were used to define the 7 metrics of cardiovascular health at all waves (eTable 1 in the Supplement).1 Cardiovascular health status was then categorized as high, moderate, or low to reflect 5 to 7, 3 to 4, and 0 to 2 metrics at ideal level.2,3 A continuous 14-point cardiovascular health score assigning 0 points for poor metrics, 1 point for intermediate metrics, and 2 points for ideal metrics was also calculated.
Change in cardiovascular health was examined between 1985/1988 and 1997/1999 in participants having the 7 metrics at both time points. For participants with at least 1 missing cardiovascular health metric in 1997/1999, change in cardiovascular health was estimated between 1985/1988 and 1991/1993. All participants were required to be free of CVD event between 1985/1988 and 1997/1999 examinations.
Covariates
Sociodemographic variables included age, sex, race/ethnicity (white, nonwhite), marital status (married/cohabiting, other), socioeconomic status (assessed by occupational position and based on income and work status: high, intermediate, and low), and education (less than primary school [aged <11 years], lower secondary school [aged <16 years], higher secondary school [aged <18 years], university, and higher university degree). Race/ethnicity was self-reported (fixed categories) and collected to study race/ethnicity disparities in health. Depressive symptoms were ascertained using the 30-item General Health Questionnaire.7 Family history of myocardial infarction or stroke in either parent or in a sibling was reported by participants at each wave.
Outcomes
The primary outcome was incident CVD (coronary heart disease and stroke combined), and the secondary outcome was mortality. CVD follow-up was until March 31, 2017, and mortality follow-up was until August 31, 2017.
Coronary heart disease was ascertained by the following study-specific assessments: electrocardiogram recording (coded using the Minnesota system), self-reported coronary heart disease (verified in medical records), and linkage to the Hospital Episodes Statistics database (International Classification of Diseases, Ninth Revision [ICD-9] codes 410-414, ICD-10 codes I20-I25, or ICD-10 procedures K40-K49, K50, K75, U19). Hospital Episodes Statistics is a national database that contains information on inpatient and outpatient care.8,9 The ascertainment included nonfatal myocardial infarction, definite angina, reported coronary artery bypass grafting, and percutaneous transluminal coronary angioplasty.
Stroke was assessed using the World Health Organization Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA)-Augsburg stroke questionnaires, which capture symptoms associated with events, even if the participant did not report having had a diagnosis of stroke. These reports were corroborated in the Hospital Episodes Statistics database (ICD-9 codes 430, 431, 434, 436 and ICD-10 codes I60-I64). The ascertainment included transient ischemic attack, ischemic stroke, and hemorrhagic stroke.9,10
Mortality data came from linkage to the British National Mortality Register. We examined deaths due to cardiovascular-related causes (ICD-9 codes 390-459 and ICD-10 codes I00-I99) and cancer-related causes (ICD-9 codes 140-208 and ICD-10 codes C00-C97).
Statistical Analysis
The 2 steps of analyses for this study are summarized in eFigure 1 in the Supplement.
Time-Varying Analysis
Cardiovascular health status, the number of ideal metrics (range, 0-7), and the 14-point cardiovascular health score between 1985/1988 and 2015/2016 were used as time-varying variables in Cox proportional hazard regression. At each date of an event (CVD or death), the model used the cardiovascular health exposure present at the visit just before the event. In case of missing cardiovascular health exposure, the last carried forward approach was used. Coronary heart disease and stroke were investigated as a combined CVD end point but also as separate outcomes. For the 141 participants who had coronary heart disease and a stroke, follow-up was censored at the date of first event. When investigating associations of cardiovascular health exposures with cause-specific mortality, competing risk analysis with the Fine and Gray method11 was used and subdistribution hazard ratios (HRs) were estimated.
Change in Cardiovascular Health Between 1985/1988 and 1997/1999 and Subsequent Outcomes
Change in cardiovascular health categories yielded 9 possible combinations of cardiovascular health status: consistently low, consistently moderate, consistently high, low to moderate, low to high, moderate to high, high to low, high to moderate, and moderate to low cardiovascular health. In these analyses, follow-up for CVD and mortality started from the 1997/1999 examination. Kaplan-Meier curves of incident CVD events and all-cause mortality across combinations of change in cardiovascular health were compared with the log-rank test using time in study as the time scale. The HRs of CVD and all-cause mortality for each combination of cardiovascular health change were computed in Cox models using the consistently low cardiovascular health group as the reference category. The HRs per unit of change in the number of ideal metrics and in the 14-point cardiovascular health score were also estimated.
All Cox models (ie, the time-varying models and the models with cardiovascular health change) used age as the time scale and were stratified by year of birth (5-year intervals) to account for birth cohort effects. In addition, all models were adjusted for baseline covariates (sex, race/ethnicity, education, occupation, depression, family history of CVD), and baseline number of ideal metrics or cardiovascular health score as appropriate. Depression was accounted for as a confounding factor because individuals with depression have lower cardiovascular health12,13 and a higher CVD risk.14 However, to address the potential for depression to lie on the causal pathway to CVD, post hoc analyses were also conducted that removed depression as a covariate. The proportional hazard assumption was assessed by visual inspection of the survival curves and the Kolmogorov test. The linearity assumption for the models with the number of ideal metrics and the 14-point cardiovascular health score as continuous exposures was assessed by comparing the Akaike information criterion of linear models with models including quadratic and cubic terms.
Sensitivity Analyses
The analysis was repeated with 4 groups of cardiovascular health change, as used in the Framingham Offspring Study,4 using the 14-point cardiovascular health score: consistently high (≥8 to ≥8), high to low (≥8 to ≤7), low to high (≤7 to ≥8), and consistently low (≤7 to ≤7). Change in the number of ideal metrics between 1985/1988 and 1997/1999 as the exposure was evaluated in the Cox analysis using those with no change as the reference category. Also, missing cardiovascular health metrics and covariates were imputed by multiple imputation (using fully conditional specification method under SAS MI procedure, n = 10 imputations). In addition, the associations between time-varying and change in the individual cardiovascular health metrics with outcomes were investigated.
Statistical analyses were performed using SAS version 9.4.
Results
The study population included 9256 participants free of CVD who had data on all 7 cardiovascular health metrics at baseline. Their mean (SD) age was 44.8 (6.0) years, and 32% were women (Table 1). The 1052 participants excluded at baseline had a poorer sociodemographic and cardiovascular risk profile (eTable 2 in the Supplement).
Table 1. Characteristics and Cardiovascular Health Status at Baseline and Follow-up, 1985/1988 to 2015/2016a.
| Characteristics | Examination Round | ||||||
|---|---|---|---|---|---|---|---|
| 1985/1988 (n = 9256) |
1991/1993 (n = 8972) |
1997/1999 (n = 8539) |
2002/2004 (n = 8014) |
2007/2009 (n = 7363) |
2012/2013 (n = 6795) |
2015/2016 (n = 6334) |
|
| Age, mean (SD), y | 44.8 (6.0) | 50.0 (6.1) | 55.7 (6.0) | 60.9 (5.9) | 65.6 (5.9) | 69.5 (5.8) | 72.4 (5.7) |
| Women | 2941 (31.8) | ||||||
| Depressionb | 1272 (13.7) | 1300 (14.5) | 1275 (14.9) | 1194 (14.9) | 983 (13.4) | 942 (13.9) | 840 (13.3) |
| Education level | |||||||
| High school | 2368 (25.6) | ||||||
| College | 1744 (18.8) | ||||||
| Tertiary | 2933 (31.7) | ||||||
| Occupation | |||||||
| Administrative | 2791 (30.2) | 3271 (36.5) | 3254 (38.1) | 3144 (39.2) | 2925 (39.7) | 2743 (40.4) | 2580 (40.7) |
| Professional/executive | 4538 (49.0) | 4059 (45.2) | 3762 (44.1) | 3492 (43.6) | 3190 (43.3) | 2927 (43.1) | 2726 (43.0) |
| Clerical/support | 1927 (20.8) | 1641 (18.3) | 1523 (17.8) | 1378 (17.2) | 1248 (17.0) | 1125 (16.5) | 1028 (16.2) |
| Marital status | |||||||
| Married/cohabiting | 6894 (74.5) | 6760 (75.4) | 6387 (74.8) | 5947 (74.2) | 5383 (73.1) | 4936 (72.6) | 4508 (71.2) |
| Single | 1509 (16.3) | 1369 (15.3) | 1255 (14.7) | 1136 (14.2) | 1038 (14.1) | 946 (13.9) | 891 (14.1) |
| Divorced | 742 (8.0) | 687 (7.7) | 669 (7.8) | 634 (7.9) | 575 (7.8) | 502 (7.4) | 468 (7.4) |
| Widowed | 111 (1.2) | 156 (1.7) | 228 (2.7) | 297 (3.7) | 367 (5.0) | 411 (6.1) | 467 (7.4) |
| White race/ethnicityc | 8389 (90.6) | ||||||
| Family history | |||||||
| Stroke | 1609 (17.4) | ||||||
| Myocardial infarction | 2492 (26.9) | ||||||
| CVH status, No. of ideal metrics | |||||||
| Low, 0-2d | 2177 (23.5) | 3493 (38.9) | 3402 (39.8) | 3792 (47.3) | 3365 (45.7) | 3387 (49.9) | 2976 (47.0) |
| Moderate, 3-4d | 5690 (61.5) | 4673 (52.1) | 4323 (50.6) | 3623 (45.2) | 3371 (45.8) | 2916 (42.9) | 2735 (43.2) |
| High, 5-7d | 1389 (15.0) | 806 (9.0) | 814 (9.5) | 599 (7.5) | 627 (8.5) | 492 (7.2) | 623 (9.8) |
| No. of ideal metrics, median (IQR)d | 3 (3-4) | 3 (2-4) | 3 (2-4) | 3 (2-3) | 3 (2-4) | 3 (2-3) | 3 (2-4) |
| 14-Point CVH score, median (IQR)e | 9 (7-10) | 8 (7-10) | 8 (7-10) | 8 (7-10) | 8 (7-10) | 8 (7-10) | 9 (7-10) |
Abbreviations: CVH, cardiovascular health; IQR, interquartile range.
Values are reported as No. (%) unless otherwise indicated. Empty table cells indicate variables assessed at baseline only.
Depressive symptoms were ascertained using the 30-item General Health Questionnaire.7
Although variable is termed white/nonwhite, race/ethnicity was self-reported using fixed categories. Those with known ethnicity and categorized as nonwhite were South Asian (56%), black (35.4%), and other (8%).
The cardiovascular health metrics included nonsmoking, body weight, physical activity, diet, blood pressure, fasting blood glucose, and total cholesterol.
The continuous 14-point CVH score (range, 1-14 in the present study; higher score indicating higher CVH) was calculated by assigning 0 (poor), 1 (intermediate), and 2 (ideal) points to each of the 7 metrics (listed in footnote d) and summing them.
Prevalence of Cardiovascular Health Status From 1985/1988 to 2015/2016
The baseline characteristics of the study population and characteristics at each wave are displayed in Table 1, which shows that the sociodemographic profile did not vary across the waves. The prevalence of high cardiovascular health was 15.0% at baseline and ranged from 7.2% to 9.8% thereafter. Participants had a median of 3 ideal metrics at each wave, and this was consistent by age, sex, and race/ethnicity (eFigure 2A-2D in the Supplement). The prevalence of individual cardiovascular health metrics is displayed in eTable 3 in the Supplement.
Time-Varying Cardiovascular Health and Risk of CVD and Mortality
The median follow-up of 29.5 (interquartile range [IQR], 25.2 to 30.4) years for CVD and 30.2 (IQR, 29.6 to 31.1) years for mortality, starting from baseline (1985/1988), yielded 2052 incident CVD events (1757 coronary heart disease events; 295 stroke events) and 1657 deaths (408 from CVD, 748 from cancer, and 501 from other causes). Compared with low cardiovascular health, moderate cardiovascular health (HR, 0.72 [95% CI, 0.66-0.79]) and high cardiovascular health (HR, 0.48 [95% CI, 0.38-0.59]) were associated with a lower risk of CVD (Table 2). Likewise, there was a significant and linear decrease in risk of CVD for each additional time-varying ideal metric (HR, 0.83 [95% CI, 0.80-0.86]) and for each additional point of the 14-point cardiovascular health score (HR, 0.86 [95% CI, 0.84-0.88]) (Table 2). Similar findings were observed for all-cause mortality (Table 2), coronary heart disease and stroke (eTable 4 in the Supplement), and cause-specific mortality (eTable 5 in the Supplement). The incidence rates by categories of cardiovascular health, number of ideal metrics, and level of 14-point cardiovascular health score at baseline are given in Table 3.
Table 2. Time-Varying Cox Proportional Hazard Model for Incident Cardiovascular Disease and All-Cause Mortality.
| CVH Status Adjusted HR (95% CI)a | |||||
|---|---|---|---|---|---|
| No. of Ideal Metricsb | Per Additional Ideal Metricb | Per 1-Point Increase in the 14-Point CVH Scoreb,c | |||
| Low, 0-2 | Moderate, 3-4 | High, 5-7 | |||
| Cardiovascular disease (No./total No.=2052/9256) |
1 [Reference] | 0.72 (0.66-0.79) | 0.48 (0.38-0.59) | 0.83 (0.80-0.86) | 0.86 (0.84-0.88) |
| All-cause mortality (No./total No.=1657/9256) |
1 [Reference] | 0.69 (0.62-0.77) | 0.67 (0.54-0.83) | 0.84 (0.80-0.87) | 0.85 (0.83-0.87) |
Abbreviations: CVH, cardiovascular health; HR, hazard ratio; IQR, interquartile range.
HRs and 95% CIs were estimated by Cox proportional hazard models stratified by year of birth (5-y intervals) and using age as the time scale over a median follow-up of 29.5 (IQR, 25.2-30.4) years for cardiovascular disease and 30.2 (IQR, 29.6-31.1) years for mortality starting from baseline.
CVH status, per additional ideal metric and per 1-point increase in the 14-point CVH score, were included as time-varying variables. HRs were adjusted for sex, race/ethnicity, depression, education, occupation, and family history of cardiovascular disease at baseline. The linearity assumption of the model, per additional ideal metric and per 1-point increase in the 14-point CVH score, was evaluated by comparing the Akaike information criterion of a linear model with a quadratic and a cubic model.
The continuous 14-point CVH score (range, 1-14 in the present study; higher score indicating higher CVH) was calculated by assigning 0 (poor), 1 (intermediate), and 2 (ideal) points to each of the 7 metrics and summing them.
Table 3. Incidence Rates for Cardiovascular Disease and All-Cause Mortality According to Measures of Baseline Cardiovascular Health.
| Incidence Rate per 1000 Person-Years (95% CI)a | ||
|---|---|---|
| Cardiovascular Disease (No./Total No.=2052/9256) |
All-Cause Mortality (No./Total No.=1657/9256) |
|
| CVH status, No. of ideal metrics | ||
| Low, 0-2 | 12.1 (11.2-13.1) | 9.4 (8.7-10.2) |
| Moderate, 3-4 | 8.1 (7.6-8.5) | 5.7 (5.3-6.0) |
| High, 5-7 | 5.0 (4.3-5.7) | 3.6 (3.1-4.3) |
| CVH status per No. of ideal metrics | ||
| 0 | 30.5 (7.6-122) | NA |
| 1 | 16.9 (14.2-20.1) | 13.8 (11.6-16.4) |
| 2 | 11.3 (10.3-12.3) | 8.7 (7.9-9.5) |
| 3 | 9.7 (9.0-10.4) | 6.3 (5.7-6.8) |
| 4 | 6.4 (5.8-7.0) | 5.0 (4.5-5.5) |
| 5 | 4.9 (4.2-5.7) | 3.6 (3.0-4.3) |
| 6 | 5.5 (3.9-7.8) | 4.2 (2.8-6.1) |
| 7 | 4.2 (0.6-29.5) | NA |
| CVH status per points on the 14-point CVH scoreb | ||
| 1 or 2 | 49.2 (20.5-118) | 24.7 (10.3-59.5) |
| 3 or 4 | 20.8 (16.8-25.7) | 17.2 (13.9-21.3) |
| 5 or 6 | 13.5 (12.1-14.9) | 11.6 (10.5-12.9) |
| 7 or 8 | 10.4 (9.7-11.1) | 9.3 (8.7-9.9) |
| 9 or 10 | 6.2 (5.7-6.7) | 5.7 (5.3-6.2) |
| 11 or 12 | 5.1 (4.4-5.9) | 4.8 (4.1-5.6) |
| 13 or 14 | 5.0 (2.4-10.5) | 4.7 (2.2-9.8) |
Abbreviations: CVH, cardiovascular health; IQR, interquartile range; NA, not applicable.
Incidence rates were calculated over a median follow-up of 29.5 (IQR, 25.2-30.4) years for CVD and 30.2 (IQR, 29.6-31.1) years for mortality starting from baseline.
The continuous 14-point CVH score (range, 1-14 in the present study; higher score indicating higher CVH) was calculated by assigning 0 (poor), 1 (intermediate), and 2 (ideal) points to each of the 7 metrics and summing them.
Change in Cardiovascular Health (1985/1988 to 1997/1999)
Change in cardiovascular health was examined and calculated among 6236 individuals. There was a median interval of 11.0 (IQR, 9.1-13.3) years in participants having all 7 metrics at both time points. For 37.8% (n = 2393) of participants with at least 1 missing cardiovascular health metric in 1997/1999, change in cardiovascular health was estimated between 1985/1988 and 1991/1993 (median interval, 5.1 [IQR, 3.8-7.5] years). Overall, change in cardiovascular health status was computed over a median follow-up of 10.4 (IQR, 3.8-13.3) years. The characteristics of individuals included in this analysis, compared with those who died (n = 248), had CVD (n = 468) in the interval, dropped out (n = 924), or had incomplete metrics (n = 1290) are shown in the eTable 6 in the Supplement.
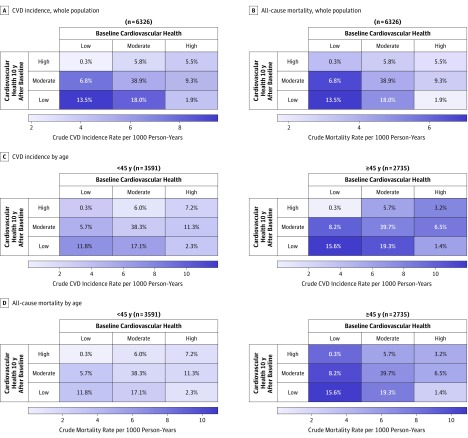
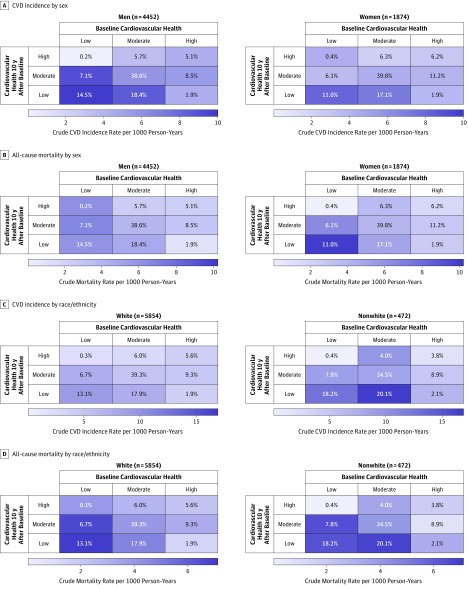
Figure 1A and B and eFigure 3A in the Supplement show that 12.9% (n = 819) of participants improved their cardiovascular health mostly from low to moderate status (6.8%) and from moderate to high status (5.8%), and only 0.3% (n = 19) improved from low to high status. In 57.9% (n = 3660) of participants with stable cardiovascular health, 13.5% had low cardiovascular health, 38.9% had moderate, and 5.5% had high cardiovascular health. In 29.2% (n = 1847) of participants with worse cardiovascular health over time, 18.0% went from moderate to low, 9.3% from high to moderate, and 1.9% from high to low cardiovascular health. Stable moderate cardiovascular health, and initially high cardiovascular health were more prevalent among younger participants (Figure 1C and D and eFigure 3B in the Supplement), in women (Figure 2A and B and eFigure 3C in the Supplement), and in white participants (Figure 2C and D and eFigure 3D in the Supplement). The remaining baseline characteristics of the participants, by patterns of cardiovascular health change, are shown in eTable 7 in the Supplement.
Figure 1. Heatmap of Unadjusted Incidence Rates of CVD and All-Cause Mortality by Patterns of Change in Cardiovascular Health Between 1985/1988 and 1997/1999 in the Total Study Population and in Individuals Younger Than 45 Years vs Aged 45 Years and Older.
Values indicate the percentage of participants in that cardiovascular health category, and colors indicate rate per 1000 person-years. Median follow-up after 1997/1999 was 18.9 (interquartile range [IQR], 17.8-19.3) years for cardiovascular disease (CVD) and 19.7 (IQR, 18.9-19.8) years for mortality. Heatmaps of unadjusted incidence rates of CVD and all-cause mortality for change in the number of ideal health metrics are in eFigure 6.
Figure 2. Heatmap of Unadjusted Incidence Rates of CVD and All-Cause Mortality by Patterns of Change in Cardiovascular Health Between 1985/1988 and 1997/1999 in Women vs Men and in White vs Nonwhite Participants.
Values indicate the percentage of participants in that cardiovascular health category, and colors indicate rate per 1000 person-years. Median follow-up after 1997/1999 was 18.9 (interquartile range [IQR], 17.8-19.3) years for cardiovascular disease (CVD) and 19.7 (IQR, 18.9-19.8) years for mortality. Heatmaps of unadjusted incidence rates of CVD and all-cause mortality for change in the number of ideal health metrics are in eFigure 6. Although variable is termed white/nonwhite, race/ethnicity was self-reported using fixed categories. Those with known ethnicity and categorized as nonwhite were South Asian (56%), black (35.4%), and other (8%).
Change in Cardiovascular Health (1985/1988 to 1997/1999) and Subsequent CVD and Mortality (2017)
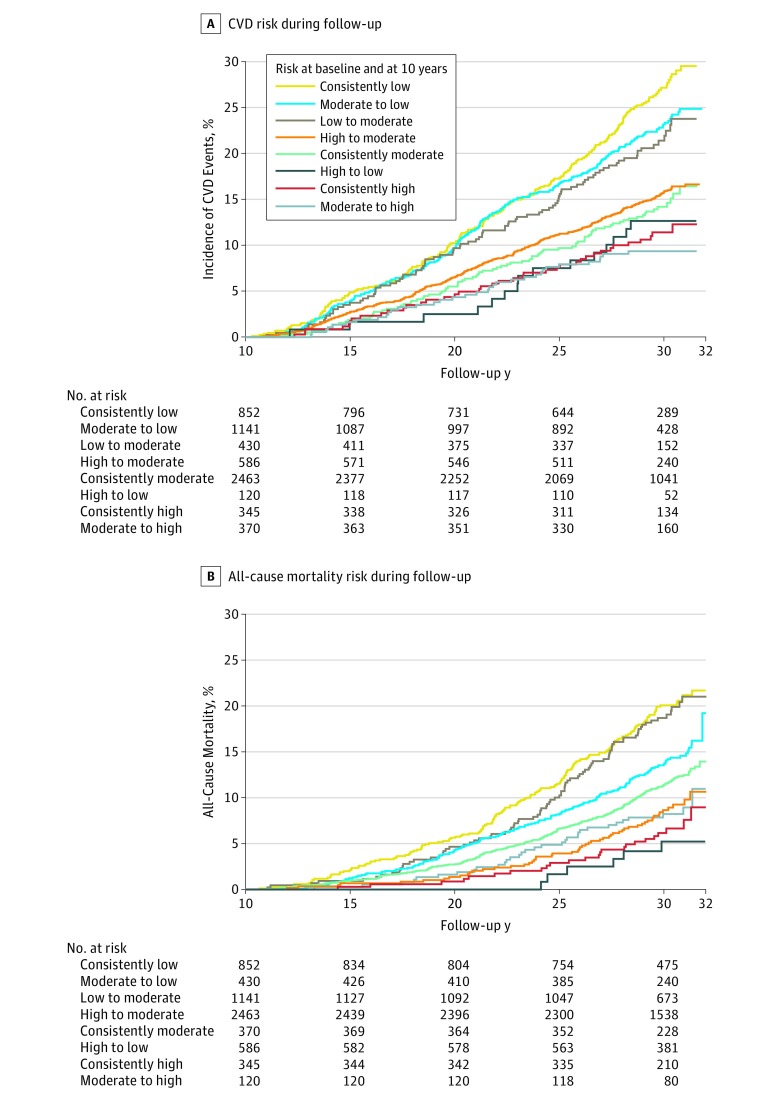
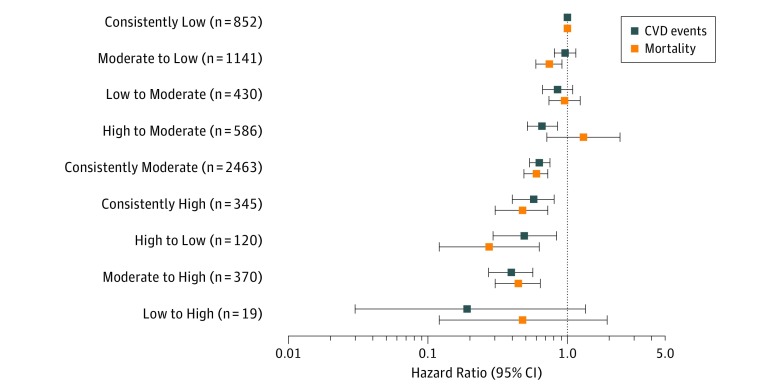
The median follow-up of outcomes starting in 1997/1999 was 18.9 (IQR, 17.8 to 19.3) years for CVD and 19.7 (IQR, 18.9 to 19.8) years for mortality, which resulted in 1114 incident CVD (coronary heart disease and stroke) events and 846 deaths. Heatmaps (Figure 1 and Figure 2) and Kaplan-Meier curves (Figure 3A and B) show the crude incidence rate of CVD and of all-cause mortality by patterns of change in cardiovascular health status. The incidence rates, absolute difference rates, and adjusted HRs for CVD and all-cause mortality are reported in Table 4 and Figure 4. In multivariable analysis, the risk of CVD was not statistically different from that of the consistently low group (reference) in the low to moderate group (absolute rate difference per 1000 person-years, −1.9 [95% CI, −3.9 to 0.1]; HR, 0.84 [95% CI, 0.66-1.08]), the low to high group (absolute rate difference per 1000 person-years, −7.7 [95% CI, −11.5 to −3.9]; HR, 0.19 [95% CI, 0.03-1.35]), and moderate to low group (absolute rate difference per 1000 person-years, −1.3 [95% CI, −3.0 to 0.3]; HR, 0.96 [95% CI, 0.80-1.15]). Instead, the risk of CVD was lower in the consistently moderate group (absolute rate difference per 1000 person-years, −4.2 [95% CI, −5.5 to −2.8]; HR, 0.62 [95% CI, 0.53-0.74]), the moderate to high group (absolute rate difference per 1000 person-years, −6.4 [95% CI, −8.0 to −4.7]; HR, 0.39 [95% CI, 0.27-0.56]), the high to low group (absolute rate difference per 1000 person-years, −5.3 [95% CI, −7.8 to −2.8]; HR, 0.49 [95% CI, 0.29-0.83]), the high to moderate group (absolute rate difference per 1000 person-years, −4.5 [95% CI, −6.2 to −2.9]; HR, 0.66 [95% CI, 0.51-0.85]), and the consistently high group (absolute rate difference per 1000 person-years, −5.6 [95% CI, −7.4 to −3.9]; HR, 0.57 [95% CI, 0.40-0.80]). In addition, there was a significant decrease in CVD risk per unit of change in the number of ideal metrics (HR, 0.83 [95% CI, 0.79-0.88]) and per unit of change in the 14-point cardiovascular health score (HR, 0.87 [95% CI, 0.84-0.90]). The results were similar for all-cause mortality. The distribution of change in the number of ideal health metrics is reported in eFigure 4 in the Supplement, while the adjusted HRs for CVD and all-cause mortality by patterns of change in the number of ideal health metrics are reported in eFigure 5 in the Supplement. The heatmaps of the crude incidence rates of CVD and of all-cause mortality, by patterns of change in the number of ideal cardiovascular health metrics, are reported in eFigure 6 in the Supplement.
Figure 3. Kaplan-Meier Curves of Incident CVD and All-Cause Mortality by Patterns of Change in Cardiovascular Health Between 1985/1988 and 1997/1999.
The follow-up of cardiovascular disease (CVD) and mortality started after 1997/1999, ie, 10 years after the baseline cardiovascular health examination. All individuals with a CVD event within 10 years after the baseline cardiovascular health examination were excluded from this analysis. The median duration of follow-up was 18.9 (interquartile range [IQR],17.8 to 19.3) years for CVD and 19.7 (IQR, 18.9 to 19.8) years for mortality. The low to high group (n = 19) is not reported as only 1 CVD event and 2 deaths occurred during follow-up. Curves are ordered from highest to lowest risk for incident CVD and all-cause mortality.
Table 4. Change in CVH Status Between 1985/1988 and 1997/1999, and Association With Subsequent Incident Cardiovascular Disease and All-Cause Mortality.
| Cardiovascular Disease | All-Cause Mortality | |||||||
|---|---|---|---|---|---|---|---|---|
| No./ Total No. 1114/6326 |
Incidence Rate per 1000 Person-Years (95% CI) | ARD per 1000 Person-Years (95% CI) | Adjusted HR (95% CI)a |
No./ Total No. 846/6326 |
Incidence Rate per 1000 Person-Years (95% CI) | ARD per 1000 Person-Years (95% CI) | Adjusted HR (95% CI)a |
|
| Change in CVH Statusb | ||||||||
| Consistently low | 219/852 | 9.6 (8.4 to 10.9) |
0 | 1 [Reference] | 175/852 | 7.1 (6.1 to 8.2) |
0 | 1 [Reference] |
| Low to moderate | 90/430 | 7.7 (6.2 to 9.4) |
−1.9 (−3.9 to 0.1) |
0.84 (0.66 to 1.08) |
85/430 | 6.8 (5.5 to 8.4) |
−0.3 (−2.1 to 1.5) |
0.94 (0.73 to 1.22) |
| Low to high | 1/19 | 1.9 (0.3 to 13.2) |
−7.7 (−11.5 to −3.9) |
0.19 (0.03 to 1.35) |
2/19 | 3.6 (0.9 to 14.3) |
−3.5 (−8.6 to 1.5) |
0.47 (0.12 to 1.91) |
| Moderate to low | 257/1141 | 8.2 (7.3 to 9.3) |
−1.3 (−3.0 to 0.3) |
0.96 (0.80 to 1.15) |
167/1141 | 5.0 (4.3 to 5.8) |
−2.1 (−3.4 to −0.8) |
0.73 (0.59 to 0.90) |
| Consistently moderate | 375/2463 | 5.4 (4.9 to 6.0) |
−4.2 (−5.5 to −2.8) |
0.62 (0.53 to 0.74) |
300/2463 | 4.1 (3.7 to 4.6) |
−3.0 (−4.1 to −1.8) |
0.59 (0.49 to 0.72) |
| Moderate to high | 34/370 | 3.2 (2.3 to 4.4) |
−6.4 (−8.0 to −4.7) |
0.39 (0.27 to 0.56) |
33/370 | 3.0 (2.1 to 4.2) |
−4.1 (−5.6 to −2.7) |
0.44 (0.30 to 0.64) |
| High to low | 15/120 | 4.3 (2.6 to 7.1) |
−5.3 (−7.8 to −2.8) |
0.49 (0.29 to 0.83) |
6/120 | 1.7 (0.7 to 3.7) |
−5.4 (−7.1 to −3.8) |
0.27 (0.12 to 0.62) |
| High to moderate | 84/586 | 5.0 (4.1 to 6.2) |
−4.5 (−6.2 to −2.9) |
0.66 (0.51 to 0.85) |
54/586 | 3.1 (2.4 to 4.0) |
−4.0 (−5.3 to −2.7) |
0.51 (0.38 to 0.70) |
| Consistently high | 39/345 | 3.9 (2.9 to 5.4) |
−5.6 (−7.4 to −3.9) |
0.57 (0.40 to 0.80) |
24/345 | 2.3 (1.6 to 3.5) |
−4.8 (−6.2 to −3.4) |
0.47 (0.30 to 0.72) |
| Change in No. of Ideal Metricsc | ||||||||
| Per 1 additional ideal metric | 0.83 (0.79 to 0.88) |
0.92 (0.86 to 0.98) |
||||||
| Lost 3, 4, or 5 ideal metrics | 45/224 | 7.1 (5.3 to 9.5) |
0.7 (−1.4 to 2.9) |
1.86 (1.34 to 2.58) |
20/224 | 3.0 (1.9 to 4.6) |
−1.6 (−3.0 to −0.2) |
1.21 (0.75 to 1.93) |
| Lost 2 ideal metrics | 150/764 | 7.0 (6.0 to 8.3) |
0.7 (−0.6 to 2.0) |
1.52 (1.25 to 1.86) |
100/764 | 4.4 (3.6 to 5.4) |
−0.2 (−1.2 to 0.8) |
1.36 (1.07 to 1.72) |
| Lost 1 ideal metric | 314/1792 | 6.3 (5.6 to 7.0) |
−0.1 (−1.0 to 0.9) |
1.15 (0.99 to 1.33) |
234/1792 | 4.4 (3.9 to 5.0) |
−0.2 (−0.9 to 0.6) |
1.13 (0.95 to 1.34) |
| 0 Ideal metrics (no change) | 396/2219 | 6.4 (5.8 to 7.0) |
0 | 1 [Reference] | 302/2219 | 4.6 (4.1 to 5.1) |
0 | 1 [Reference] |
| Gained 1 ideal metric | 163/1039 | 5.6 (4.8 to 6.5) |
−0.8 (−1.9 to 0.3) |
0.82 (0.68 to 0.98) |
144/1039 | 4.7 (4.0 to 5.5) |
0.1 (−0.8 to 1.0) |
0.94 (0.77 to 1.14) |
| Gained 2 ideal metrics | 44/249 | 6.4 (4.7 to 8.5) |
−0.0 (−2.0 to 1.9) |
0.90 (0.66 to 1.24) |
42/249 | 5.7 (4.2 to 7.7) |
1.1 (−0.7 to 2.9) |
1.09 (0.79 to 1.51) |
| Gained 3 or 4 ideal metrics | 2/39 | 1.8 (0.5 to 7.2) |
−4.6 (−7.2 to −2.0) |
0.21 (0.05 to 0.84) |
4/39 | 3.5 (1.3 to 9.2) |
−1.1 (−4.6 to 2.3) |
0.55 (0.20 to 1.48) |
| Change in 14-Point CVH Scored | ||||||||
| Per 1-point increase in scoree | 0.87 (0.84 to 0.90) |
0.91 (0.87 to 0.95) |
||||||
| Lost 5, 6, or 7 points | 13/41 | 11.6 (6.7 to 20.0) |
5.7 (−0.7 to 12.1) |
3.23 (1.83 to 5.69) |
7/41 | 5.8 (2.8 to 12.2) |
1.4 (−3.0 to 5.7) |
2.16 (1.01 to 4.62) |
| Lost 3 or 4 points | 75/403 | 6.7 (5.4 to 8.4) |
0.8 (−0.9 to 2.5) |
1.51 (1.16 to 1.96) |
58/403 | 4.9 (3.8 to 6.3) |
0.4 (−1.0 to 1.8) |
1.59 (1.18 to 2.14) |
| Lost 1 or 2 points | 391/1979 | 7.1 (6.4 to 7.9) |
1.2 (0.2 to 2.2) |
1.33 (1.14 to 1.57) |
249/1979 | 4.2 (3.7 to 4.8) |
−0.2 (−1.0 to 0.6) |
1.09 (0.90 to 1.31) |
| No change in score | 250/1508 | 5.9 (5.2 to 6.7) |
0 | 1 [Reference] | 199/1508 | 4.5 (3.9 to 5.1) |
0 | 1 [Reference] |
| Gained 1 or 2 points | 322/2040 | 5.6 (5.0 to 6.2) |
−0.3 (−1.3 to 0.6) |
0.83 (0.70 to 0.98) |
272/2040 | 4.5 (4.0 to 5.1) |
0.0 (−0.8 to 0.9) |
0.89 (0.74 to 1.07) |
| Gained 3 or 4 points | 59/332 | 6.4 (5.0 to 8.3) |
0.5 (−1.3 to 2.3) |
0.81 (0.61 to 1.08) |
56/332 | 5.8 (4.4 to 7.5) |
1.3 (−0.3 to 2.9) |
0.92 (0.68 to 1.24) |
| Gained 5 or 6 points | 4/23 | 6.6 (2.5 to 17.6) |
0.7 (−5.8 to 7.2) |
0.58 (0.22 to 1.58) |
5/23 | 8.0 (3.3 to 19.2) |
3.5 (−3.5 to 11.0) |
0.77 (0.31 to 1.89) |
Abbreviations: ARD, absolute rate difference; CVH, cardiovascular health; HR, hazard ratio; IQR, interquartile range.
Estimated by Cox proportional hazard model stratified by year of birth (5-y intervals) and using age as the time scale on a subsequent median follow-up time of 18.9 (IQR, 17.8 to 19.3) years for CVD events and 19.7 (IQR, 18.9 to 19.8) years for all-cause mortality. HRs were adjusted for sex, race/ethnicity, depression, education, occupation, and family history of cardiovascular disease at baseline. HRs for change in number of ideal metrics or change in 14-point CVH score were additionally adjusted for baseline number of ideal metrics and CVH score. The linearity assumption of the model, l per additional ideal metric and per 1-point increase in the 14-point CVH score, was evaluated by comparing the Akaike information criterion of a linear model with a quadratic and a cubic model.
Calculated using the consistently low group as the reference.
For calculation of HRs and absolute rate differences, participants with same number of ideal metrics between baseline and 1997/1999 (no change, ie, difference in the number of ideal metrics = 0) are the reference group. Change in number of ideal metrics (range, −5 to +4).
Change in 14-point CVH score (range, −7 to +6).
CVH score (range, 1-14 in the present study; higher score indicates higher CVH) was calculated by assigning 0 (poor), 1 (intermediate), and 2 points for ideal metrics. Those with the same score (baseline-1997/1999 [no change, ie, difference in the score = 0]) were the reference group.
Figure 4. Hazard Ratios of CVD and All-Cause Mortality by Pattern of Change in the Cardiovascular Health Status Between 1985/1988 and 1997/1999.
Hazard ratios (HRs) and 95% CIs (indicated by error bars) were estimated by Cox proportional hazard model stratified by year of birth (5-y intervals) and using age as the time scale. The median follow-up time after 1997/1999 was 18.9 (interquartile range [IQR], 17.8 to 19.3) years for cardiovascular disease (CVD) and 19.7 (IQR, 18.9 to 19.8) years for mortality. The consistently low group served as the reference category. Results are adjusted for sex, race/ethnicity, depression, education, occupation, and family history of CVD at baseline. HRs are ordered from highest to lowest risk for incident CVD compared with the reference category.
Sensitivity Analyses
The results with 4 groups of change in cardiovascular health score showed that compared with the consistently low group, those with high to low, low to high, and consistently high cardiovascular health had a lower CVD and mortality risk (eTable 8 in the Supplement). Multiple imputations to account for missing cardiovascular health metrics and covariates in either the time-varying analysis (eTable 9 in the Supplement) or the analysis of change in cardiovascular health (eTable 10 in the Supplement) provided results that were consistent with those obtained in the main analyses. The results for the individual cardiovascular health metrics are given in eTable 11, eTable 12, and eTable 13 in the Supplement. Post hoc analyses that excluded depression as a covariate showed minimal differences in findings.
Discussion
In this study, time-varying moderate and high measures of cardiovascular health were associated with a lower CVD risk compared with low cardiovascular health. However, there was no consistent relationship between the direction of change in category of cardiovascular health and risk of CVD.
Few previous studies have documented changes in the prevalence of cardiovascular health. Using a metric approach, the National Health and Nutrition Examination Surveys (NHANES)15 showed significant decrease in the prevalence of smoking, hypercholesterolemia, and hypertension, but showed a significant increase in obesity and diabetes; whereas levels of diet and physical activity were unchanged from 1988/1994 to 2008. In the Atherosclerosis Risk in Communities (ARIC) study,16 the general trend was a decrease in the number of ideal metrics, and only 7% of participants improved their cardiovascular health over 26 years from 1987 to 2013. The present study extends the results of these studies conducted in US participants to a UK population and found that 13% of participants improved their cardiovascular health. This is almost 2 times higher than in the ARIC study. The shorter follow-up (10 vs 26 years), younger age (30-55 years vs 45-65 years), the less ethnically diverse population, and the higher socioeconomic background in the Whitehall II study, as compared with ARIC, may contribute to these differences. In accordance with NHANES and ARIC, the present study found that patterns of cardiovascular health change differed according to age, sex, and race/ethnicity.
One previous study, the Framingham Offspring study, evaluated change in cardiovascular health with incident CVD and mortality.4 Using a 14-point cardiovascular health scale, this study defined low cardiovascular health (score of <8) and high cardiovascular health (score of ≥8) and found that individuals who remained in low cardiovascular health or changed from low to high or high to low cardiovascular health between baseline and a follow-up examination 10 to 17 years later had a higher CVD risk as compared with individuals with persistently high cardiovascular health over time. When this analysis was repeated in the present study, similar results were found. However, the present study evaluated cardiovascular health change with greater precision (9 groups and continuous measures of cardiovascular health change vs 4 groups of cardiovascular health change), had a greater sample size (n = 6326 vs n = 3460), and had a longer follow-up duration for events (median, 18.9 and 19.7 years vs 5.1 years). In addition, 3 prior studies correlated change in cardiovascular health with intermediate end points. The Cardiovascular Risk in Young Finns study17 (participants aged 9-24 years) showed that an increase in the number of ideal metrics over 20 years was related to a lower prevalence of arterial stiffness, independent of the baseline number of ideal metrics. In ARIC,16 improvement in cardiovascular health over 26 years of follow-up was associated with lower prevalence of CVD (no data on incident CVD) and better cardiac structure and function. In addition, in the Framingham Heart study,18 loss of ideal cardiovascular health metrics over 6 years was not statistically significantly associated with coronary artery calcification progression after adjustment for the number of baseline ideal metrics.
The inconsistent relationship between the direction of change in category of cardiovascular health and CVD risk in the present study may be explained by a number of reasons. First, there may be truly no relationship between change in categories of cardiovascular health and incident CVD, and the observed inconsistencies may represent random distributions of outcomes.
Second, the concept of cardiovascular health metrics may not be useful to study change in cardiovascular risk factors over time, ie, any causal relationships between cardiovascular risk factors and CVD may be more complex than can be captured with a relatively simple, categorical metric.
Third, given that the causal network for CVD is complex, there may be a large amount of unmeasured confounding and mediating embedded within the data in this study.
Fourth, prognosis may be determined primarily by early high cardiovascular health, which may explain that participants who changed from high cardiovascular health to a lower category had a relatively low CVD risk as compared with the other groups of change.
Limitations
This study has several limitations. First, the observational design precludes reaching causal conclusions about the findings.
Second, individuals excluded from the analysis of change in cardiovascular health had a less favorable cardiovascular risk profile, which may have led to an underestimation of the reported associations.
Third, some categories of cardiovascular health change were small in size, potentially explaining that some associations did not reach statistical significance (eg, only 19 participants improved from low to high cardiovascular health).
Fourth, changes in the distribution of cardiovascular health across repeated examinations might have partly been explained by aging, temporal trends, and cohort attrition.
Fifth, the Whitehall II study is based on government employees, which raises the issue of healthy worker effect; it is also mostly composed of white participants, and findings might not apply to other race/ethnicity groups.
Conclusions
Among a group of participants without CVD who received follow-up over a median 18.9 years, there was no consistent relationship between direction of change in category of a composite metric of cardiovascular health and risk of CVD.
eTable 1. Definition of Cardiovascular Health Metrics According to the American Heart Association for Ascertainment of Cardiovascular Health Status
eTable 2. Characteristics of Excluded and Included Study Participants at Baseline in 1985/88
eTable 3. Prevalence of Individual Cardiovascular Health Metrics at Each Wave of Examination From 1985/88 up to 2015/2016
eTable 4. Time-Varying Cox Proportional Hazard Model for Incident Coronary Heart Disease and Stroke as Separate Outcomes
eTable 5. Time-Varying Cox Proportional Hazard Model for Cause-Specific Mortality (Competing Risk Analysis)
eTable 6. Baseline Characteristics of Included and Excluded Study Participants for the Analysis of the Change in Cardiovascular Health Between 1985/88 and 1997/99
eTable 7. Baseline Characteristics by Pattern of Change in Cardiovascular Health
eTable 8. Associations Between 4 Groups of Cardiovascular Health Change as Defined in the Framingham Offspring Study and Incident Cardiovascular Disease and All-Cause Mortality
eTable 9. Time-Varying Cox Proportional Hazard Model for Incident Cardiovascular Disease and All-Cause Mortality – Results Using Multiple Imputations to Account for Missing Values
eTable 10. Change in Cardiovascular Health Status Between 1985/88 and 1997/99 and Association With Subsequent Incident Cardiovascular Disease and All-Cause Mortality – Results Using Multiple Imputations to Account for Missing Values
eTable 11. Change in the Level of Individual Cardiovascular Health Metrics Between 1985/88 and 1997/99
eTable 12. Time-Varying Cox Proportional Hazard Models for the Association Between Individual Cardiovascular Health Metrics and Incident Cardiovascular Disease and All-Cause Mortality
eTable 13. Association of Change in the Individual Cardiovascular Health Metrics Between 1985/88 and 1997/99 With Subsequent Incident Cardiovascular Disease Events and All-Cause Mortality
eFigure 1. Summary of the Statistical Analysis Design
eFigure 2. Distribution of the Number of Ideal Cardiovascular Health Metrics at Each Wave in the Total Study Population (A), by Age Group (B), by Sex (C) and in White Versus Nonwhite Participants (D)
eFigure 3. Distribution of the Change in Cardiovascular Health Between 1985/88 and 1997/99 in the Total Study Population (n=6326) (A), in Individuals Aged <45 (n=3591) and ≥45 Years (n=2735) (B), in Women (n=1874) and Men (n=4452) (C) and in White (n=5854) Versus Nonwhite Participants (n=472) (D)
eFigure 4. Distribution of the Change in the Number of Ideal Cardiovascular Health Metrics Between 1985/88 and 1997/99 in the Total Study Population (n=6326) (A), in Individuals Aged <45 (n=3591) and ≥45 Years (n=2735) (B), in Women (n=1874) and Men (n=4452) (C) and in White (n=5854) Versus Nonwhite Participants (n=472) (D)
eFigure 5. Hazards Ratios of Incident Cardiovascular Disease and All-Cause Mortality for Change in the Number of Ideal Cardiovascular Health Metrics Between 1985/88 and 1997/99
eFigure 6. Heatmap of Unadjusted Incidence Rates of Cardiovascular Disease (A) and All-Cause Mortality (B) by Change in the Number of Ideal Health Metrics Between 1985/88 and 1997/99 in the Total Study Population
References
- 1.Lloyd-Jones DM, Hong Y, Labarthe D, et al. ; American Heart Association Strategic Planning Task Force and Statistics Committee . Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586-613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 2.Guo L, Zhang S. Association between ideal cardiovascular health metrics and risk of cardiovascular events or mortality: a meta-analysis of prospective studies. Clin Cardiol. 2017;40(12):1339-1346. doi: 10.1002/clc.22836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaye B, Canonico M, Perier MC, et al. Ideal cardiovascular health, mortality, and vascular events in elderly subjects: theThree-City Study. J Am Coll Cardiol. 2017;69(25):3015-3026. doi: 10.1016/j.jacc.2017.05.011 [DOI] [PubMed] [Google Scholar]
- 4.Enserro DM, Vasan RS, Xanthakis V. Twenty-year trends in the American Heart Association cardiovascular health score and impact on subclinical and clinical cardiovascular disease: the Framingham Offspring Study. J Am Heart Assoc. 2018;7(11):e008741. doi: 10.1161/JAHA.118.008741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeboah J. Road to the American Heart Association 2020 impact goals: the metric for monitoring progress. Circ Cardiovasc Imaging. 2018;11(1):e007385. doi: 10.1161/CIRCIMAGING.117.007385 [DOI] [PubMed] [Google Scholar]
- 6.Marmot MG, Smith GD, Stansfeld S, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337(8754):1387-1393. doi: 10.1016/0140-6736(91)93068-K [DOI] [PubMed] [Google Scholar]
- 7.Stansfeld SA, Marmot MG. Social class and minor psychiatric disorder in British civil servants: a validated screening survey using the General Health Questionnaire. Psychol Med. 1992;22(3):739-749. doi: 10.1017/S0033291700038186 [DOI] [PubMed] [Google Scholar]
- 8.Kivimäki M, Batty GD, Hamer M, et al. Using additional information on working hours to predict coronary heart disease: a cohort study. Ann Intern Med. 2011;154(7):457-463. doi: 10.7326/0003-4819-154-7-201104050-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kivimäki M, Batty GD, Singh-Manoux A, Britton A, Brunner EJ, Shipley MJ. Validity of cardiovascular disease event ascertainment using linkage to UK hospital records. Epidemiology. 2017;28(5):735-739. doi: 10.1097/EDE.0000000000000688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Britton A, Milne B, Butler T, et al. Validating self-reported strokes in a longitudinal UK cohort study (Whitehall II): extracting information from hospital medical records versus the Hospital Episode Statistics database. BMC Med Res Methodol. 2012;12:83. doi: 10.1186/1471-2288-12-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of competing risks in survival analysis. J Am Stat Assoc. 1999;94:496-509. doi: 10.1080/01621459.1999.10474144 [DOI] [Google Scholar]
- 12.Gaye B, Prugger C, Perier MC, et al. High level of depressive symptoms as a barrier to reach an ideal cardiovascular health: the Paris Prospective Study III. Sci Rep. 2016;6:18951. doi: 10.1038/srep18951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kronish IM, Carson AP, Davidson KW, Muntner P, Safford MM. Depressive symptoms and cardiovascular health by the American Heart Association’s definition in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. PLoS One. 2012;7(12):e52771. doi: 10.1371/journal.pone.0052771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27(23):2763-2774. doi: 10.1093/eurheartj/ehl338 [DOI] [PubMed] [Google Scholar]
- 15.Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM. Cardiovascular health behavior and health factor changes (1988-2008) and projections to 2020: results from the National Health and Nutrition Examination Surveys. Circulation. 2012;125(21):2595-2602. doi: 10.1161/CIRCULATIONAHA.111.070722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah AM, Claggett B, Folsom AR, et al. Ideal Cardiovascular health during adult life and cardiovascular structure and function among the elderly. Circulation. 2015;132(21):1979-1989. doi: 10.1161/CIRCULATIONAHA.115.017882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aatola H, Hutri-Kähönen N, Juonala M, et al. Prospective relationship of change in ideal cardiovascular health status and arterial stiffness: the Cardiovascular Risk in Young Finns Study. J Am Heart Assoc. 2014;3(2):e000532. doi: 10.1161/JAHA.113.000532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hwang SJ, Onuma O, Massaro JM, et al. Maintenance of ideal cardiovascular health and coronary artery calcium progression in low-risk men and women in the Framingham Heart Study. Circ Cardiovasc Imaging. 2018;11(1):e006209. doi: 10.1161/CIRCIMAGING.117.006209 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Definition of Cardiovascular Health Metrics According to the American Heart Association for Ascertainment of Cardiovascular Health Status
eTable 2. Characteristics of Excluded and Included Study Participants at Baseline in 1985/88
eTable 3. Prevalence of Individual Cardiovascular Health Metrics at Each Wave of Examination From 1985/88 up to 2015/2016
eTable 4. Time-Varying Cox Proportional Hazard Model for Incident Coronary Heart Disease and Stroke as Separate Outcomes
eTable 5. Time-Varying Cox Proportional Hazard Model for Cause-Specific Mortality (Competing Risk Analysis)
eTable 6. Baseline Characteristics of Included and Excluded Study Participants for the Analysis of the Change in Cardiovascular Health Between 1985/88 and 1997/99
eTable 7. Baseline Characteristics by Pattern of Change in Cardiovascular Health
eTable 8. Associations Between 4 Groups of Cardiovascular Health Change as Defined in the Framingham Offspring Study and Incident Cardiovascular Disease and All-Cause Mortality
eTable 9. Time-Varying Cox Proportional Hazard Model for Incident Cardiovascular Disease and All-Cause Mortality – Results Using Multiple Imputations to Account for Missing Values
eTable 10. Change in Cardiovascular Health Status Between 1985/88 and 1997/99 and Association With Subsequent Incident Cardiovascular Disease and All-Cause Mortality – Results Using Multiple Imputations to Account for Missing Values
eTable 11. Change in the Level of Individual Cardiovascular Health Metrics Between 1985/88 and 1997/99
eTable 12. Time-Varying Cox Proportional Hazard Models for the Association Between Individual Cardiovascular Health Metrics and Incident Cardiovascular Disease and All-Cause Mortality
eTable 13. Association of Change in the Individual Cardiovascular Health Metrics Between 1985/88 and 1997/99 With Subsequent Incident Cardiovascular Disease Events and All-Cause Mortality
eFigure 1. Summary of the Statistical Analysis Design
eFigure 2. Distribution of the Number of Ideal Cardiovascular Health Metrics at Each Wave in the Total Study Population (A), by Age Group (B), by Sex (C) and in White Versus Nonwhite Participants (D)
eFigure 3. Distribution of the Change in Cardiovascular Health Between 1985/88 and 1997/99 in the Total Study Population (n=6326) (A), in Individuals Aged <45 (n=3591) and ≥45 Years (n=2735) (B), in Women (n=1874) and Men (n=4452) (C) and in White (n=5854) Versus Nonwhite Participants (n=472) (D)
eFigure 4. Distribution of the Change in the Number of Ideal Cardiovascular Health Metrics Between 1985/88 and 1997/99 in the Total Study Population (n=6326) (A), in Individuals Aged <45 (n=3591) and ≥45 Years (n=2735) (B), in Women (n=1874) and Men (n=4452) (C) and in White (n=5854) Versus Nonwhite Participants (n=472) (D)
eFigure 5. Hazards Ratios of Incident Cardiovascular Disease and All-Cause Mortality for Change in the Number of Ideal Cardiovascular Health Metrics Between 1985/88 and 1997/99
eFigure 6. Heatmap of Unadjusted Incidence Rates of Cardiovascular Disease (A) and All-Cause Mortality (B) by Change in the Number of Ideal Health Metrics Between 1985/88 and 1997/99 in the Total Study Population