Figure 3: Mechanisms and consequences of age-related vascular inflammation.
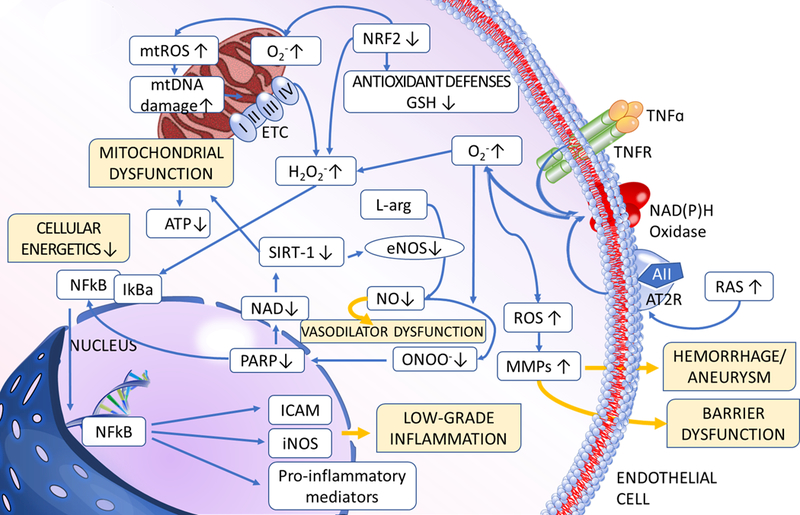
The model predicts that multiple pathways converge on activation of inflammatory processes in the vascular tissue. During aging increased ROS production, exacerbated by Nrf2 dysfunction, enhances NF-κB activation, which promotes inflammatory cytokine and chemokine expression, microvascular endothelial activation, leukocyte adhesion and extravasation. Increased nitrative stress promotes PARP1 activation, which contributes to impaired activity of anti-inflammatory sirtuins. Sterile inflammation in the vascular wall is also exacerbated by increased secretion of inflammatory mediators from senescent cells and danger-associated molecular patterns (DAMPs), which activate innate immune system effectors, including toll-like receptors (TLRs) and the NLRP3 inflammasome complex. The aging vasculature in humans is also affected by the high prevalence of endothelium-trophic persistent cytomegalovirus (CMV) infection. Inflammatory processes contribute to a wide range of macro- and micro-vascular pathologies affecting older people.
